Links: Basic Info & Vitamin Use: Benefits/Risks | Common Vitamin Supplements & Aluminum | Ascorbic Acid (Vit-C) | Vitamin A | Thiamine (B1) | Riboflavin (B2) | Niacin (B3) | Pyridoxine (B6) | Vit B-12 | Biotin | Calcium | Co-Q10 | Creatine | L-Carnitine | Chromium | Chloride | Cobalt | Copper | Vit-D | Fatty Acids | Vit-E | Fluoride | Folic Acid | Iodine | Iron | Vit-K | Magnesium | Manganese | Molybdenum | Pantothenic Acid | Phosphorus | Protein | Potassium | Selenium | Sodium | Sulfur, Strontium & Vandium | Zinc | Trace Elements | Signs of Deficiencies | Vitamin Toxicity | Basic Nutrients and Special Diets | Omega-3 | See Nutriceuticals (Herbal) | Antioxidants | Healthy Living | Basic Dietary Building Blocks (Protein, Carb, Fat, Veges/ Fiber, Dairy, Water, Salt etc) |
Vitamins are a number of organic compounds that are essential for normal metabolism. All vitamins (with the exception of Vit-D) cannot be synthesized by humans, thus they need to be ingested in the diet to prevent d/o’s of metabolism. If one is unable to attain the optimal diet with >5 servings of vegetables and fruits per day, or if age >65 or pregnant or with a chronic disease, it may be worth taking a generic multivitamins as they are inexpensive and safe.
Vitamin Supplementation: The USPSTF does not recommend routine vitamin supplementation because multiple large trials have failed to demonstrate benefits of vitamin A, C, or E against heart disease or cancer. Two studies suggested that beta-carotene may increase risk of lung cancer in smokers (see below).
• A survey of 12,000 U.S. adults found that half use dietary supplement (at a total cost of about US$30 billion annually) (JAMA Intern Med 2013:Feb 4;e-pub ahead of print)……The most common motivations for supplement use were to improve overall health (45%), maintain health (33%), improve bone health (25%), and “get more energy” (11%). The most commonly used supplements were multivitamins (31%), calcium (12%), and {omega}-3 fatty acids or fish oil (10%). Participants reported that only about a quarter of supplement use was recommended by healthcare professionals.
• Taking a daily multivitamin x 11.2 years does not reduce the risk for major cardiovascular events in men according to data on 14,641 men from the Physicians’ Health Study II (JAMA. 2012;308:1751-1760)…..multivitamins are the most common supplement taken by US adults….Individuals who believe they are deriving benefits from supplements may be less likely to engage in other preventive health behaviors, and chronic use of daily supplements poses a financial burden, with annual vitamin supplement sales in the billions of US dollars.
• Taking vitamins and antioxidants does not prevent major adverse cardiovascular events according to data from data from 50 randomized, controlled trials that involved 295,000 participants (BMJ 2013;346:f10)……supplemental vitamins and antioxidants had no effect on risk for CV-related death, myocardial infarction, angina, stroke, sudden cardiac death, or transient ischemic attack. …..”There is no evidence to support the use of vitamin or antioxidant supplements in the prevention of cardiovascular disease.”
• Short-term folic acid supplementation (2mg qd) had no effect on cancer incidence (Lancet 2013:Jan 25;e-pub ahead of print).
Multivitamins May Be Harmful: In women aged 55 to 69 years, several widely used dietary vitamin and mineral supplements, especially supplemental iron or copper,, may be associated with increased risk for death, according to data from 38,772 participants in the Iowa Women’s Health Study (mean age at baseline, 62) (Arch Intern Med. 2011;171:1625-1634)….several vitamin supplements were associated with a higher risk for total mortality, including multivitamins, vitamins B6, and folic acid, as well as minerals iron, magnesium, zinc, and copper……Vitamin B6, folic acid, iron, magnesium, and zinc were associated with about a 3% to 6% increased risk for death, whereas copper was associated with an 18.0% increased risk for total mortality when compared with corresponding nonuse…..In contrast, use of calcium was inversely related to risk for death (hazard ratio, 0.91; 95% confidence interval, 0.88 – 0.94; absolute risk reduction, 3.8%)……..with the exception of calcium, supplement use was not associated with lower risk for cancer-related, cardiovascular, or all-cause death……caution regarding use of dietary supplements by well-nourished individuals seems warranted and makes biological sense.
• Vitamins are often taken by the people who need them least a study suggests (Am J Clin Nutr 2011;online September 28)…..people who take mineral supplements also tend to get more nutrients from their food than those who don’t take supplements……supplement users may be getting too much of a good thing by overloading on minerals, such as iron, that can cause potentially serious health problems, researchers said…..Supplement users also were more likely to boost their intake of magnesium and zinc above recommended upper limits.
Notes: All brands of multivitamins are quite similar, there is no evidence of bioavailability differences because of the formulation (Vitamins for chronic disease prevention in adults. JAMA 2002;287:3127-9). Blood tests for many vitamins are widely available, but there is no need to tailor supplements to individual needs, as there is insufficient information about the optimum blood levels of vitamins (difficult to interpret subtle deficiency states).
• In a systematic review and meta-analysis of eight RCT’s found that those >65yo who take vitamin and mineral supplements had significantly fewer days of infection yearly (mean, 17.5 days/year) than did placebo recipients (BMJ 2005;330(April 16):871-4).
• The evidence for routine use of multivitamin and mineral supplements to reduce infections in elderly people is weak and conflicting (BMJ. 2005 Mar 31;Epub).
• Multivitamin and multimineral supplementation x1 year did not affect morbidity in 910 community dwelling pt’s >65yo (BMJ. 2005;331:304-305, 324-327).
• Low-dose antioxidant vitamin and mineral supplementation lowers all-cause mortality in men (RR 0.69) but not in women (RR 1.04), according a RCT (Arch Intern Med. 2004;164:2335-2342) (120 mg of ascorbic acid, 30 mg of Vit-E, 6 mg of beta carotene, 100 µg of selenium, and 20 mg of zinc qd). Routine vitamin and mineral supplementation neither prevented infection nor reduced emergency department and hospital visits in 763 elderly nursing home pt’s (mean age, 85)(J Am Geriatr Soc 2007;55:35-42). A meta-analysis of 47 studies with high-quality methodology (180,000 pt’s) found recipients of supplements (beta carotene, vitamin A, and vitamin E) had increased all-cause mortality compared with controls (RR 1.05) (JAMA. 2007;297:842-857) (Vit-C and selenium had no significant effect on mortality). Higher vitamin intake from diet and supplements is unlikely to reduce pneumonia risk in well nourished women (Am J Med 2007;120:330-336).
• The NIH found that there is insufficient evidence regarding multivitamin/mineral supplements and cancer or chronic disease prevention (Ann Intern Med 2006;145:364-71, 372-85)…they did recommend: Smokers should avoid beta-carotene, based on evidence that it increased the incidence of lung cancer and of death. Calcium and Vit-D can improve bone-mineral density and reduce fx risk in postmenopausal women.
Results of single studies and examination of secondary outcomes suggest that:
(1) selenium may reduce risk for prostate, lung, and colorectal cancer;
(2) vitamin E may reduce risk for heart disease in women and prostate cancer in male smokers;
(3) vitamin A and zinc may decrease stomach cancer risk;
(4) vitamin C, vitamin E, beta-carotene, and zinc may prevent progression of age-related macular degeneration.
A large prospective study, concludes that regular multivitamin use has no effect on the risk for prostate cancer, but that men with high intakes (> 7 times per week) have more than double the risk for advanced and fatal prostate cancer compared with never users (J Natl Cancer Inst. 2007;99:754-764)…. Heavy multivitamin use is not associated with increased risk unless selenium, folate, or vitamin E supplements were also used.
• For postmenopausal women, taking multivitamins won’t lower the risk of developing serious disease according to data from 161,808 women in the Women’s Health Initiative study (Arch Intern Med 2009;169(3):294-304)….the use of multivitamins had no effect on cancer or cardiovascular disease risk for postmenopausal women…… multivitamins that purport to work against stress (high doses of folic acid and other B vitamins) were the only supplements that had a protective association with cardiovascular disease (HR 0.75 for myocardial infarction).
• Vitamins C (500 mg) and E (400 IU) were found to provide no CVD benefit in low-risk men according to an 8 year RCT with 14,641 male physicians (mean age, 64)(The Physicians’ Health Study II. JAMA 2008;300:2123)……A near doubling in risk for hemorrhagic stroke was observed in the vitamin E groups, although the change in absolute risk was small (39 vs. 23 events).
• Multivitamin supplements did not affect CVD risk, cancer risk, or overall mortality in Women’s Health Initiative (WHI) participants (Arch Intern Med 2009;169:294)…..41.5% of the women reported using multivitamins, most commonly with minerals (35%)……Multivitamin users were significantly more likely to be white, to live in the western U.S., to have lower BMIs, to be more physically active, to have college degrees, to be nonsmokers, and to drink alcohol than were nonusers. …editorialist notes that “we still lack adequate evidence to recommend for or against multivitamins”.
• A study found that exercise promotes health, but vitamins C and E block this benefit (Proc Natl Acad Sci U S A 2009;106:8665)……All participants were randomized to receive placebo or vitamin E (400 IU/day) plus vitamin C (500 mg twice daily) and underwent an exercise regimen for 4 weeks (5 days/week: biking or running, 20 minutes; circuit training, 45 minutes; warm-up/cool-down, 20 minutes)…….antioxidants prevented the glucose-regulating effects of exercise……The idea free radicals may be beneficial appears counterintuitive…….However, we tend to forget that the body is highly adaptive; interfering with its processes might be detrimental……..exercise transiently increases ROS, which induces genes to express enzymes that ultimately increase insulin sensitivity and help to detoxify ROS.
• Data suggest that there is no association between the use of antioxidant supplements (including selenium, zinc, and beta carotene) and an increased risk for melanoma (Arch Dermatol. 2009;145:879-882)……..The findings are in contrast to those from the recent Supplementation in Vitamins and Mineral Antioxidants (SUVIMAX) study, which involved about 13,000 people.
• SUVIMAX found a 4-fold higher melanoma risk in women — but not in men — who used nutritionally appropriate doses of antioxidant supplements (J Nutr. 2007;137:2098-2105).
• A study shows that multivitamins reduce the risk of cancer by 8%…mostly prostate cancers (JAMA 2012;308:1871-80)….but it’s really not that significant as it translates to 83 patients needing to take multivitamins for 11 years to prevent one case of cancer.
• There’s no evidence that multivitamins extend life (Prescriber’s Letter. 2013;20:3)….Encourage patients to keep things in perspective…..Explain that taking a multivitamin isn’t going to make up for smoking, too much sun exposure, poor diet, sedentary lifestyle, etc.
• High intake of total calcium and iron appear to be associated with greater odds of self-reported glaucoma according to an analysis of the National Health and Nutrition Examination Survey (NHANES)(American Academy of Ophthalmology (AAO) 2012 Annual Meeting. Abstract 126. Presented November 11, 2012). “But greater dietary intake of calcium and iron, however, was associated with a decreased odds of glaucoma in this study,” Dr. Wang added. “We think dietary rather than supplementary intake of iron and calcium may be absorbed differently, in different forms, or act in biologically different ways.” Therefore, that the increased odds for glaucoma may be driven by higher use of supplements.
Pediatric: A study suggests that more than 30% of U.S. children take dietary supplements daily, most often multivitamins and multiminerals (18.3%) followed by single vitamins (4.2%), single minerals (2.4%) and botanicals (0.8%) (Arch Pediatr Adolesc Med 2007;161:978-985)….Regular dietary supplement use in children correlated with higher family income, a smoke-free home, lower body mass index in children and less daily TV, video game or computer time.
• More non-Hispanic white and Mexican American children (38.3% and 22.4%, respectively) used supplements than non-Hispanic black children (18.8%). About one-third of American children and teens have taken supplemental vitamins in the past month, and most don’t need them according to a study yet those with varied diets, active lifestyles, and better access to health care are the most likely to take them (Arch Ped Adol Med 2009;163:150-157).
See above on recommendations. Roughly 30% of Americans use at least one vitamin or mineral supplement in a given month. The highest use is seen in non-Hispanic whites (42.6%) (Arch Fam Med 2000;9:258-62) If you are active and have a good appetite, you can get a lot of vitamins in your diet. Unlike an inactive elderly person, who might eat 1,000 to 1,500 calories per day. By choosing wholesome foods (fruits and vegetables), then, you can double or triple your vitamin intake. If you eat fewer than 1,500 calories per day, one multivitamin and mineral pill might be good. If you do not eat meat, iron and zinc supplements can be helpful.
• Despite its well-known health benefits, a daily multivitamin (x 1yr) may not help students ace exams or even make it to school on time suggests a study on 700 inner city New Jersey elementary school kids (J Am Dietetic Assoc 2010;July).
Do not take vitamins in the belief that “they couldn’t hurt”: Antioxidants [vitamin E (800 IU/day), vitamin C (500 mg/day), and ALA (900 mg/day); CoQ (400 mg/day)] do not improve AD biomarkers and adversely affected cognition (Arch Neurol 2012:Mar 19;e-pub ahead of print)…..This combination treatment was associated with significantly greater cognitive decline than placebo (MMSE, –2.8 vs. –0.9 points) and showed a trend toward greater functional deterioration.
Centrum Silver (for age >50): Contents: Vitamin A – 5000 IU. Vitamin C -60 mg. Vitamin D – 400 IU. Vitamin E – 45 IU. Vitamin K -10 mcg. Vitamin B6 – 3 mg. Thiamin – 1.5 mg. Riboflavin – 1.7 mg. Niacin – 20 mg. Folate – 400 mcg. Vitamin B12 – 25 mcg. Biotin – 30 mcg. Pantothenic acid – 10 mg. Calcium – 200 mg. Phosphorus – 48 mg. Iodine – 150 mg. Magnesium – 100 mg. Zinc – 15 mg. Selenium – 20 mcg. Copper – 2 mg. Manganese – 2 mg. Chloride – 72 mg. Potassium – 80 mg. Nickel – 5 mcg. Silicon – 2 mg. Vanadium – 10 mcg. Boron – 150 mcg (Data obtained from product label).
Centrum Advanced Formula (for active adults): Contents: Vitamin A – 5000 IU. Vitamin C – 60mg. Vitamin D – 400IU. Vitamin E – 30IU. Vitamin K – 25mcg. Thiamin – 1.5mg. Riboflavin – 1.7mg. Niacin – 20mg. Vitamin B6 – 2mg. Folate – 400mcg. Vitamin B12 – 6mcg. Biotin – 30mcg. Pantothenic acid – 10mg. Calcium – 162mg. Iron – 18mg. Phosphorus – 109mg. Iodine – 150mg. Zinc – 15mg. Selenium – 20mcg. Copper – 2mg. Manganese – 2mg. Chromium – 120mcg. Molybdenum – 75mcg. Chloride – 72mg. Potassium – 80mg. Nickel – 5mcg. Tin – 10mcg. Silicon – 2mg. Vanadium – 10mcg. Boron – 150mcg. Lutein – 250mcg.
Nature Made Essential Balance: Contents: Vitamin A – 5000IU. Vitamin C – 120mg. Vitamin D – 400IU. Vitamin E – 50IU. Vitamin K – 25mcg. Thiamin -1.5mg. Riboflavin – 1.7mg. Niacin – 20mg. Vitamin B6 – 2mg. Folate – 400mg. Vitamin B12 – 6mcg. Biotin – 30mcg Pantothenic acid – 10mg. Calcium – 100mg. Iron – 9mg. Phosphorus – 77mg. Iodine – 150mcg. Magnesium – 100mg. Zinc – 15mg. Selenium – 25mcg. Copper – 2mg. Manganese – 2mg. Chromium – 120mg. Molybdenum – 25mcg. Chloride – 36mg. Potassium – 40mg. Nickel – 5mcg. Tin – 10mcg. Silicon – 2mg. Vanadium – 10mcg. Boron – 150mg. Lutein – 250mcg. (Data obtained from product label)
One-A-Day: 50 Plus Formula: Contents: Vitamin A – 5000IU. Vitamin C – 120mg. Vitamin D – 400IU. Vitamin E – 60IU. Vitamin K – 20mcg. Thiamin – 4.5mg. Riboflavin – 3.4mg. Niacin – 20mg. Vitamin B6 – 6mg. Folate – 400mcg. Vitamin B12 – 30mcg. Biotin – 30mcg. Pantothenic acid – 15mg. Calcium – 120mg. Iodine – 150mcg. Magnesium – 100mg. Zinc – 22.5mg. Selenium – 105mcg. Copper – 2mg. Manganese – 4mg. Chromium – 180mcg. Molybdenum – 94mcg. Chloride – 34mg. Potassium – 37.5mg. (Data obtained from product label)
Rx Essentials: A new line of over-the-counter supplements promoted for “drug-induced nutrient depletion.” Costs ~$12 for a two-month supply. Comes in 5 formulas. While many drugs can affect nutrient levels…but most of these are not clinically significant. Patients who have a healthy diet and take a multivitamin usually don’t need Rx Essentials (Prescriber’s Letter 2008;15:2).
Rx Essentials for Cholesterol medication: contains vitamin B6 10 mg, vitamin B12 200 mcg, folic acid 400 mcg, and coenzyme Q-10 100 mg.
Rx Essentials for Anti-depressants: contains vitamin D 1000 units, vitamin B6 10 mg, vitamin B12 200 mcg, and folic acid 400 mcg.
Rx Essentials for Diabetes taking metformin: contains vitamin B6 10 mg, vitamin B12 200 mcg, and folic acid 400 mcg.
Rx Essentials for people taking heartburn or acid reflux medication: contains vitamin B6 10 mg, vitamin B12 200 mcg, vitamin D 1000 units, folic acid 400 mcg, and a very small amount of calcium (100 mg)
Rx Essentials for people taking NSAIDs: contains vitamin C 500 mg, vitamin D 1000 units, and folic acid 400 mcg.
Aluminum:
A light, ductile and malleable metal with atomic number 13 and symbol Al. Bound as oxides and complex aluminosilicates, it is the most abundant metal in the earth’s crust. Aluminum is not considered an essential nutrient for humans. However aluminum deficiency states have been reported in some animals. Goats fed diets low in aluminum have been reported to have depressed growth, an increased number of spontaneous abortions, decreased life expectancy, and incoordination and weakness in their hind legs. Chicks fed low-aluminum diets have been reported to have depressed growth. Typical daily dietary intake of aluminum ranges from about 2 to 8 milligrams. The major source of aluminum in foods is food additives, such as sodium aluminum phosphates in cake mixes, frozen dough, self-rising flour and processed cheese, as well as sodium aluminum sulfate in baking powder. Aluminum is found in a number of commercial teas. However, the absorption of aluminum from tea may be quite low. Aluminum-containing compounds are widely used in medicine and are found in many consumer products. Aluminum hydroxide is used as a phosphate binder in the tx of hyperphosphatemia and to control renal osteodystrophy and secondary hyperphosphatemia in pt’s with end stage renal disease on hemodialysis. Sucralfate is used in the tx of peptic ulcer disease. Aluminum and magnesium hydroxide mixtures are commonly used antacids. Aluminum-containing compounds are used as astringents, as antiperspirants and in underarm deodorants. < 1% ingested aluminum typically absorbed by intestine and primarily excreted by kidney; body burden of aluminum stable in healthy persons with normal elimination capacity.
Aluminum Concentrations Measured Using Graphite Furnace Atomic Absorption Spectrometry:
(Nutrition 1999;15(9):683)
Pediatric trace elements: 130-3,000 mcg/L
K-phosphates: 9,800 mcg/L
Na/K phosphates: 13,000 mcg/L
10% calcium gluconate: 4,400 mcg/L
6.5% amino acids: 30 mcg/L
10% amino acids: 120 mcg/L
12.5% amino acids: 121 mcg/L
20% lipid emulsion: 30-180 mcg/L
Water-soluble vitamins: 12 mcg/L
Lipid soluble vitamins: 360 mcg/L
Trace elements (standard for children 3-5 kg): 55 mcg/L
Trace elements (standard for children 5-10 kg): 90 mcg/L
Toxic effects: encephalopathy, osteomalacia and microcytic anemia—can occur in pt’s with chronic renal failure. The aluminum comes from excessive amounts of this substance in dialysis fluids and/or from its absorption from the oral doses of aluminum-containing medications given for the tx of hyperphosphatemia. Aluminum is also neurotoxic in experimental animals, premature infants and those with chronic renal failure who are not on dialysis. This neurotoxic activity of aluminum raised the concern of whether aluminum intake in healthy individuals could be a contributing factor to such d/o’s as Alzheimer’s disease. Although aluminum has not been ruled out as playing some role in Alzheimer’s disease, aluminum accumulation does not appear to occur to any appreciable extent in those with normal renal function who use aluminum-containing antacids. Consequently, it does not appear that dietary intake of aluminum would increase the risk of Alzheimer’s disease in the general population. However, this remains a controversial topic.
(Systemic aluminum toxicity: effects on bone, hematopoietic tissue and kidney. J Toxicol Environ Health. 1996;48:649-665) (A preliminary study of dietary aluminum intake and risk of Alzheimer’s disease. Age Aging. 1999;28:205-209)
Causes: Excess ingestion and absorption of aluminum from aluminum-containing drugs (antacids, phosphate binders). Excess aluminum in dialysate, usually derived from contaminated water. Excess aluminum in total parenteral nutrition (TPN). Commercial products, as well as administration sets, containers, and manipulation are all sources of aluminum in parenteral nutrition provided to premature infants (JPEN J Parenter Enteral Nutr 2010;34:322).
S/s: change in mental status, proximal muscle weakness, bone pain. Children may have growth retardation. Seizures. Coma. Motor disturbances – twitching, myoclonic jerks and motor apraxia. Defective spatial orientation. Usually slowly progressive.
Dx: bone biopsy considered gold standard for diagnosis (iliac crest bone biopsy with aluminum staining method of choice in patients with symptoms of aluminum toxicity).
Ddx: dementia, delirium, seizures, hyperparathyroidism, iron deficiency anemia (for microcytic anemia)
W/u: serum aluminum levels. A serum aluminum level > 200 mcg/L considered a contraindication for deferoxamine (DFO) test. Ck serum calcium, parathyroid hormone levels. The deferoxamine (DFO) test, also called desferrioxamine test in a non-invasive alternative to bone biopsy…serum aluminum level measured before and 2 days after DFO 5 mg/kg infusion.
75 mg/d for women, 90mg/d in men (Max of 2g/d). Used in microsomal electron transport, tyrosine, tryptophan, DA synthesis, steroid synthesis, hydroxylation of collagen proline and lysine and folic acid metabolism. Synthesis of collagen, osteoid, chondroid, dentin + intracellular cement substance, Facilitates absorption of inorganic iron. Vitamin C is stored in adrenal cortex.
Defic: Scurvy. See C defic |
Toxic effects: nephrolithiasis and diarrhea. See Vitamin Toxicity |
Normal levels: 0.5-1 mg/dL in serum, 15-30 mg/dL in WBC. The use of vitamin C supplements may protect against CAD, use associated with a 28% lower risk (J Am Coll Cardiol 2003;42:246-255).
Sources: About 90% of Vit-C in the average diet comes from fruits and vegetables. Peppers—sweet green and red peppers and hot red and green chili peppers—are especially rich in Vit-C. Other good sources include citrus fruits and juices, brussels sprouts, cauliflower, cabbage, kale, collards, mustard greens, broccoli, spinach, tomatoes, greens, potato, kiwi and strawberries. Nuts and grains contain very little vitamin C. Rose hips are the major source of natural Vit-C. Cooking destroys Vit-C activity.
Reduced-acidity Vit-C: consists of a mixture of 50% ascorbic acid and 50% sodium ascorbate. Some find this form of Vit-C a more tolerable supplement than ascorbic acid. Since the first pKa of ascorbic acid is 4.2, the pH of the mixture dissolved in water would be 4.2. Also known as buffered Vit-C.
Non-acid Vit-C: consists of an ascorbate salt of sodium or calcium which has a neutral pH when dissolved in water. The calcium salt consists of two molecules of ascorbate and one atom of calcium. The molecular formula is C12H14CaO12.
Tabs [OTC]: 100, 200, 250, 500 mg, 1, 1.5 g. Chewable tabs (Sunkist Vitamin C) [OTC]: 60, 100, 250, 500, 1000 mg (some may contain aspartame)
Tabs (timed release) [OTC]: 0.5, 1, 1.5 g. Caps [OTC]: 500 mg. Extended-release caps [OTC]: 250, 500 mg. Solution (Cecon) [OTC]: 100 mg/mL (50 mL). Liquid [OTC]: 500 mg/5 mL (120, 480 mL). Lozenges [OTC]: 60 mg.
Scurvy (PO/IM/IV/SC): Rx Child @ 100–300 mg/24 hr divided QD–BID for at least 2 wk. Adults @ 100–250 mg QD–BID for at least 2 wk.
SE: Adverse reactions: nausea, vomiting, heartburn, flushing, headache, faintness, dizziness, hyperoxaluria. Use high doses with caution in G6PD pt’s. May cause false-negative and false-positive urine glucose determinations with glucose oxidase and cupric sulfate tests, respectively. Oral dosing is preferred with or without food. IM route is the preferred parenteral route. Protect the injectable dosage form from light.
IV doses: [Injection: 250, 500 mg/mL] can produce plasma concentrations 30-70 fold higher than the max tolerated oral doses, IV Vit-C commonly used for cancer tx by alternative practitioners and should be re-evaluated (Ann Int Med 2004;533-37).
Info: The term vitamin C applies to substances that possess antiscorbutic activity and includes two compounds and their salts: L-ascorbic acid, commonly called ascorbic acid, and L-dehydroascorbic acid. Ascorbic acid is the major dietary form of Vit-C. The terms Vit-C, ascorbic acid and ascorbate are commonly used interchangeably. Vit-C is a hexose derivative, similar in structure to the six-carbon sugar glucose. It is required in the diet by only a few species of animals—man, other primates, the guinea pig, an Indian fruit-eating bat, and the red-vented barbul and some related species of Passeriform birds. It is also an essential nutrient for Coho salmon, rainbow trout, carp and some insects. Most other animals, all higher plant species and probably all algal classes can synthesize Vit-C from glucose or other sugars. Molecules similar to ascorbic acid are made by some fungi but not by bacteria. All Vit-C requiring animals lack the enzyme L-gulano-gamma-lactone oxidase, the final step in the synthesis of ascorbic acid from glucose.
• A meta-analysis of 72 trials examining the benefits of regular vitamin C supplementation concludes that although vitamin C may have a modest yet consistent effect on the duration of colds, it has no effect on the incidence of colds, except in people exposed to short periods of extreme physical stress (such as marathon runners, skiers, and soldiers on subarctic exercises had a 52% reduction in risk) (Cochrane Database Syst Rev. 2013;Published online January 31)…..vitamin C supplements were associated with about an 8% reduction in duration of symptoms in adults and a 14% reduction in children at 1 to 2 g/day……The effect of therapeutic vitamin C (up to 8 g/day begun after onset of symptoms) showed no consistent effects of vitamin C on either severity or duration of colds. Routine vitamin C supplementation is not justified, yet vitamin C may be useful for people exposed to brief periods of severe physical exercise,” the authors write. “Nevertheless,” they conclude, “given the consistent effect of vitamin C on the duration and severity of colds in the regular supplementation studies, and the low cost and safety, it may be worthwhile for common cold patients to test on an individual basis whether therapeutic vitamin C is beneficial for them.”
• A prospective cohort study suggests that higher plasma levels of vitamin C are associated with a reduced risk for stroke (Am J Clin Nutr. 2008;87:5-7, 64-69)…..those in the highest quartile for plasma vitamin C had a 42% reduced risk for stroke compared with those in the lowest quartile…..a biomarker of fruit and vegetable consumption, which have many nutrients which may be biologically active and protective for stroke….”Measuring plasma vitamin C levels may identify those who will most benefit from established risk factor management such as blood pressure control.”
• Research suggests that gamma-aminobutyric acid (GABA) receptors in the retina need ascorbic acid (vitamin C) to function properly (J Neurosci. 2011;31:9672-9682)……”a vitamin C–rich diet could be neuroprotective for the retina, especially for people who are prone to glaucoma or to epilepsy or other conditions involving overexcitation of the brain”.
• Use of vitamin C (ascorbic acid) supplements (~1000 mg) is associated with development of kidney stones in men according to data on 50,000 men in Sweden followed over 11 years (0.9% developed kidney stones)(JAMA Intern Med. 2013;Published online February 4)(adjusted relative risk, 1.92). Urinary oxalate is an important determinant of calcium oxalate kidney stone formation. Vitamin C is excreted in urine both in its unmetabolized form and as oxalate.
Cancer: A report of 3 cases in which high-dose IV Vit-C (15-65 g twice a week for 10 mo’s) apparently led to longer-than-expected survival in pt’s with advanced cancer (CMAJ 2006;174:937-942).
Vitamin A (V-A, Retinol, Retinoic Acid, Beta carotene):
RDA is 300-500ug in child, 900ug in male >14yo and 700ug in female, 1200ug if lactating. ~= 4,000-5,000 IU/d (800-1000 mg RE). Vitamin A refers to a group of fat-soluble substances that are structurally related to and possess the biological activity of the parent substance of the group called all-trans retinol or retinol. Found in green leafy vegetables, dairy, yellow fruits and vegetables, liver. Needed for light sensitive pigments in the retina, epithelial maintenance (retinoic acid), immune function.
Normal level: 20-60 mcg/dL (-.7-2 umol/L).
Defic: Keratomalacia: (dry conjunctiva, corneal ulcers and prolapse of the iris), Bitot’s spots (white/ yellow spots under the conjunctiva), gingivitis, dry skin with hyperkeratinization, night blindness. Some carotenoids, most notably beta-carotene, are metabolized into compounds with vitamin A activity and are considered to be provitamin A compounds. Vitamin A is an integral component of rhodopsin and iodopsin, light-sensitive proteins in retinal rod and cone cells. Pt’s with a remote history of major intestinal surgery (intestinal bypass / resection) may have an increased risk of vitamin A deficiency (Br J Ophthalmol 2006:June).
Vitamin A (Aquasol A and others): [Caps: 10,000 IU (OTC), 15,000 IU (OTC), 25,000 IU. Tabs: 5000 IU (OTC), 15,000 IU. Injection: 50,000 IU/mL (2 mL)]
Supplementation in measles (6 mo to 2 yr): 6 mo–1 yr: 100,000 IU/dose QD PO x2 days. Repeat 1 dose at 4 wk. 1–2 yr: 200,000 IU/dose QD PO x2 days. Repeat 1 dose at 4 wk. The use of vitamin A in measles is recommended in children 6 mo to 2 yr who are either hospitalized or have any of the following risk factors: immunodeficiency, ophthalmologic evidence of vitamin A deficiency, impaired GI absorption, moderate to severe malnutrition, or recent immigration from areas with high measles mortality.
Malabsorption syndrome prophylaxis: Child>8 yr and adult: 10,000–50,000 IU/dose QD PO of water-miscible product.
SE: High doses above the U.S. RDA are teratogenic (category X). May cause GI disturbance, rash, headache, increased ICP (pseudotumor cerebri), papilledema, and irritability. Large doses may increase the effects of warfarin. Mineral oil, cholestyramine, and neomycin will reduce vitamin A absorption.
Toxicity: See Vitamin Toxicity |
Deficiency: The earliest sign of vitamin A deficiency is a decrease in dark adaptation, or night vision. Serum retinol levels are not predictive of subclinical deficiency states.
Rapid dark adaptation test (RDAT): (Ann Ophthalmol 1977;9:731–734) The basis for the test is the measurement of the time of the so-called Purkinje shift = the shifting of peak retinal wavelength sensitivity from the red toward the blue end of the visual spectrum during the transition from day (cone-mediated) vision to night (rod-mediated) vision. When color vision is non-functional, this shift causes the intensity, not the color, of blue to appear brighter than red under dim lighting.
Step #1: The procedure is explained to the subject.
2. The subject is light-adapted by fixation on a standard X-ray viewer for 1 minute at a distance of 0.5 m. The X-ray viewer is then turned off (the darkroom light is, of course, on).
3. The subject is given a pile containing all 18 discs mixed in random order and the stopwatch is started.
4. The subject separates the white and then the blue discs as fast as possible. Under these controlled lighting conditions, the subject will not be able to recognize the colors, since the cones cannot distinguish color with the limited light available. The ability to separate the discs by brightness is therefore dependent upon the rods. Any disc mistakenly separated by the subject is returned to the original pile until 100% accuracy of sorting is achieved.
5. The first test performed by a subject should be redone to allow for learning and standardization.
Equipment and supplies: Light-proof room. A standard darkroom light fixture fitted with a 7.5 W bulb and a neutral density filter (allowing 1% transmittance). Alternately, an exposed X-ray film may serve as filter. The bottom of the fixture is suspended 1.2 m above the work surface, so that the target brightness on the work area is approximately 0.0068 candela/m2 .
• Munsell color discs with matte finish – five white discs (N9.5/-), six blue discs (5PB5/10), and seven red discs (5R5/10). Available from Munsell Color and Macbeth Division (Baltimore, MD). A non-reflective work surface. A stopwatch. A standard X-ray viewbox.
Normals: 20–39 yo: 3.03 ± 1.00 min. 40–60 yo: 4.41 ± 0.83 min.
Vit-A-deficient: 7.63 ± 1.79 min (Am J Clin Nutr 1981;34:1961-1966).
Conditions causing abnormal RDAT results with normal levels of vitamin A: Zinc deficiency. Cataract. Retinitis pigmentosa. Diabetic retinopathy. Severe errors of refraction. Miosis caused by pharmaceutical agents. Tinted corrective lenses.
Giving vitamin A capsules to children aged 6 months to 5 years may reduce deaths and incidence of measles and diarrhea (Cochrane Database Syst Rev. Published online December 8, 2010). ….Among 7 trials reporting mortality from diarrhea, there was a 28% overall reduction for VAS (RR, 0.72; 95% CI, 0.57 – 0.91)…..Vit A defic (VAS) was associated with a lower incidence of diarrhea (RR, 0.85; 95% CI, 0.82 – 0.87) and measles morbidity (RR, 0.50; 95% CI, 0.37 – 0.67), there was no significant impact on respiratory tract disease incidence or hospitalizations for diarrhea or pneumonia. Within the first 48 hours of VAS, the risk for vomiting was increased (RR, 2.75; 95% CI, 1.81 – 4.19).
Beta-Carotene:
5-6mg/d. Antioxidant, can be converted to V-A. Found in carrots, sweet potatoes, yellow-green veges, mangoes, apricots, papaya. Defic: same as V-A. During active tx, beta-carotene supplementation appears to increase risk of lung cancer among smokers (JAMA 2003;290:476-485).
• Beta-carotene supplementation leads to a small but significant increase in all-cause morbidity and mortality from CVD among adults who take them for 4-6 years (Use of antioxidant vitamins for the prevention of cardiovascular disease: Meta-analysis of randomized trials. Lancet 2003;361:2017-23).
• Beta-carotene (25 mg/d) reduced the risk of colon polyp recurrence, but smoking and drinking attenuated this benefit (J Natl Cancer Inst 2003;95:697-699).
Thiamine (B1): Link: Wernicke-Korsakoff Syndrome |
1-1.5mg/d. Dietary sources include legumes, pork, beef, whole grains, yeast, enriched breads/ cereals, wheat germ, organ meats, nuts, beans and peas and fresh vegetables. A deficiency state can occur in as little as 3 weeks following total dietary absence. Cofactor for transketolase, pyruvate to metabolize branched chain ketoacids. Essential for glucose and alcohol metabolism. A water-soluble compound containing substituted pyrimidine and thiazole rings and a hydroxyethyl side chain. Thiamine combines with ATP to form thiamine pyrophosphate (TPP) coenzyme, a necessary component for carbohydrate metabolism. Serves as a coenzyme in many alpha-keto-acid decarboxylation and transketolation reactions. Synonyms: Aneurine, Thiaminium.
Deficiency: Inadequate thiamine availability leads to impairment of the above reactions and consequently to inadequate ATP synthesis and abnormal carbohydrate metabolism. Lactic acidosis, Wernicke-Korsakoff syndrome (see below), Wet beriberi (high output CHF, edema, peripheral vasodilation), Dry beriberi (peripheral neuropathy, muscle wasting), hyperglycemia (impaired insulin secretion). The brain is extremely sensitive to thiamine deficiency.
Normal levels: 1.6-4 mg/dL or 8-15 IU ETK or <10% TPP effect.
Recommended daily allowance: <6 mo’s: 0.3 mg,
6 mo’s to 1 year: 0.4 mg, 1-3 years: 0.7 mg,
4-6 years: 0.9 mg, 7-10 years: 1 mg,
11-14 years: 1.1-1.3 mg, >14 years: 1-1.5 mg.
Thiamine (Thiomalate, Betaxin, others) [OTC: 20, 50, 100, 250, 500 mg tabs. 100 mg/mL inj]
Beriberi (thiamine deficiency): Child @ 10–25 mg/dose IM/IV QD (if critically ill) or 10–50 mg/dose PO QD x 2 wk, followed by 5–10 mg/dose QD x 1 mo. Adult @ 5–30 mg/dose IM/IV TID x 2 wk, followed by 5–30 mg/24 hr PO divided QD or TID x 1 mo.
Wernicke’s encephalopathy syndrome: See below.
Toxicity: excess intake is largely excreted in the urine although parenteral doses >400 mg/d are reported to cause lethargy, ataxia, and reduced tone of the GI tract.
Wernicke-Korsakoff Syndrome (WKS):
Link: See Korsakoff’s psychosis & Tx | AKA Alcoholic polyneuritic psychosis. Wernicke’s encephalopathy (WE) is a common, acute, severe partially reversible neurologic d/o caused by thiamine deficiency that occurs most commonly in alcoholics. Korsakoff’s amnestic syndrome is a late, neuropsychiatric manifestation of WE. Wernicke’s encephalopathy is a medical emergency with a mortality rate of 10-20%. Wernicke-Korsakoff syndrome is one of the sequelae of WE (Alcohol Alcohol 2009;44:148).
Etiology: Thiamine deficiency in alcohol abusers is due to a combination of inadequate dietary intake, reduced GI absorption, decreased hepatic storage and impaired utilization. Staple diet of polished rice (milling removes the husk). GI surgical procedures such as gastrectomy; gastrojejunostomy; partial or subtotal colectomy; gastric bypass surgery; vertical banded gastroplasty; therapy with an intragastric balloon. GI disorders such as peptic ulcer; gastric cancer; colon cancer; ulcerative colitis with megacolon; severe obesity. Recurrent vomiting or chronic diarrhea. Pyloric stenosis; peptic ulcer; drug-induced gastritis; biliary colics; Crohn’s disease; intestinal obstruction or perforation; lithium-induced diarrhea; migraine attacks; anorexia nervosa; pancreatitis; hyperemesis gravidarum. Cancer and related conditions: gastric carcinoma; non-Hodgkin’s lymphoma; myelomonocitic leukaemia; large B-cell lymphoma; myeloid leukaemia; allogenic bone marrow transplantation. Chemotherapeutics with erbulozole; ifosfamide. Systemic diseases such as Renal diseases; AIDS; chronic infectious febrile diseases; thyrotoxicosis. Magnesium depletion (cofactor). Secondary to chronic diuretic therapy; intestinal tract resection; Crohn’s disease. IV infusion of high-dose nitroglycerin; tolazamide. Absolute deficiency of food/thiamine: dietary restrictions owing to economic reasons or political trade embargoes; psychogenic food refusal; fasting for religious-philosophical reasons; starvation for tx of obesity; hunger strike; neglect in old age or Alzheimer’s disease.
• Bariatric surgery appears to increase the risk of atypical WE (Neurology 2007; 68:807-811) (32 cases reported, mostly womenafter vertical banded gastroplasty, Roux-en-Y gastric bypass, elective gastric partitioning, and gastric plication).
• An X-linked transketolase-like 1 (TKTL1) gene might also contribute to genetic susceptibility to WKS (Genomics 1996;32:309-316). Genetic and environmental factors may also play a part in the pathogenesis in this d/o. An inborn enzymatic error, a thiamine-dependent enzyme, transketolase, is deficient or less responsive in some pt’s with the WKS. This may explain why the d/o develops in only a few alcoholics. Persons with transketolase deficiency are asymptomatic until they are stressed by thiamine def. Protracted vomiting, inadequate diet, and malabsorption all contribute to thiamine deficiency in the alcoholic.
• Mammillothalamic connectivity is reduced in patients with alcoholism and WE compared with both patients without WE and healthy controls (Brain 2009;132:369)……The mammillary bodies and thalamus are important centers within a complex, interconnected, limbic memory circuit.
S/s: Early detection of subclinical thiamine deficiency is a difficult task, as sx’s may be vague and non-specific, such as frequent headaches, fatigue, irritability, abdominal discomfort, and decline in the growth rate of children.
The classic description (triad) of WE includes: the classic trio of eye movement abnormalities, confusion, and ataxia are seen in <20% of pt’s (Neurology. 2005;65:1847). WKS consists of neuronal loss, microhemorrhages, and gliosis in the paraventricular and periaqueductal grey matter.
(1) oculomotor disturbances: begins with nystagmus and lateral rectus or horizontal gaze paresis and progress to complete ophthalmoplegia- CN VI loss, usually with pupillary sparing. Nystagmus is the most common finding and is typically evoked by horizontal gaze to both sides.
(2) encephalopathy: abnormal mentation (usually confusion, amnesia, mental slowing (abulia), confabulation). These changes largely result from an involvement of thalamic or mamillary bodies and range from a confusional state to mental sluggishness, apathy, impaired awareness of the immediate situation, inability to concentrate and, if left untreated, coma and death (Lancet Neurology 2007;6:5).
(3) gait ataxia resulting in part from thiamine deficiency. Likely due to a combination of polyneuropathy, cerebellar involvement, and vestibular paresis. Peripheral neuropathy typically involves just the lower extremity, pt’s complain of the gradual onset of weakness, paresthesias, and pain affecting the distal lower extremities. Some have no sx’s, but examination reveals diminished or absent ankle jerks and patchy distal sensory loss.
CV: involvement of the cardiovascular system may take two forms: a common, high-output state characterised by heart failure, orthopnea, and pulmonary and peripheral edema, and a rare, low-output state, characterised by severe hypotension, lactic acidosis, and absence of edema.
• A study found that patients with KS scored better than patients with dementia on the QUALIDEM subscales “Restless tense behavior,” “Social relations,” and “Having something to do” (JAMDA. 2012;13:778-781)……Patients with KS tend to have more social relationships and more positive emotions than patients with dementia. Furthermore, patients with dementia show more restless behavior than patients with KS; however, patients with KS tend to feel less at home in a nursing home than patients with dementia.
Dx: It remains a clinical dx and is poorly recognized because the complete triad is found in as few as 12% of pt’s. Difficult if not impossible, to differentiate from drunkenness. No specific routine lab test available, and no specific diagnostic abnormalities have been revealed in CSF, brain imaging, EEG, or evoked potentials and none are required tx dx.
Proposed new criteria require two of these signs: (1) dietary deficiencies, (2) oculomotor abnormalities, (3) cerebellar dysfunction, and (4) either an altered mental state or mild memory impairment. The dx should be entertained in any alcoholic or malnourished pt presenting with ocular abnormalities, ataxia, altered mental status, hypothermia, or coma. The most effective measure of B1 status is the erythrocyte transketolase activity coefficient, which measures enzyme activity before and after addition of exogenous TPP: RBC’s from a deficient individual express a substantial increase in enzyme activity with addition of TPP.
MRI: The lesions of WE occur in a characteristic, symmetrical distribution in structures surrounding the third ventricle, aqueduct, and fourth ventricle. MRI may show symmetric hyperintense signal on T2-weighted and fluid attenuated inversion recovery images at the floor of the fourth ventricle, periaqueductal gray matter, the medial portions of both thalami, and the premotor and motor cortices, with contrast enhancement in all T2 hyperintense regions.
Ddx: paramedian thalamic infarction (top-of-the-basilar syndrome), ventriculoencephalitis, Miller-Fisher syndrome, primary cerebral lymphoma, Behçet’s disease, multiple sclerosis, Leigh’s disease, variant Creutzfeldt-Jakob disease, paraneoplastic encephalitis, severe hypophosphataemia, acute intoxication from methyl bromide, and chronic intoxication from bromvalerylurea.
Korsakoff’s psychosis: an amnesic state, also called alcohol-induced persisting amnestic d/o, refers to a d/o with primarily recent memory impairment, inability to learn new information or recall previously learned information, apathy, and confabulation. It is a neuropsychiatric d/o of selective anterograde, retrograde amnesia, apathy, an intact sensorium, and relative preservation of long-term memory and other cognitive skills. Although common, confabulation is not essential for the dx. Age >40yo and many years of heavy alcohol use are risk factors. The onset may be abrupt or insidious. Usually follows or accompanies WE, with the typical clinical pattern emerging when the acute global confusional state of the latter resolves. Prompt tx of WE with adequate doses of parenteral thiamine may prevent the development of Korsakoff’s syndrome, but this syndrome responds little if at all to thiamine therapy. Pt’s with Korsakoff’s syndrome present with a severe anterograde amnesia and are unable to remember events even within the previous half an hour, although they retain implicit learning, so these pt’s can learn new motor skills or develop conditioned reactions to stimuli. Disorientation to time is noticeable. Other cognitive functions are preserved in most pt’s, or may show only minor deficits (eg, executive functions). Confabulation accompanies the memory defect in the early stages but becomes less apparent after months or years. Emotional changes may develop, including apathy, blandness, or mild euphoria, with little or no reaction to events. The dx is supported by neuroimaging or autopsy findings that show thalamic and mammillary-body degeneration and frontal-lobe atrophy. With Korsakoff’s get confabulation, anterograde amnesia (some retrograde), pt is “stuck in time” thus fixated in their past, pleasantly apathetic, no cure.
Tx: Alcoholics with altered mental status or signs of WE should receive naloxone (0.08 mg IV), thiamine (500 mg IV dissolved in 100 ml of normal saline), and either a rapid blood glucose determination or empiric dextrose (25 g IV). Give the thiamine by infusion over a period of 30 min TID x 2–3 days. Tx for WKS consists of abstinence, adequate diet, and thiamine. Doses of thiamine between 100-250 mg per day apparently may not restore vitamin status, improve clinical signs, or prevent death (Lancet Neurology 2007;6:5). Continue the Thiamine 50–100 mg IM/IV QD until pt resumes a normal diet. (Administer thiamine before starting glucose infusion, because glucose alone can precipitate the disorder in thiamine-deficient individuals). Then PO 10 mg daily until the pt fully recovers. Must be given before or concurrent with dextrose fluids as a glucose load will incr metabolic demand for thiamine. With pure Wernicke’s, can tx with Thiamine an pt usually gets better in 1-2 days. Most suggest that parenteral thiamine tx should be initiated immediately while the pt’s are still drunk and continued for an adequate time for any pt with evidence of Wernicke’s encephalopathy when sober. The ophthalmoplegia and nystagmus usually have a good response to thiamine (hours to days). Ataxia tends to improve less completely; more than half of pt’s are left with a broad-based, unsteady gait. More serious are lasting mental sx’s. Drowsiness, inattentiveness, and apathy tend to clear with tx, but an amnestic d/o often persists, termed Korsakoff’s syndrome, in which both anterograde and retrograde memory loss occur–sometimes accompanied by confabulation–which is out of proportion to additional mental abnormalities. Once established, the memory d/o is permanent in the majority of pt’s. The ataxia and mental changes may take days to weeks to improve and usually have a poorer prognosis. <25% of pt’s show any real recovery, 50% show some recovery, and the remainder show no response despite adequate thiamine replacement. Because magnesium is a cofactor for this enzyme system, serum levels should be corrected. Pt’s with Wernicke’s syndrome require admission and aggressive thiamine and magnesium repletion. Recovery is variable in the Korsakoff or alcohol amnesic state.
80% of pt’s with WKS have peripheral neuropathy, and many alcoholics have peripheral neuropathy without other neurologic sx’s or signs. The earliest sx’s are sensory in nature, with paresthesias or pain in the feet and later the hands. Absent ankle tendon reflexes and impaired distal vibratory and pain sensation usually precede proprioceptive loss or weakness, but progression to a severe sensorimotor d/o can occur, with proximal as well as distal weakness in addition to vagal sx’s (hoarseness, dysphagia) and autonomic signs (tachycardia, postural hypotension). Alcoholic myopathy can be either chronic, with progressive proximal weakness, or acute, with rhabdomyolysis, severe muscle weakness and pain, and myoglobinuria causing renal failure. Serum creatine kinase levels are elevated, and electromyography reflects myopathy. Such pt’s are often malnourished, but direct toxicity is probably more important than nutritional deficiency. Other factors, most importantly hypokalemia, are often present and contribute to the muscle necrosis and myoglobinuria. Sx’s sometimes begin or accelerate during a binge, and improvement follows abstinence. Alcoholic cardiomyopathy, a low-output state distinguishable from beriberi heart disease, is often coexistent. Alcoholic cerebellar degeneration manifesting as gait impairment, tremor and dysarthria.
Prognosis: 25% of pt’s with the Korsakoff syndrome ‘recover’, 50% show improvement through time, and 25% remain unchanged. It is unlikely that any established pt shows complete recovery, but substantial improvement does occur over a matter of years.
Alcoholic myopathy: can be either an acute or indolent. The acute form develops in relation to an alcoholic binge, presenting with weakness, pain, tenderness, and swelling of proximal muscles. Dysphagia and congestive heart failure may occur.
Alcoholic polyneuropathy: a gradually progressive d/o of sensory, motor, and autonomic nerves. Usually symmetric and predominantly distal. Numbness, paresthesia, burning dysesthesia, pain, weakness, muscle cramps, and gait ataxia.
Marchiafava-Bignami disease: occurs almost exclusively in alcoholics, is defined by characteristic demyelinating lesions of the corpus callosum. Early sx’s are usually mental in nature, with depression, paranoia, psychosis, or dementia. Major motor seizures are common, and hemiparesis, aphasia, abnormal movements, and ataxia may progress to coma and death over a few mo’s. CT and MRI can detect the lesions, and in a few cases clinical improvement has been accompanied by regression of the CT or MRI abnormalities. The cause of Marchiafava-Bignami disease, including the role–if any–of nutritional deficiency, is unknown. (Operational criteria for the classification of chronic alcoholics: identification of Wernicke’s encephalopathy. J Neurol, Neurosurg Psychiatry 1997;62:51) (Wernicke’s encephalopathy. Lancet Neurology 2007;6:5)
ICD-9: 291.1 Alcohol amnestic syndrome
Ddx: Brain tumor. Cerebral anoxia. Dementia from any cause.
1.3-1.7 mg/d. Found in dairy foods, organ meats, enriched cereals, green leafy veges, eggs, nutritional yeast, fortified soy milks, vegetarian burger patties, ready-to-eat breakfast cereals and peanuts. If pt limits animal products in their diets, they should take supplements or eat fortified food. Used as electron transporter in flavin metabolism. Can be synthesized from tryptophan in foods. A compound consisting of a substituted isoalloxazine ring with a ribitol side chain. Serves as a coenzyme for diverse biochemical reactions. The primary coenzymatic forms are flavin mononucleotide and flavin adenine dinucleotide. Riboflavin holoenzymes participate in oxidation-reduction reactions in myriad metabolic pathways.
Deficiency: Usually found in conjunction with deficiencies of other B vitamins. Isolated deficiency of riboflavin produces hyperemia and edema of nasopharyngeal mucosa, cheilosis, angular stomatitis, glossitis, seborrheic dermatitis, and a normochromic, normocytic anemia. Soreness and burning of the mouth from cheilosis, angular stomatitis, gingivitis, atrophic lingular papillae, hypertrophy of filiform and fungiform papillae, seborrheic dermatitis, conjunctivitis, photophobia, anemia.
Riboflavin: [25, 50, 100 mg tabs OTC] Tx deficiency: Child @ 2.5–10 mg/24 hr divided QD–BID PO. Adult @ 5–30 mg/24 hr divided QD–BID PO. Hypersensitivity may occur. Administer with food. Causes yellow to orange discoloration of urine.
Toxicity: not reported in humans.
Assessment: the most common assessment is determining the activity coefficient of glutathione reductase in RBC’s (the test is invalid for individuals with glucose-6-phosphate dehydrogenase deficiency). Measurements of blood and urine concentrations are less desirable methods.
13-20 mg/d. Found in meats, peanuts, liver, enriched grains/ breads. Nicotinamide adenine dinucleotide (NAD) and nicotinamide adenine dinucleotide phosphate (NADP), which are involved in redox reactions (electron transport), the oxidation of fuel molecules, and fatty acid biosynthesis.
Defic: = Pellagra: 4 D’s–> Dermatitis (hyperpigmented, weeping, edema with fissuring, common on the head & neck or sun exposed areas), Dry MM’s, Diarrhea, Dementia. Fissured tongue with atrophy of lingular papillae, scaling/ dry/ atrophic/ thickened/ hyperpigmented skin, dementia, diarrhea. Most common in alcoholics. Often affects populations where corn is the major source of energy endemic in parts of China, Africa, and India.
Normal levels: 4-9 mcg/ml. Blood levels of vitamin not reliable. Measurements of urinary excretion of the niacin metabolites N-methyl nicotinamide and 2-pyridone are thought to be the most effective means of assessment at present. Refers to nicotinic acid and the corresponding amide nicotinamide. The active coenzymatic forms are composed of nicotinamide affixed to adenine dinucleotide to form NAD or NADP. Over 200 apoenzymes use these coenzymes as electron acceptors or hydrogen donors. The essential amino acid tryptophan is used as a precursor of niacin; 60 mg of dietary tryptophan yields ~ 1 mg of niacin. Dietary requirements depend partly on the tryptophan content of diet. See endocrine, lipid d/o’s.
Tx of pellagra @ 300-500 mg PO divided qd or 50-100 mg IM 5x/d or 25 mg IV bid (max 500 mg/d).
Toxicity: hypolipidemic effects. Includes vasomotor phenomenon (flushing), hyperglycemia, parenchymal liver damage, and hyperuricemia.
RDA of 2mg/d in men, 1.6mg/d in women. Age 1-3 yo @ 0.9 mg, 4-6 yo @ 1.3 mg, 7-10 yo @ 1.6 mg. As a coenzyme, B6 is involved in many transamination reactions (and thereby in gluconeogenesis), in the synthesis of niacin from tryptophan, and in the synthesis of several neurotransmitters, and delta-aminolevulinic acid (and therefore in heme synthesis). B6 is vital to more than 100 enzyme processes in the body, mostly those involving the metabolism of protein.
Found in: pork, glandular meats, bananas, bran/germ cereals, milk, egg yolk, oatmeal and legumes. Chicken breast, hamburger, fish, pinto beans, and vegetables like red peppers and potatoes.
Defic: Seen in conjunction with other water-soluble vitamin deficiencies. Glossitis, peripheral neuropathy, dementia, MCHC anemia, sz, N/V, cheilosis, depression. A normochromic, normocytic anemia has been reported in severe deficiency. Abnormal EEGs and, in infants, convulsions have been observed. Some sideroblastic anemias respond to B6 administration. Isoniazid, cycloserine, penicillamine, ethanol, and theophylline can inhibit B6 metabolism. Subclinical B6 deficiency frequently occurs in those with malabsorption syndromes, uremia, cancer, heart failure and cirrhosis, and in alcoholics, the elderly and adolescent females and during pregnancy.
• Low levels of vitamin B6 may be a key factor involved with chronic inflammation in the body (J Nutr 2012;July)…..people with the lowest levels of vitamin B6 in their blood had the highest levels of chronic inflammation, based on a wide variety of indicators.
Tx: Pyridoxine (Aminoxin, Vit-B6): [OTC: 25, 50, 100, 250, 500 mg tabs and Rx inj 100 mg/mL]
Deficiency, IM/IV/PO (PO preferred): Child: 5–25 mg/24 hr x 3 wk, followed by 1.5–2.5 mg/24 hr as maintenance therapy (via multivitamin preparation). Adult: 10–20 mg/24 hr x 3 wk, followed by 2–5 mg/24 hr as maintenance therapy (via multivitamin preparation)
Drug-induced neuritis, (INH, hydralazine, penicillamine, cycloserine): Prophylaxis (PO): Child: 1–2 mg/kg/24 hr. Adult: 25–100 mg/24 hr.Tx Child: 10–50 mg/24 hr. Adult: 100–300 mg/24 hr.
Sideroblastic anemia: Adult: 200–600 mg/24 hr PO x 1–2 mo. If adequate response, dose may be reduced to 30–50 mg/24 hr.
Pyridoxine-dependent seizures: Neonate/infant: Initial: 50–100 mg/dose IM or rapid IV x 1. Maintenance: 50–100 mg/24 hr PO. Acute hydralazine toxicity @ 25 mg/kg in divided doses IM/IV.
Info: Use caution with concurrent levodopa therapy. Chronic administration has been associated with sensory neuropathy. Nausea, headache, increased AST, decreased serum folic acid level, and allergic reaction may occur. May lower phenytoin levels. Burning may occur at the injection site after IM or SQ administration; seizures have occurred following IV administration of very large doses.
Normal levels: EGOT index <1.5. Plasma or erythrocyte PLP levels are most common. Urinary excretion of xanthurenic acid after an oral tryptophan load or activity indices of RBC alanine or aspartic acid transaminases (ALT and AST, respectively) all functional measures of B6 -independent enzyme activity.
Toxicity: chronic use with doses exceeding 200 mg/d (in adults) may cause peripheral neuropathies and photosensitivity. Assessment of Status Many lab methods of assessment exist. Studies have shown taking more than 500 mg a day can cause nerve damage, difficulty walking, or tingling.
2-3 mcg/d. Found in meats, milk, eggs, fish, cheese, poultry. Used as a methyl donor in carboxylation reactions such as DNA synthesis (with folate), reduces blood homocysteine levels. Strict vegetarians and elderly (>60yo have atrophic gastritis and cannot absorb) need supplements.
Defic: glossitis, optic neuritis, hyporeflexia, dementia, ataxia, anorexia, loss of proprioception and vibration sense, megaloblastic/ pernicious anemia. 7 P’s of pancytopenia, peripheral neuropathy, pyramidal tract signs, papillary atrophy, pH elevation (GI), psychosis and posterior column disease =subacute combined degeneration (stocking-glove paresthesias, clumsiness, ataxia, weakness and spasticity).
Nl level: 150-900 pg/ml.
Recommended daily allowance (RDA): 2.4 mcg/day for adults. Pregnancy: 2.6 mcg/day. Lactation: 2.8 mcg/day. Peds: RDA = 0.3-1.4 mcg/day.
Tx Vitamin B12 deficiency: Intranasal @ 500 mcg in one nostril once weekly. Oral @ 250 mcg/day. IM or deep SubQ @ Initial: 30 mcg/day for 5-10 days, then maintenance: 100-200 mcg/month.
Tx Pernicious anemia: IM or deep SubQ @ 100 mcg/day for 6-7 days or 1000 mcg/day for 5 days (followed by 500-1000 mcg/month). Once in hematologic remission can use Intranasal gel @ 500 mcg in one nostril once weekly or oral @ 1000-2000 mcg/day or IM / SubQ @ 100-1000 mcg/month.
50-200 mcg/d. Found in most foods such as liver, egg yolk, mushrooms, fruits, peanuts, dark green vege. Used as cofactor in carboxylation of pyruvate and acetyl CoA, works with B vitamins. It is involved in the biosynthesis of fatty acids, gluconeogenesis, energy production, the metabolism of the branched-chain amino acids (L-leucine, L-isoleucine, L-valine) and the de novo synthesis of purine nucleotides.
Defic: alopecia, seb derm, neuritis, dry skin, generalized erythematous scaly skin eruptions, alterations in mental status, myalgias, hyperesthesias, and anorexia occur. The rash may be distributed around the eyes, nose, mouth, ears and perineal orifices. The facial appearance associated with the deficiency, with the rash around the eyes, nose and mouth along with an unusual distribution of facial fat, is called biotin deficiency facies. In biotin deficient infants, the neurological findings are hypotonia, lethargy and developmental delay. In adults, the neurological findings are lethargy, depression, hallucinations and paresthesias of the extremities. Although clinical biotin deficiency in humans is rare, it does occur. Prolonged consumption of raw egg white, long-term total parenteral nutrition without biotin supplementation and malabsorption syndromes, such as short-gut syndrome, have resulted in biotin-deficiency states.Marginal biotin status may occur under certain conditions, e.g., during the first trimester of pregnancy, and it is thought that this situation may be teratogenic. Functional biotin deficiency occurs in certain genetic d/o’s. Biotin is the coenzyme for four carboxylases. Acetyl coenzyme A (CoA) carboxylase, found in both the mitochondria and cytosol, catalyzes the carboxylation of acetyl-CoA to malonyl-CoA.
Multiple carboxylase deficiency (MCD): two congenital d/o’s of biotin metabolism that lead to deficiency of the four biotin-dependent carboxylases. These two genetic d/o’s are essentially the result of a deficiency of biotinidase or holocarboxylase synthetase (HCS), two enzymes crucial to the biotin metabolism pathway. Biotinidase deficiency is associated with a slow but progressive loss of biotin in the urine, leading to the typical organic aciduria of multiple carboxylase deficiency.
Normal levels: 200-500 pg/ml (1500 pmol/L). Plasma and urine concentrations of biotin are diminished in the deficient state. Elevated urine concentrations of methyl citrate, 3-methylcrotonylglycine, and 3-hydroxyisovalerate are observed in deficiency
A bi-cyclic compound consisting of a uredio ring fused to a substituted tetrahydrothiophene ring. Most dietary biotin is linked to lysine, a compound called biotinyl lysine, or biocytin. The lysine must be hydrolyzed by an intestinal enzyme called biotinidase before intestinal absorption occurs. Acts primarily as a coenzyme for several carboxylases; each holoenzyme catalyzes an ATP-dependent CO2 transfer. The carboxylases are critical enzymes in carbohydrate and lipid metabolism.
Toxicity: not been reported in humans with doses as high as 60 mg/d in children.
Calcium: Links: Recommneded Intake | Ca Content of Foods | Ca Preparations & Adverse SE’s | IV Forms & Oral absorption | Blood Serum Calcium (Ca) | Vitamin D |
800-1500mg/d (see below). Found in milk, broccoli, sardines, clams, kale, turnip greens, mustard greens. Body contains 600 g, 99% in bones. Used for blood clotting, nerve and muscle function. Defic –> osteomalacia, tetany.
Normal = 8.6-10.8 mg/dL (2.2-2.7 mmol/L) if normal serum albumen. Need to take in 400-600 IU of Vit-D, intestinal absorption of Ca is not possible w/o Vit-D (does not need to be taken at same time). Calcium is an alkaline-earth metal with atomic number 20 and an atomic mass of 40.08 daltons. Its atomic symbol is Ca. Many elderly are not compliant with calcium supplementation (calcium carbonate, 600 mg BID), but those who are compliant have reduced risk for fx (associated with improved quantitative U/S of the heel and femoral neck, whole body DEXA and bone strength), according to the results of a 5-year, RCT (Arch Intern Med. 2006;166:869-875). Children from families with high-calcium diets show a lower risk for mortality from stroke later in life, according to a 65-year follow-up study on 4400 children from England and Scotland working class families (Heart 2009;online-first 26 July).
Recommended Calcium Intake in mg/day: Start in pre-adolescence to incr peak bone mass. Diary products are the best source. Need spread out pills as can only absorb a max of 500-600mg at one time.
Infants, first 6 mo’s of life–> 400.
Infants, 7 to 12 mo’s–> 600.
Children 1-10 years–> 800.
Adolescents and young adults (11-24yo)–> 1200 – 1500. Calcium supplementation (1000 mg calcium carbonate/day) in adolescent girls may increase total BMD, an effect that is sustained over time during puberty (Am J Clin Nutr 2005;81:168-188).
Women 25-50 years –> 1000.
Women pregnant or nursing–> 1200 – 1500.
Women 51-65 taking estrogens–> 1000.
Women 51-65 not taking estrogens–> 1500.
Women >65 years of age–> 1500.
Men 25 – 65 years–> 1000.
Men >65 years–> 1500.
• For maintaining calcium metabolism, intake of calcium levels >800 mg/d is probably unnecessary provided that Vit-D status is adequate (JAMA 2005;294:2336-2341) (serum PTH levels rose as serum 25-hydroxyVit-D levels fell).
• A US Preventive Services Task Force (USPSTF) recommendation statement has concluded that the evidence is insufficient to support the use of vitamin D and calcium supplementation to prevent fractures among community-dwelling men and premenopausal women (Ann Intern Med. Published online February 25, 2013). However, the task force did find sufficient evidence to recommend against daily vitamin D and calcium supplements for the primary prevention of fractures in postmenopausal women.
PP: Dietary Ca is complexed with proteins and anions like phosphate, citrate, carbonate. Gastric acid is needed for dissociation of Ca from anionic components of food and Ca salts. The role of PTH is as important as Vit.D. PTH promotes 1,25(OH)2D secretion which primarily increases Ca absorption.The neg. feedback mechanism of Serum Ca and PTH is so fine to the point that the range of Total Serum CA is bet. 8.5-10.5 mgs, but the most important component is the ionized Ca of 4.4-5.2.The protein bound and complex fractions are not regulated by PTH nor by 1,25OH D.The purpose of a constant level of ionized Ca in the extracellular fluid is to provide adeuquate amounts of Ca to cells, to bone and for renal excretion.Receptors for PTH and Vit D are found in bones, kidney and intestine. Ca citrate could be given with meals or divided doses.
• Dietary calcium may be important in the regulation of energy metabolism as a study suggest that high-calcium diets lead to inhibition of adipogenesis and enhanced insulin sensitivity via a mechanism mediated by the signaling protein S100A16 (Metabolism Clin Exp 2012;61:157-163). ..”High-calcium diets may lead to nuclear exclusion of S100A16, which results in the inhibition of adipogenesis and enhanced insulin sensitivity”.
1000mg Ca = 1qt milk (3 to 4 eight ounce [240ml] glasses), 2.7 lb of broccoli. It is generally recommended that calcium supplements be taken in doses of no more than 500 to 600 mg per dose to optimize absorption.
1 cup (8 oz) milk (whole or skim) or yogurt has ~300mg.
1 slice (1oz or 28g) swiss cheese = 260mg, american cheese = 175mg. 1 slice cheese pizza = 150mg.
½ cup of tofu or ¾ cup of Ca fortified cereal has 250mg.
1 oz cheddar or mozzarella or 6 oz of fortified orange juice has 200mg.
1 oz (28g) of Gruyere cheese or 10 figs has 280mg.
½ cup ice cream ~95mg.
½ cup cottage cheese = 90mg.
1 tsp powdered nonfat milk = 50mg.
1 cup broccoli = 175mg. 1 medium egg = 55mg.
Canned salmon (3 oz = 90g, with bones) = 200mg.
Sardines in oil (with bones, 3oz, 90g) = 370mg.
½ cup of collards has 175mg.
1 cup low fat cottage cheese = 154mg.
½ cup of mustard greens, kale or broccoli has 50mg. 4 oz tofu has 130mg. S
soy milk has 7mg, (80-300mg if fortified). ¼ a cup of roasted soybeans has 119 mg (88mg if boiled). Tempeh, ¼ cup has 77mg.
Collard greens (300 mg to 350 mg).
Cereal [up to 1000 mg].
Fortified fruit juice [225 mg to 300 mg].
Breakfast bars: often contain 200 mg to 500 mg.
Calcium Preparations: See Oral absorption & Interactions | Cardio Risks | Contra if hypercalcuria (Ur Ca excretion >300mg/24hr) that cannot be controlled with a thiazide. To minimized SE’s, best to take with food. Magnesium + calcium combos might be useful to counteract calcium’s constipating effect, but no evidence that magnesium also improves bone density (Prescriber’s Letter 2008;15:10)….additionally, there is no proof that vitamin K reduces fractures. Only 30% of calcium intake is normally absorbed regardless of dietary or supplement source (Mayo Clin Proc 2010;85:752-58)….ex if take 1,000mg, only absorb 300mg (body needs 50mg, a normal 24-hour Ur calcium excretion is then 100-250mg/d)…..with Vit-D deficiency, only 10% is absorbed.
SE: intestinal gas and constipation, more common with Ca-carb, less so with Ca-citrate. Hypercalcuria rare if dose is <2g/d.
Calcium content of the various calcium salts:
Calcium acetate: 253 mg (12.7 mEq) per g.
Calcium carbonate: 400 mg (20 mEq) per g.
Calcium chloride: 270 mg (13.5 mEq) per g.
Calcium citrate: 211 mg (10.6 mEq) per g.
Calcium gluceptate: 82 mg (4.1 mEq) per g.
Calcium gluconate: 90 mg (4.5 mEq) per g.
Calcium glycerophosphate: 191 mg (9.6 mEq) per g.
Calcium lactate: 130 mg (6.5 mEq) per g.
Calcium phosphate dibasic anhydrous: 290 mg (14.5 mEq) per g.
Calcium phosphate dibasic dihydrate: 230 mg (11.5 mEq) per g.
Calcium phosphate tribasic: 400 mg (20 mEq) per g.
Ca-Carbonate (Tums, Os-Cal, Oyst-Cal, Caltrate, Gencal, Calci-Chew): 500mg Ca. Highest % of elemental Ca (40%) by weight. Most have 200mg Vit-D except Tums, which has none. Best taken with meals as absorbed in acid environment. SE: gas and bloating, lowers Thyroxine absorption. Avoid oyster-shell or bone meal preparations as impure, containing possible contaminants (lead or mercury) (Caltrate 600, Eckerd, Nature Made). Absorption may be impaired in pt’s with high gastric pH (pt’s taking acid-suppressing drugs and the elderly. Prolonged use of large doses of calcium carbonate, >12 g/d (~5 grams of elemental Ca)– may lead to the milk-alkali syndrome, nephrocalcinosis and renal insufficiency. Calcium carbonate from oyster shell calcium and bone meal are only 28% to 31% elemental calcium. Cost, inexpensive $1-6.50/mo. Calcium from the carbonate salt is fully absorbable (Osteoporos Int 1999;9:19-23). Formulation of choice in patients with hyperphosphatemia in chronic renal failure due to good phosphate binding ability.
Ca-Citrate (Citracal): 21% elemental calcium. $8.50/mo. 1 caps contains 315mg Ca + 200 IU Vit D. Can take with or without food. May have better absorption than calcium carbonate, especially in patients with higher gastric pH as it’s absorption is less dependent on the presence of gastric acid. Good for elderly pt’s and those on H2 blockers or proton pump inhibitors. Can enhance intestinal absorption of aluminum. Avoid in patients with end-stage renal disease.
Ca-citrate malate: 24% elemental calcium. Citrate form is best if h/o renal stones.
Ca-lactate: 13% elemental calcium. 325 & 650 mg/tab with 42 & 84 mg Ca2+/tab. A large number of tablets (12-24/d) are required for a therapeutic effect.
Ca-Phosphate = Tribasic (Posture): 39% elemental calcium, avoid if renal failure. 1565 mg/tab has 600mg Ca2+/tab. $6/mo
Ca-glubionate (Neo-Calglucon): comes in a syrup (5 mL syrup) @188 mg/tsp (115mg Ca2+/tsp), good for kids. 6.5% elemental calcium.
Calcium Glucarate (Ca D-glucarate): 12% Elemental Calcium. Multiple doses need to be taken to get sufficient amount of elemental calcium. Promoted to rid body of toxins. Calcium D-glucarate is thought to decrease estrogen levels by affecting estrogen’s elimination. Though there is interest in using calcium D-glucarate for preventing estrogen-related cancer such as breast cancer and other hormone-related cancers, there is not enough evidence to support its use for this purpose.
Coral Calcium: primarily Ca-Carbonate with magnesium and other trace minerals. Not any more effective than other Ca, costs 3X as much. Calcium of coral origin may be better absorbed from the intestine than calcium of calcium carbonate origin on the average (J Nutr Sci Vitaminol (Tokyo) 1999;45: 509-17). On June 9, 2003, the U.S. FTC charged the marketers of Coral Calcium with making false claims about the product’s health benefits (http://www.fda.gov/oc/whitepapers/chbn_summary.html). One of the promoters of Coral Calcium is Kevin Trudeau, who hosts the infomercial that has sold millions of dollars worth of this. Trudeau is a twice-convicted felon for credit card fraud and larceny. He has been the subject for multiple fines and injunctions for false advertising. Coral Calcium’s only real claim is that it is certainly the world’s most expensive calcium supplement (/www.quackwatch.org).
Ca- Acetate (Calphron, PhoLo): tabs, 667mg (169 mg Ca2+/tab):2 tabs with each meal. May need 3-4 tabs per meal to lower phosphate to < 6 mg/dL, as long as hypercalcemia does not occur. For control of hyperphosphatemia in end-stage renal disease. Does not promote aluminum absorption. Calcium acetate taken with meals combines with dietary phosphate to form insoluble calcium phosphate that is excreted in the feces.
Taking magnesium (Mg) along with calcium?: Some claim that Mg helps boost calcium absorption or works better than calcium alone to build bones, but this isn’t true if Mg levels are adequate. Mg can have a laxative effect, this might help people who get constipation from taking calcium (>350 mg Mg can cause diarrhea). The RDA for Mg in age >30 is 420 mg for men and 320 mg for women. Avoid if impaired renal function (Pharmacist’s Letter/Prescriber’s Letter 2004;20:201205).
Commercial Products:
Citracal Slow Release 1200: 1 tab qd with 1200mg Ca + 1,000 IU Vit D3.
Viactive: soft flavored chew, with Vit-D and K. 500mg.
One-A-Day: Bone strengths and Calcium plus give 500mg. Calcium (1,000mg qd) and Vit-D3 (800 IU qd) supplementation do not reduce fx’s in those at risk (s/p a recent low-trauma fx, any previous fx, low body weight (<58 kg), smoking, FHx of hip fx or fair or poor self-reported health), according to the results of two studies with >8,000 pt’s (BMJ. 2005;330:1003-1006 and Lancet. Posted online April 28, 2005). Only 55-60% of pt’s were taking their supplement at 2 years.
Bone meal: composed of finely crushed, processed bone, usually from cattle but sometimes also from horses. Bone meal was at one time a popular nutritional supplement for calcium, but they contain substantial amounts of lead, as well as other toxic elements, such as arsenic, mercury and cadmium.
How Much is Too Much? Calcium intake of >2500 mg daily may increase the risk of hypercalcemia and resulting renal impairment (Menopause 2006;13:862-77)…kidney stones are associated with calcium intake >2150 mg daily. Excess calcium can impair absorption of iron, zinc, magnesium, and phosphorus.
Cardio Risks: The best source of calcium remains diet and the consumption of calcium-rich foods such as low-fat dairy, beans, and green leafy vegetables.
Are Calcium Supplements Bad for the Heart?: Use of calcium supplements is associated with a near doubling of risk for myocardial infarction (HR, 1.86) but not stroke (HR, 1.05) or CV death (HR, 1.02)…. but calcium intake through diet does not confer increased risk according to data from nearly 24,000 German residents aged 35 to 64 with 11 years’ follow-up (Heart 2012;98:920-925)…..Editorialists note….”We should return to seeing calcium as an important component of a balanced diet and not as a low-cost panacea to the universal problem of postmenopausal bone loss.” Although this analysis does not prove a causal link, it seems prudent to rely predominantly on dietary calcium whenever possible, reserving calcium supplements for situations where their benefits clearly outweigh their risks.
• Calcium from food is not associated with a significant increase in cardiovascular risk (Prescriber’s Letter. 2013;20:4)…..Tell patients to meet calcium needs as much as possible from foods…such as low-fat dairy, green leafy vegetables, and beans.
• High supplemental calcium intake (>1000 mg) is associated with cardiovascular death according to data on 390,000 older adults (mean age, 61) in the NIH–AARP Diet and Health Study (JAMA Intern Med 2013:Feb 4;e-pub ahead of print)……elevated risk was only in men and only for death from heart disease……Compared with individuals who took no calcium, men who consumed 1000 mg or more of supplemental calcium per day had a significant 20% increased risk of CVD death, a risk that was driven by a significant 19% increased risk of heart-disease death. For women, however, there was no association between calcium intake and the risk of death.
• Calcium intake above 1400 mg a day was associated with increased risks for cardiovascular disease and mortality among women in a prospective longitudinal, population-based Swedish cohort study (BMJ 2013;346:f228)…..women who consumed 1400 mg or more of calcium daily (through diet or supplements) had 40% higher mortality, 51% higher cardiovascular mortality, and nearly double the ischemic heart disease mortality, compared with those who consumed 600 to 999 mg. Among women with 1400 mg daily intake, those who took calcium supplements had even higher all-cause mortality (adjusted hazard ratio, 2.57). The authors explain that serum calcium levels “are under tight homeostatic control” and do not normally correlate with the amount of calcium intake. However, low or very high intakes override this control, “causing changes in blood levels of calcium or calciotropic hormones.” He advised that one should not make recommendations on the basis of a single study, but emerging evidence suggests caution about high calcium intake. He also noted that a meta-analysis of randomized trials has shown that calcium supplementation actually increased the rate of hip fracture. “My present recommendation is to avoid calcium supplement use if you have a normal varied diet,” he said. “Having a healthy balanced diet and avoiding water filters that reduce calcium in drinking water is probably best.”
• A study has shown that calcium supplementation might increase vascular events in elderly women (Circulation 2007; 115:846-854)…..”The trial was primarily looking at what calcium supplements do to bone density, but we had a secondary hypothesis right from the outset that calcium might actually prevent heart attack. What we found, to our surprise, was that we didn’t see a decrease but an increase, and the findings appear to be quite robust.”…High calcium uptake might accelerate calcification of arteries?….”if you are in the older age group and are known to have heart disease, it’s probably not sensible for you to take a calcium supplement. In younger people, calcium supplements look reasonable, but it may be sensible to aim for a smaller dose, say 500 mg/day.”
• Calcium supplementation may adversely affect cardiovascular health in older women according to a RCT in New Zealand with 1500 postmenopausal women on either 1 g of calcium (Citracal; two tablets, each containing 200 mg elemental calcium qAM and 3 q PM) or placebo daily (BMJ 2008;15 January, doi:10.1136/bmj.39440.525752)(NNT = 50 to prevent one symptomatic fracture over 5 years — and an NNT of 44 to cause one MI, 56 to cause one stroke, and 29 to cause one cardiovascular event)….the risk of MI with calcium supplementation could outweigh any benefits on bone from calcium supplements. Calling their data “not conclusive,” the researchers nonetheless recommend that until definitive studies are done, “this potentially detrimental effect should be balanced against the likely benefits of calcium on bone, particularly in elderly women.” ……..barely achieved statistical significance……Until larger prospective trials are conducted to establish the true cardiovascular risk, if any, of calcium supplementation in these patients, clinicians should weigh these possible risks against the presumed beneficial role of calcium in preventing osteoporosis….. An editorialist states “they have overstated their data by emphasizing a nonsignificant trend and by deemphasizing the equivocal nature of their results and the need for further study. Women and their clinicians should not panic about the increased CV risk from calcium supplements suggested in this study”.
• Calcium supplementation (500 mg daily or greater) without vitamin D supplementation is associated with a 30% increased risk of myocardial infarction (HR 1.27) according to a meta-anaysis with almost 12,000 pt’s (BMJ 2010;341:c3691)…..treating 69 patients with calcium 500 mg or more for 5 years will cause one additional myocardial infarction (treating 1000 people with calcium supplements for 5 years would prevent only 26 fractures but would cause an additional 14 MIs)…..vs treating 50 healthy postmenopausal women for 5 years with calcium 1000 mg daily will prevent one fracture (BMJ 2008;336:262-6).
• Calcium (1 g), with or without Vit-D (400 IU), raises the risk for adverse cardiovascular events according to reanalysis of WHI data (BMJ 2011;342:d2040)…Vascular calcification is one proposed mechanism…..a composite of MI or stroke, compared with placebo (relative risk, 1.2 for each outcome). A meta-analysis of nine trials that involved 28,000 participants showed that calcium or calcium and vitamin D supplementation significantly raised risks for MI and a composite of MI or stroke compared with placebo (RR, 1.2 for each outcome).
Possible mechanisms: calcium supplements acutely elevate serum calcium levels possibly accelerating vascular calcification, which is predictive of vascular event rates. The trend to more frequent cardiac events in the calcium group does not seem to be secondary to changes in lipids or other risk factors, since calcium supplementation was associated with beneficial trends in levels of HLD and LDL cholesterol. Other possible mechanisms include an increase in vascular calcification or coagulability or altered vascular flow.
Advice: Evidence suggests that calcium supplements double heart attack risk…but calcium in food does not (Prescriber’s Letter 2012;19:7)…Supplements may cause a spike in calcium levels…possibly leading to atherosclerosis or clots…..advise patients not to overdo it with calcium supplements…and to try to get most or all of their calcium from food…..aim for a total of 1000 mg/day for women up to 50 and men up to 70…and 1200 mg/day for older adults….To figure out dietary calcium, have people count 300 mg/day from all NONdairy foods…plus 300 mg per cup of milk, fortified juice, etc. Continue to advise people to use calcium supplements if needed…but not to exceed recommended amounts. Tell people to consider their total calcium intake from supplements plus foods. Most of the studies in the meta-analysis weren’t designed to collect cardiovascular risk or outcomes. Plus patients were taking calcium ALONE…without vitamin D. Low vitamin D may increase cardiovascular risk.
• Calcium supplementation is safe, effective, and necessary in a society where the majority of people do not get enough calcium, and concerns of potential cardiovascular risks related to supplementation are based on somewhat inconclusive data (American Society for Bone & Mineral Research 2011 Annual Meeting; Calcium Supplementation Debate. September 17, 2011)…….”Tailored daily supplementation with calcium and vitamin D is a safe, effective, and relatively cheap method of fracture prevention in elderly women.”
• High calcium intake (>1400 mg/day) was associated with earlier mortality in women according to a prospective cohort study from Sweden (BMJ 2013;346:f228)……Median follow-up was 19 years. Compared with dietary calcium intakes of 600 to 999 mg daily, daily intakes of =1400 mg were associated with significantly higher rates of death from all causes (multivariate adjusted hazard ratio, 1.4), CV disease (AHR, 1.5), and ischemic heart disease (AHR, 2.1), but not from stroke. Similar results were obtained for total calcium intake. Vitamin D intake did not modify the associations.
IV Ca Forms and Oral absorption issues:
Ca-gluconate: soluble, but give less Ca per tablet as 9% elemental calcium. 10% soln in amps and vials. 10 mL contains 1 g (90 mg Ca2+) of calcium gluconate. IV for acute hypocalcemic crisis (tetany, laryngospasm, or seizures) or severe hypocalcemia with sx’s or hyperkalemia with ECG changes. Seldom used orally because of its low calcium content. In adults in acute hypocalcemic crisis, 10-20 mL calcium gluconate may be given over 10 min IV. In children, the dosage is 2 mg/kg elemental calcium. In adults with severe hypocalcemia, a continuous IV infusion, containing 5-6 amps (10 mL of 10% soln/amp) of calcium gluconate/L of IV fluid, may be given at a rate of 100-125 mL/h. In hyperkalemia with ECG changes, 5-10 mL of a 10% soln of calcium gluconate is injected over 2 min IV. This dosage may be repeated in 5 min.
Ca-Chloride (CaCl2): 10 mL soln in amps, vials, & syringes that contain calcium: 1 g CaCl2 (272 mg Ca). For symptomatic hypocalcemia, ECG changes and/or cardiac dysfunction. The usual IV dose is about 500 mg. The rate at which it is given should not exceed 1 mL/min. This compound is very irritating and may cause severe necrosis and sloughing if extravasated, thus calcium gluconate is preferable.
Ca-Gluceptate: 5 mL has 220 mg/mL (18 mg Ca2+/mL), for IV or IM administration of calcium. In adults, 5-20 mL IV or 2-5 mL IM into the gluteal region or lateral thigh.
Absorption of Calcium: two mechanisms are involved in intestinal calcium transport. Calcium is absorbed in the duodenum and jejunum via an active transport that depends on 1,25-dihydroxy Vit-D [1,25-(OH)2 Vit-D]. At higher calcium intakes, passive diffusion in the jejunum and ileum is significant. The general absorptive efficiency of calcium is generally < 50% (~ 0.45 at intakes of 200 mg of calcium per day), and there is an inverse correlation between calcium intake and absorption fraction. Absorptive ability decreases with age and loss of estrogen at menopause. Absorption of calcium from dairy foods is generally good, and calcium is absorbed equally well from milk and yogurt. The absorption of calcium from spinach is poor, because most of the calcium is complexed with oxalate. Potentially toxic levels of lead were reported in supplements derived from bone meal, dolomite, and oyster shell. Absorption of calcium from whole milk, chocolate milk, yogurt, imitation milk (from dairy and nondairy products), cheese, and calcium carbonate was similar in 10 healthy postmenopausal women. Other studies have indicated that calcium citrate is absorbed more readily than calcium carbonate in doses of 0.2, 0.5, 1, and 2, g, however.
SE: Most pt’s tolerate calcium supplements without problems; however, nausea, dyspepsia, and constipation may limit adherence and may necessitate the substitution of different calcium salts.
Can interfere with absorption of other nutrients such as fluoride, iron, zinc, atenolol, propranolol, salicylates, bisphosphonates, and tetracycline’s. **Calcium interferes with thyroid hormone absorption, best to take Synthroid upon rising, 30-45min before breakfast, take the Ca with lunch or dinner. The proton pump inhibitor omeprazole reduces calcium absorption from the gut (Am J Med 2005;118:778-781) (radiolabelled calcium carbonate absorption was decreased from an average of 9.1% while on placebo to 3.5%). The small effect of calcium supplementation on bone mineral density in the upper limb is unlikely to reduce the risk of fx, either in childhood or later life, to a degree of major public health importance (BMJ. 2006;Epub ahead of print).
Choline: used for brain, organ and muscle function. Adult men and lactating women need 550 mg/d. Pregnant women need 450mg/d and Other women need 425mg/d. The typical adult diet gives 1g/d of choline as it is present in a variety of foods. High amounts in liver, eggs, wheat germ, dried soybeans and pork. Choline is a precursor for acetylcholine, phospholipids, and betaine. Choline is necessary for the structural integrity of cell membranes, cholinergic neurotransmission, lipid and cholesterol metabolism, and transmembrane signaling. Choline is thought to be a “conditionally essential” nutrient, in that de novo synthesis occurs in the liver and is < the vitamin’s utilization only under certain stress conditions.
Defic: seen in pt’s receiving parenteral nutrition devoid of choline. Deficiency results in fatty liver and incr LFT’s. The dx of choline deficiency is made on the basis of low plasma levels.
Toxicity: results in hypotension, cholinergic sweating, diarrhea, salivation, and a fishy body odor. The upper limit for choline has been set at 3.5 g/d.
Essential for mitochondria, a lipophilic substance involved in electron transport in mitochondria, 40% HTN and 60% CAD are deficient. Takes 4-6 weeks to lower BP @50-150mg BID. 100mg/d may improve EF. Insufficient evidence to recommend. Fairly safe drug. See “Dietary Supplements” in Compendium chapter.
An amino acid (methyl guanidine acetic acid). Not routinely incorporated into proteins. Endogenously synthesized from glycine, arginine and methionine. Taken orally, it will increase total muscle creatinine 20%, with 20% of that increase in the form of creatinine phosphate. Increases energy substrate to muscle in order to delay fatigue. May increase power and strength. Increases wt due to water retention (not muscle), may cause dehydration, cramps and strains.
95% is in skeletal muscle as phosphocreatine, supports synth of ATP, may or may not help in recovery of muscle strength or improve performance, yet incr in body weight (fluid retention and/or stim Protein synthesis). Naturally in meat, milk and some fish (½# raw meat has 1g creatine). Gain 1-3# in first week, then 10# by 6wks. Used for intermittent high intensity exercise (soccer, basketball).
Load dose of 5g QID for 5-7d, then 2-3g/d maintenance. (should use BW dose of 0.3g/kg load, .03g/kg maint), monitor LFT’s and BUN/Cr. The safest form is the monohydrate powder, which is usually mixed with 4-8 oz of juice. When stopped creatine levels rapidly decrease in 4-12 days to normal levels. No known serious adverse effects. 25% of people do not respond to high muscle creatinine levels.
Lutein: a carotenoid found in green and yellow veges. Some studies show benefit in cataract and macular degeneration. 6mg/d.
Helps metab FA’s by transporting free fatty acids into mitochondrial cytosol for oxidation. Normally synthesized in the liver from Lysine.
S/s: weakness, fatigue, cramps. Essential to supplement if deficient. However w/o the genetic d/o, there is little to no loss from skeletal m during high or low intensity exercise. Even massive doses increase levels by only 1-2%.
Carnitine Deficiency:
Primary systemic carnitine deficiency is a very rare genetic disorder that typically presents in infants.
Secondary carnitine deficiency may present in infants, children, and adults. Factors contributing to carnitine deficiency may include inborn errors of metabolism, fanconi syndrome, chronic renal dialysis, carnitine-deficient diet, extreme prematurity, malabsorption, HIV infection or antiretroviral therapy, valproic acid and a ketogenic diet.
Tx: Levocarnitine Oral Solution (Carnitor SF): [1-g/10 mL-oral solution] In infants and children the dose ranges between 50 and 100 mg/kg/day in divided doses to a maximum of 3 g/day. Therapy should be initiated at a dose of 50 mg/kg/day and uptitrated according to clinical response. For adults, dosage should start at 1 g (10 mL) a day and be increased slowly while assessing tolerance and therapeutic response. Monitoring should include periodic blood chemistries, vital signs, plasma carnitine concentrations, and overall clinical condition. SE: nausea, vomiting, body odor, gastritis, and seizures. Sugar-Free fersion FDA approved in 3/07 to treat primary systemic carnitine deficiency and for the acute and chronic tx of secondary carnitine deficiency because of an inborn error of metabolism.
Androstenedione: androgen derived from plants at 100-300mg/d. In its natural form it is produced by the adrenal glands and gonads. It may increase muscle mass and serum testosterone levels. SE: decr HDL, behavioral changes, acne, testicular atrophy, premature closure of epiphysial plates.
L-Carnitine (Levocarnitine, Carnitor): [330, 500 mg tabs. 250 mg caps. Oral solution: 100 mg/mL (118 mL). Injection: 200 mg/mL (5mL)]
Primary carnitine deficiency Tx:
Oral: Child @ 50–100 mg/kg/24 hr PO divided Q8–12 hr; increase slowly as needed and tolerated to max. dose of 3 g/24 hr. Adult @ 330 mg to 1 g/dose BID–TID PO. Mix with juice or liquids.
IV: Child and adult @ 50 mg/kg as loading dose; may follow with 50 mg/kg/24 hr IV infusion; maintenance: 50 mg/kg/24 hr divided Q4–6 hr; increase to max. dose of 300 mg/kg/24 hr if needed. Depletion is common in those on hemodialysis, some give 2g IV with each dialysis.
SE: May cause nausea, vomiting, abdominal cramps, diarrhea, and body odor. Seizures have been reported in pt’s with or without a history of seizures. Give bolus IV infusion over 2–3 min.
50-200 mcg/d. 6mg in body, used as part of glucose receptor and may have glucose-regulatory activity. The American Diabetes Association asserted in 1996 that “chromium supplementation has no known benefit in pt’s who are not chromium deficient.” Some pt’s on long-term parenteral nutrition have developed chromium deficiency and diabetic sx’s that were reversed with chromium supplementation. In general, plasma chromium levels are about 40% lower in diabetic subjects, compared with healthy individuals.
Defic: glucose intolerance.
Normal levels: 2-4ng/ml (35-73 nmol/L) plasma. Element #24. Dietary intake should be 50-200 mcg/d. Usually combined with picolate to increase GI absorption.
Deficiency: may cause anemia, chromosomal damage, cognitive impairment and interstitial nephritis. Has been reported to cause glucose intolerance, peripheral neuropathy, and confusion. Low chromium concentrations are associated with an increased risk of nonfatal myocardial infarction (Am J Epidemiol 2005;162:157-164).
Sources: corn oil, clams, whole grain cereals, meats, brewers yeast, liver, American cheese, wheat germ, alfalfa, apples with skins, brown sugar, carrots, potatoes. Also in spices (black pepper, thyme), mushrooms, brown sugar, coffee, tea, beer, wine. Fruits and vegetables are generally poor sources of chromium, as are most refined foods.
Intake: adults is 50 to 200 g/d. Adequate intake values for chromium in adults is 35 mcg/day in men and 25 mcg/day in women. Chromium in the trivalent state is found in supplements and is largely nontoxic; however, chromium-6 is a product of stainless steel welding and is a known pulmonary carcinogen, as well as causing liver, kidney, and central nervous system.
No proven benefit unless deficient. Deficiency seen with long-term TPN. Advice to diabetics: it is inexpensive, can try adding 300-1000 mcg/d once BS is stable on traditional meds, if see no measurable improvement in diabetics parameters, then stop taking.
Toxicity: Hexavalent chromium is corrosive and sensitizing. Workers in the chromate and chrome pigment production industries have consistently had an excess risk of lung cancer.
Chromium is a metal with atomic number 24 and an atomic mass of 52 daltons. Its symbol is Cr. It occurs in nature chiefly as a chrome-iron ore. Chromium exists in several valence states, of which the trivalent and hexavalent states are the most common. Most chromium in the food supply is in the trivalent state. Hexavalent chromium compounds are recognized as toxic and are potential carcinogens. Chromium is found in many foods, typically in small amounts. Chromium is a steel-grey, lustrous metal; odourless, available as lumps, granules, powder or high purity single crystals. It is a component of stainless steels and high temperature alloys; coating on metal and plastic (electroplated from solutions of chromium salts); synthesis of inorganic pigments; manufactured metal goods. Upon inhalation, the metal dust appears to have low toxicity, can probably cause coughing and mild temporary irritation (non-specific dust effects). It is not irritating to the eyes except as a “foreign object”. It is practically non-toxic by ingestion and is not absorbed into the body.
Chloride is the most abundant extracellular ion (80g in body). It is closely related to Na metabolism. Chloride is an inorganic anionic halogen with an atomic weight of 35.5. It is distributed exclusively within the extracellular fluid compartment. Normal serum chloride concentrations range from 96 to 106 mEq/L.
Requirements: adult –> 90-120 mEq/d. Child–> 5-7 mEq/kg/d. The normal serum range of chloride is 96-109 mmol/L. Changes in plasma chloride levels can occur with changes in hydration and acid-base balance. Urine chloride levels are helpful in the evaluation of metabolic alkalosis. Low urine chloride (<10 mmol/L) is present with chloride-responsive causes of alkalosis, such as vomiting with volume depletion. Elevated levels of urine chloride (>20) are present in conditions associated with mineralocorticoid excess, such as hyperaldosteronism and hypercortisolism.
Sources: table salt, seafood, milk, meats, eggs.
Defic: metabolic alkalosis. Nl: 89-106 mEq/L.
ICD-9 Codes: 276.9 Electrolyte and fluid d/o’s not elsewhere classified – chloride
Conditions Associated with Hypochloremia: Total body chloride depletion. Inadequate NaCl intake. Losses of GI fluids. Vomiting. Nasogastric suction. Small bowel fistulas. Burns. Renal (diuretic abusers, salt-losing nephropathy, interstitial nephritis). Adrenal insufficiency. Dilutional (decreased chloride concentration). Increased effective circulatory blood volume. Hypertonic infusions. Hyperglycemia (early stages). Normal effective circulatory blood volume. Pathologic water drinkers. Intrinsic renal diseases. Hypothyroidism. Syndrome of inappropriate antidiuretic hormone (SIADH). Drugs (Barbiturates, Chlorpropramide, clofibrate, Morphine, Nicotine, Tricyclics). Decreased effective circulatory blood volume such as edema states, congestive heart failure, cirrhosis of the liver or nephrotic syndrome. Compensated respiratory acidosis. Metabolic alkalosis.
Conditions Associated with Hyperchloremia: Loss of electrolyte free fluids (pure water loss) such as skin losses, fever, hypermetabolic states, increased ambient room temperature. Inadequate water intake. Loss of thirst perception. Renal losses. Central diabetes insipidus. Nephrogenic diabetes insiuidos. Loss of hypotonic fluids (water deficit in excess of sodium and chloride deficits). Diarrhea. Burns. Renal losses. Osmotic diuresis. Diuretics. Postobstructive diuresis. Intrinsic renal disease. Sodium gain. Administration of 3 to 5% NaCl. Saltwater drowning. Saline abortion. Hyperchloremic metabolic acidosis. Renal tubular acidosis. Interstitial renal disease. Multiple myeloma. Idiopathic. Drugs (carbonic anhydrase inhibitors such as acetazolamide or topical sulfamylon acetate and metabolites). Small bowel diarrhea. Ureteral diversion procedures. Ureterosigmoidostomy. Ileal bladder. Ileal ureter. Administration of acidic salts. NH4Cl. Arginine HCl. Lysine HCl. Hyperalimentation. Early renal failure. Primary hyperparathyroidism. Recovery from diabetic ketoacidosis.
Rx Products: Solution: 0.45% (77 mEq/L sodium, 77 mEq/L chloride). 0.9% (154 mEq/L sodium, 154 mEq/L chloride). 3% (513 mEq/L sodium, 513 mEq/L chloride). 5% (855 mEq/L sodium, 855 mEq/L chloride). Concentrated solution: 14.6% and 23.4% sodium chloride. Injection: 0.9% sodium chloride.
OTC Products: 0.45% sodium chloride or 0.9% sodium chloride.
Indications:
0.45% and 0.9% flexible plastic containers: Parenteral replenishment of fluid and sodium chloride.
0.9% syringe: For use in flushing the indwelling venipuncture device where the medication to be administered is incompatible with heparin.
0.45% and 0.9% vial: For diluting or dissolving drugs for intramuscular, IV, or subcutaneous injection, or for inhalation according to instructions of the manufacturer of the drug to be administered. Also flushing of intravenous catheters and for tracheal lavage.
3% and 5% concentrates: Sources of electrolytes and water in hyponatremia and hypochloremia.
14.6% concentrate: Electrolyte replenisher in parenteral fluid therapy; IV sodium supplement in hyponatremia; additive for TPN; additive for carbohydrate-containing IV fluids.
23.4% concentrate: As an additive in parenteral fluid therapy. Strongly hypertonic and must be diluted prior to administration.
Dosage: IV: In the average adult, daily requirements of sodium and chloride are met by the infusion of 1 L of sodium chloride 0.9% (154 mEq each of sodium and chloride). Base fluid administration on calculated maintenance or replacement fluid requirements.
IV catheters (0.9%) – Prior to and after administration of the medication, entirely flush with preservative-free 0.9% sodium chloride for injection.
Calculation of sodium deficit – To calculate the amount of sodium that must be administered to raise serum sodium to the desired level, use the following equation (TBW = total body water): Na deficit (mEq) = TBW (desired – observed plasma Na).
Base the repletion rate on the degree of urgency in the patient. Use of hypertonic saline (eg, 3% or 5%) will correct the deficit more rapidly.
3% and 5% concentrates: Do not use plastic container in series connection.
When administered peripherally, maximum IV dosage should be 100 mL given over a period of 1 hour. Before additional amount is given, evaluate the need for more sodium chloride. IV administration of these solutions should not exceed 100 mL/hour or 400 mL/24 hours.
3 mcg/d. Sources are wholemeal flour, seafoods, shellfish, liver, kidney, poultry, milk, and veges (depending on soil). There is ~80ug in body, used as a cofactor in B12. Intakes of cobalt are ~ 5 µmole/day.
Defic: no known. Normal levels: 2-5 ng/ml.
Toxicity: cobalt chloride used as a fortifier in beer has led to outbreaks of fatal cardiomyopathy among heavy consumers.
Found in liver, shellfish, whole grains, cherries, legumes, kidney, poultry, oysters, chocolate, nuts/seeds, bran, and organ meats. Drinking water from copper piping. Whereas milk is a very poor source. 100mg in body, used as cofactor in lysyl oxidase for collagen synthesis and in cytochrome. Copper absorption likely occurs in stomach and proximal duodenum. Zinc induces negative copper balance.
Recommended Dietary Allowance (RDA):
340 mcg/day for children aged 1-3 yo. 440 mcg/day for children aged 4-8 yo.
700 mcg/day for children aged 9-13 yo. 890 mcg/day for adolescents aged 14-18 yo.
900 mcg/day for adults e 19 yo. 1,000 mcg/day if pregnant. 1,300 mcg/day for lactating.
Normal levels: 90-130 mcg/dL (14-20 umol/L). Deficiency is reliably detected by diminished serum copper and ceruloplasmin concentrations, as well as by low erythrocyte superoxide dismutase activity. Absorbed by a specific intestinal transport mechanism. It is carried to the liver, where it is bound to ceruloplasmin, which circulates systematically and delivers copper to target tissues in the body. Excretion of copper is largely through bile into feces.
Toxicity: absorption of copper salts applied to burned skin. Milder manifestations include nausea, vomiting, epigastric pain, and diarrhea; coma and hepatic necrosis may ensue in severe cases. Toxicity may be seen with doses as low as 70 mug/kg/d. Chronic toxicity is also described. Wilson disease is a rare, inherited disease associated with abnormally low ceruloplasmin levels and accumulation of copper in the liver and brain, eventually leading to damage to these two organs. It is due to mutations in the copper-transporting ATP7B gene.
Defic: Normal serum copper 0.75-1.45 mcg/mL (11.8-22.8 mcmol/L). Deficiency is a rare condition due to copper’s ubiquitous distribution and low daily requirement but becoming more common with increasing bariatric surgeries.
Risks of Def: patients following gastric surgery (gastrectomy for peptic ulcer surgery, bariatric surgery). Patients with GI malabsorptive conditions (celiac disease, cystic fibrosis, Crohn’s disease, small bowel resection). Malnourished children. Excess zinc ingestion, and long-term parenteral nutrition (TPN) without adequate copper supplementation. In many cases, the cause is not apparent. Has been observed in premature and low-birthweight infants fed exclusively a cow’s milk diet. Patients with Menkes disease caused by mutations in copper-transport gene (ATP7A) (NEJM 2008;358:605).
S/s Defic: Get anemia, neutropenia, osteopenia in children, depigmentation of skin and hair, neurologic disturbances (similar to B12 def). Hypochromic, normocytic (or microcytic due to impaired iron absorption or macrocytic also seen) anemia, often accompanied by neutropenia and megaloblastic changes in BM (Myelodysplasia and myeloneuropathy and copper deficiency. Mayo Clin Proc 2005;80:943-46). Mental retardation and psychomotor abnormalities. Dx via low serum levels of copper (<65 g/dL) and low ceruloplasmin levels (<18 mg/dL). Hyperzincemia often occurs even in the abscence of exess intake. Acquired copper deficiency can be a cause of myeloneuropathy.
• Copper deficiency can cause myelopathy presenting with gait difficulty (sensory ataxia secondary to dorsal column dysfunction) and lower limb paresthesias (Mayo Clin Proc 2006;81:1371-84)…tx with 2g/day of elemental copper (using salts such as copper gluconate and copper chloride, but doses as high as 9mg/d have been used….soem Rx 6mg/d x 7 days, then 4mg.d x 7 days then 2mg/d x 6mo.
• A retrospective cohort study with 25 patients with copper deficiency myelopathy found that the chief complaint was gait difficulty, sometimes with mild spastic component (Mayo Clin Proc 2006;81:1371)…all patients reported lower limb paresthesias, other symptoms included upper limb signs or symptoms in 23 patients. Symptoms may be delayed 10-20 years after bariatric surgery before diagnosis of copper deficiency.
• Complications indclude anemia, neutropenia, myelopathy (or myeloneuropathy) with spastic gait and prominent sensory ataxia as well as peripheral neuropathy and optic neuropathy (Arch Neurol 2009;66:1025).
W/u: CBC, B12, serum folate level, serum methylmalonic acid, serum homocysteine, serum copper level, 24-hour urinary copper excretion, serum zinc level, serum ceruloplasmin, spinal MRI, bone marrow exam.
Dx: serum copper < 0.75 mcg/mL (11.8 mcmol/L). 24-hour urine copper excretion < 15 mcg consistent with copper deficiency. Typically see anemia and neutropenia, low serum copper, high serum zinc, low white cell count, low neutrophil count, low ceruloplasmin. Erythrocyte superoxide dismutase and platelet cytochrome-c oxidase may be more reflective of metabolically active copper and copper stores than plasma copper or ceruloplasmin (Am J Clin Nutr 1998;67(5 Suppl):1041S).
Ddx: vitamin B12 deficienc, iron deficiency, subacute combined degeneration of spinal cord, myelodysplastic syndrome, sideroblastic anemia, drug or alcohol toxicity.
Tx: copper supplementation with elemental copper 2 mg/day. Oral route preferred, but parenteral route may be needed. Cpper gluconate and copper chloride are commonly used copper salts (copper gluconate may have limited oral bioavailability). Discontinue zinc for cases of zinc-induced copper deficiency. Sample oral copper repletion protocol (based on dose of elemental copper) 8 mg/day for first week. 6 mg/day for second week. 4 mg/day for third week. 2 mg/day thereafter. Monitor serum copper levels and blood counts.
Prognosis: after copper supplementation, it usually associated with complete and prompt reversal of anemia and neutropenia, but residual neurologic deficits may remain, but usually stabilize. Neurologic decline may be prevented with copper supplementation.
ICD-9 codes:
269.3 mineral deficiency, not elsewhere classified
275.1 disorders of copper metabolism
790.6 other abnormal blood chemistry
ICD-10 codes:
D53.8 other specified nutritional anaemias
E61.0 copper deficiency
E64.8 sequelae of other nutritional deficiencies
E83.9 disorder of mineral metabolism, unspecified
R79.0 abnormal level of blood mineral
Vitamin D (Vit-D): The sunshine vitamin.
Links: PP | Serum Levels | Risks for Defic | Deficiency | Forms of Vit-D | Sources, (Diet & Sun) & PP & Toxicity | Rickets & Child | Calcium |
Vitamin D is a group of fat-soluble secosteroids responsible for intestinal absorption of calcium and phosphate. In humans, the most important related compounds of vitamin D are cholecalciferol (vitamin D3) and ergocalciferol (vitamin D2). Although vitamin D is commonly called a vitamin, it is not actually an essential dietary vitamin in the strict sense, as it can be synthesized in adequate amounts by most mammals exposed to sunlight. (Cats and dogs cannot synthesize vitamin D efficiently and must receive it in their diet.)
RDA: (in 2010) is 400 IU for infants, 600 IU for ages 1 to 70 and 800 IU for over 70. But these RDAs are based only on the amount needed to prevent rickets, osteomalacia, and fractures. Higher amounts of vitamin D are associated with a lower risk of falls, cancer, heart disease, autoimmune disorders, etc. Obtaining adequate levels of Vit-D is essential for health. There are only three sources of Vit-D — sunlight, food, and supplements. Dermatologists have taken the position that exposure to sunlight is not a good solution for the prevention of vitamin D deficiency, because of concerns about skin cancer and other adverse effects of ultraviolet radiation. The daily Vit-D intake should be 400-1200 U/day depending on the time of day, skin color of the patient and level of sun exposure (see below). The RDA is 200-400 IU/d, 5-10mg/d), 400 U/d in age 51-70, 600 IU/d if >70yo. Most of us don’t get enough Vit-D from food or sun exposure and most multivits don’t contain enough, either.
• The current recommended intakes are set high enough to prevent rickets…but not enough for most people to maintain healthy levels (Prescriber’s Letter 2009;25(5):250509)…Adequate Vit-D can reduce muscle and bone pain, falls, and fractures. Higher levels are also associated with a lower incidence of some cancers, heart disease, and other chronic diseases.
• The AAP recommend s supplementation with 400 IU/day of vitamin D is recommended for all infants, children, and adolescents who consume <1 L/day of vitamin D–fortified formula or milk (Pediatrics 2008;122:1142)…..Vit-D deficiency is associated with multiple sclerosis and type 2 diabetes.
• A meta-analysis suggests benefit at a Vit-D dose of >800 IU daily, but factors relating to treatment adherence could have biased the results (N Engl J Med 2012;367:40).
Institute of Medicine Recommendations on Vitamin D: (J Clin Endocrinol Metab 2010:Nov 29;e-pub ahead of print)
The committee concluded that vitamin D and calcium play critical beneficial roles in bone metabolism, but evidence is insufficient for health benefits of vitamin D in extraskeletal contexts (e.g., promotion of immune response; protection against cancer, cardiovascular disease, diabetes, and preeclampsia). Serum 25-hydroxyvitamin D levels of 20 ng/mL are sufficient to maintain adequate bone health, and dietary intake of 600 IU daily is enough to achieve adequate vitamin D stores in most individuals younger than 71; for those who are 71 and older, 800 IU daily is recommended. Although the mean intake of vitamin D in North American populations is less than this, the committee found that mean blood levels are 20 ng/mL, suggesting that the amounts of sun exposure received are sufficient to maintain adequate vitamin D levels. The committee cautioned against taking large doses of vitamin D (i.e., >4000 IU daily) because at such doses, harmful effects (e.g., renal and tissue damage) emerge.
• Many experts now recommend that adults get 1000 IU/day for bone health as most are getting less sun exposure. Vit- D nomenclature can be confusing, because the term “Vitamin-D” is used for both the final biologic product and its precursors. Vit-D is obtained from two sources, synthesis in the skin (the major source) and dietary sources. The best dietery sources is fortified milk (100 IU / 8oz or 240ml), milk products, oily fish, egg yolks, and fortified foods . Intestinal absorption of Ca is not possible w/o Vit-D (does not need to be taken at same time). The primary source of Vit-D in humans is sunlight. However, the effect of sunlight exposure and Vit- D synthesis is reduced in individuals with darker skin pigment or if wear Sunblock (>SPF 8). Essentially every tissue and cell has a Vit-D receptor; thus, optimizing Vit-D status likely improves overall health and well-being.
• The active form of Vit-D regulates more than 200 genes, many of which control cellular proliferation and differentiation, insulin and renin secretion, and innate immunity. Intake of ordinary doses of Vit-D supplements (mean daily dose of 528 IU, range 400-833 IU) seems to be associated with decreases in total mortality rates (7%) according to a meta-analysis of 18 RCT’s (Arch Intern Med. 2007;167:1730-1737)….the authors say may be via “inhibition of cellular proliferation and activation of cellular differentiation, could reduce aggressiveness of cancerous processes and expansion of atheromatous lesions.”
• Low vitamin D levels may raise the risk of death from any cause (Arch Intern Med 2008;168:1629-1637)…..increased all-cause mortality risk by 26% compared with optimal levels (below 17.8 versus above 32.1 ng/mL)…..analyzed data from 13,331 adults ages 20 and older in the nationally representative National Health and Nutrition Examination Survey (NHANES III).
• Research suggests that vitamin D may be beneficial to cancer patients as higher levels of vitamin D might lower the risk for colon, breast, endometrial, and prostate cancers (J Clin Oncol. 2009;Published online before print April 6).
• Vitamin D exposure (from cod liver oil, milk, vitamin supplements, and sun exposure) during adolescence and young adulthood protected against breast cancer, regardless of ER/PR status (Am J Epidemiol 2008;168:915).
• Higher vitamin D levels correlated with better muscle power and force in adolescent girls (J Clin Endocrinol Metab 2009;94:559)…..Median 25(OH)D level was 21.3 nmol/L. After adjustment for body weight, vitamin D levels were positively associated with jump velocity (P=0.002), jump height (P=0.006), fitness index (P=0.003), and force (P=0.04)……Because milk intake (a major source of vitamin D) by adolescents has decreased significantly during the last 20 years, supplementation with vitamin D might be necessary.
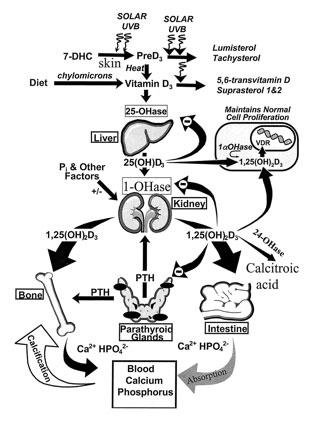 PP: Dietary Vit-D3 & Vit-D2 & 7-dehydrocholesterol in the skin are prohormones and is not known to have any intrinsic biological activity itself. UVB (290-315nm) activates 7-dehydrocholesterol to pre-vitamin D3. It is only after Vit-D3 is metabolized, first into 25(OH)D3 in the liver (liver adds OH), and then into 1a,25(OH)2D3 and 24R,25(OH)2D3 by the kidney (adds second OH), that biologically active molecules are produced.
PP: Dietary Vit-D3 & Vit-D2 & 7-dehydrocholesterol in the skin are prohormones and is not known to have any intrinsic biological activity itself. UVB (290-315nm) activates 7-dehydrocholesterol to pre-vitamin D3. It is only after Vit-D3 is metabolized, first into 25(OH)D3 in the liver (liver adds OH), and then into 1a,25(OH)2D3 and 24R,25(OH)2D3 by the kidney (adds second OH), that biologically active molecules are produced.
Step 1: The major biologic form of vitamin D, vitamin D3, is synthesized in the skin from the precursor (pre-D) under direct sunlight. In the skin, photoconversion (UV-A) of 7-dehydrocholesterol to Vit-D3 (Cholecalciferol) or dietary intake of Vit-D3. Some suggest that it’s a serious mistake to encourage the public to get intentional sun exposure to improve health when adequate Vit-D can be obtained through the diet. Yet, cutaneous synthesis of vitamin D3 from sunlight exposure is the major source (80% to 90%) of vitamin D in humans under natural conditions.
Step 2: Metabolism of Vit-D3 by the liver to 25(OH)D3 (= Calcidiol), which is the major form of Vit-D circulating in the blood compartment. It is hydroxylated into carbon-25 by 25-hydroxyVit-D-1a hydroxylase or CYP27B1, an enzyme located in the mitochondria of the hepatocyte.
Step 3: Conversion by the kidney of 25(OH)D3 [functioning as an endocrine gland] to produce the two principal dihydroxylated metabolites, namely 1a,25(OH)2D3 (= Calcitriol = Rocaltrol) and 24R,25(OH)2D3.
Step 4: Systemic transport of the dihydroxylated metabolites 1a,25(OH)2D3 and 24R,25(OH)2D3 to distal target organs.
Step 5: Binding of the dihydroxylated metabolites, particularly 1a,25(OH)2D3, to a nuclear receptor at the target organs followed by the subsequent generation of appropriate biological responses. The active form of Vit-D (1,25[OH]2 vitamin D) is bound to vitamin D–binding protein (DBP) in circulation, crosses the cell membrane, and binds to vitamin D receptor (VDR). The conjugated vitamin D with its receptor forms a heterodimer complex with retinoid X receptor (RXR) and with other factors, attaches to vitamin D–responsive elements on deoxyribonucleic acid, and alters gene expression.
25-hydroxyVit-D (Vit-D 25-OH) = 25(OH)D: the best indicator for determining adequacy of Vit-D intake since it represents the combination of cutaneous production and the oral ingestion of both Vit-D2 (ergocalcerferol or plant-based Vit-D) and VIT-D3.
• Supplemental vitamin D (400 IU to 4800 IU daily) enhanced calcium absorption very little among 163 postmenopausal women with mild vitamin D insufficiency (mean 25[OH]D level, 16 ng/mL) (J Clin Endocrinol Metab 2012;97:3550)….Participants ingested a standard dose of radioactive calcium, and serum radiocalcium was measured 2 hours later. At baseline, a mean 54% of ingested calcium was absorbed. After 1 year of vitamin D supplementation, the percent absorption rose by only about 3% on average, with trivial differences among the seven vitamin D dosages (range, 400–4800 IU daily). Moreover, among patients whose 25(OH)D levels exceeded 60 ng/mL after supplementation, calcium absorption was only 6% higher than in patients whose 25(OH)D levels reached only 20 ng/mL (58% vs. 52%). The authors conclude that calcium malabsorption occurs only when 25(OH)D levels are very low (<10 ng/mL); the likely reason is that levels of 1,25(OH)2D — the active metabolite of 25(OH)D that facilitates intestinal calcium absorption — don’t fall substantially until 25(OH)D levels are below 10 ng/mL.
Vit-D Levels: Serum 25-Hydroxyvitamin D [25(OH)D].
Normal levels: 20-100 ng/ml (25-200 nmol/L, to convert ng/ml to nmol/L, multiply by 2.496).
Optimal level: 30 to 60 ng/mL.
Insufficient: 11-20 ng/ml
Deficient: <10ng/ml (Mayo Clin Proc 2011;86:50-60). In the northern hemishphere, the lowest 25-hydroxyvitamin D levels tend to occur in March and the highest level in August. See Deficiency |
The serum concentration of this major circulating metabolite is the best indicater of systemic status, except in chronic renal failure, in which the impairment in renal 1-hydroxylation results in disassociation of the monohydroxy- and dihydroxyvitamin concentrations (measuring the serum concentration of the precursor, 1,25-dihydroxyVit-D is then necessary).
• According to one study, the most advantageous serum concentrations of 25(OH)D begin at 75 nmol/L (30 ng/mL), and the best range from 90 to 100 nmol/L (36–40 ng/mL) (Am J Clin Nutr. 2006;84:18-28) (adults need ~1000 IU (40 µg) Vit-D (cholecalciferol)/day)….based on a review findings from studies that evaluated thresholds for serum 25(OH)D concentrations in relation to BMD, lower extremity function, dental health, risk of falls, fx’s, and colorectal cancer.
• On average, serum 25-hydroxyvitamin D levels differed by 5 ng/mL across two assays (using both a radioimmunoassay and an automated chemiluminescent immunoassay)(J Clin Endocrinol Metab 2012;97:835)…..In 13% of patients, measurements from the two assays differed by more than 10 ng/mL……When a patient undergoes serial measurements, the same assay should be used for all measurements.
• A study in which sent serum samples to 8 laboratories that used various 25(OH)D assay methods found significant interlaboratory variability (Clin Chim Acta. 2010;411:1976-1982)…..”If you get a measurement for a patient that is, for instance, 20 ng/mL, recognize that the real value is likely somewhere between 10 and 35 ng/mL,” Dr. Binkley said.
Rule of thumb: 1,000 IU/day increases vitamin D levels by 7 to 10 ng/mL (Prescriber’s Letter 2012;19:9). Wait at least 6 weeks to check 25-hydroxyvitamin D levels after starting treatment or a dose increase.
• For many patients, 1000 to 2000 IU of vitamin D daily is required to maintain a 25(OH)D level at 30 ng/mL or above…..vitamin D inadequacy is common, but I think fixing this is cheap and virtually side-effect free (American Society for Bone and Mineral Research (ASBMR) 2012 Annual Meeting. Presented October 14, 2012).
Vit-D 25-OH D2: an indicator of compliance with supplements. Levels >4ng/mg suggest compliance.
Vit-D 25-OH D3: indicates endogenous production. Therapy should be based on measurement of the total Vit-D 25-OH (D3 + D2) and <20 ng/ml suggest deficiency, 20-30 suggest need for supplementation.
1,25-dihydroxyvitamin D [1,25-(OH)2D] levels: 1,25-Dihydroxy vitamin D is the most potent vitamin D metabolite. It stimulates calcium absorption in the intestine and its production is tightly regulated through concentrations of serum calcium, phosphorus, and parathyroid hormone.
Normal Levels of 1,25-(OH)2D:
Males: > or =16 years: 18-64 pg/mL. <16 years @ 24-86 pg/mL.
Females: > or =16 years: 18-78 pg/mL. <16 years @ 24-86 pg/mL.
High 1,25: primary hyperparathyroidism and in physiologic hyperparathyroidism secondary to low calcium or Vit-D intake. Some pt’s with granulomatous diseases (eg, sarcoidosis) and malignancies containing nonregulated 1-alpha hydroxylase in the lesion may have elevated 1,25-(OH)2D levels and hypercalcemia. 1hydroxylase gene over expression capability seen in breast Ca, lymphomas and leukemias.
Low 1,25: hypoparathyroidism and in chronic renal failure.
Skin Types and levels:
Type 1 skin: extremely fair. Eye color is usually blue or hazel, and hair color is often red or blond. They never tan, but just burn.
Type 2 skin: fair, and eye color is blue. These people may tan a little but usually burn.
Type 3 skin: A darker shade of white. Hair color is brown, as is eye color.
Type 4 skin: light brown. It doesn’t burn easily, but instead tans to a medium brown. American Indians, Hispanics, Mediterraneans, and Asians.
Brown or black hair and brown eyes.
Type 5 skin: tans to a medium or dark brown. Hispanics, Middle Easterners, and some African Americans. T? Type 6 skin isn’t sensitive to sun and rarely burns.
Type 6 skin: Pigmentation is very dark. This group includes African Americans and dark-skinned Asians.
NOTES: Blood levels greater than 120 nmol/L are seen only in Caucasians who work outdoors during the summer months. But Caucasian skin didn’t evolve for full strength sunlight exposure year-round; African-American skin did. Among communities of dark-skinned people who spend much or all of their time outdoors while wearing little clothing, the typical 25-hydroxyvitamin D blood level is 40 to 60 nmol/L.
Sun Exposure Times Needed to Generate Vitamin D
Skin Type / Time to 1,000 IU June 22 / Time to MED (Produce a Sunburn) / Time to 1,000 IU December 22
1: 4 min / 16 min / 37 min.
2: 4 min / 20 min / 46 min.
3: 5 min / 25 min / 55 min.
4: 8 min / 37 min / 1 hr, 24 min.
5: 11 min / 50 min / 1 hr, 55 min.
6: 19 min / 84 min / 3 hr, 39 min.
Deficiency: Definitions & ICD9 | PTH Levels | S/s, Info & Pain | Links: Risks for Defic | Tx & Forms of Vit-D | Vit-D | See Rickets & Child |
A diet deficient in vitamin D causes osteomalacia (called rickets when it occurs in children), which is a softening of the bones. It has been estimated that 50% to 60% of people do not have satisfactory vitamin-D status (levels <20-25 ng/mL), and this is probably related to factors such as urbanization, demographic shifts, decreased outdoor activity, air pollution and global dimming, and decreases in the cutaneous production of vitamin D with age. Vit-D deficiency is defined as serum 25-hydroxyvitamin D (25[OH]D) level <20 ng/mL (50 nmol/L); however, serum assays are notoriously variable. Deficiency leads to osteomalacia in adults, muscle weakness/ hypotonia, rickets in children. Expansion of the epiphyseal growth plates and replacement of normal bone with unmineralized bone matrix are the cardinal features.
Prevalence: 25-50% in nursing home / housebound residents mean age 81yo, 44% elderly ambulatory females age >80yo, 30% women with osteoporosis age 70-79yo, 23% pt’s with hip fx’s mean age 77yo, 42% African American women age 15-49yo, 57% aduls hospitalized pt’s mean age 62yo (Mayo Clin Proc 2010;85:752-58). Data from the third National Health and Nutrition Examination Survey (NHANES III) suggest that a considerable Vit-D deficiency exists in the U.S. and that it has major public health implications (Arch Intern Med 2009;169:626)…..8% of participants had low 25(OH) D (<10 ng/mL)……Females had uniformly lower levels than males and blacks and Latinos had lower vitamin D levels than whites……The percentage of non-Latino blacks with levels lower than 10 ng/mL was 29%, and the percentage of white women older than 40 with low levels was 11%.
• Vitamin D deficiency is common in the elderly and a lack of this vitamin as reflected by 25-hydroxyvitamin D (25(OH)D) levels in older men is associated with reduced BMD (J Clin Endocrinol Metab 2009;94:2773-2780)……the average annual decline in hip bone mineral density was 0.59% in men with levels of 25(OH)D below 15 ng/mL and 0.54% in those with levels of 150 to 19.9 ng/mL……In men with levels of at 20 to 29.9 ng/mL, the annual loss was 0.35%.
ICD-9: 268.9 Unspecified Vit-D deficiency. 268.2 Osteomalacia.
Mild deficiency / insufficiency: serum level 10-30 ng/ml (25-75 nmol/ml).
Deficiency: 25-hydroxyVit-D level <10 ng/ml (<25 nmol/L).
Severe deficiency: 25(OH)D level <5–8 ng/ml (12.5–20 nmol/ml).
Deficiency is often defined as follows: Vit-D-25-OH: <4 ng/mL = profound deficiency; 5 to 8 ng/mL = severe deficiency (usually the level when expect sx’s to arise); 9 to 12 ng/ml = moderately severe deficiency; 13 to 16 ng/mL = moderate deficiency; and 17 to 20 ng/mL = marginal deficiency.
Assessment of Vit-D status: Most experts recommend only screening with the 25(OH)D level (not 1,25). Others suggest that it often is essential to consider both 25(OH)D and 1,25(OH)2D concentrations for accuracy. The circulating concentration of 25(OH)D generally reflects the amount of Vit-D transmitted to the liver from dietary or epidermal sources, and therefore serves as the best index of overall Vit-D status. Because of substantial variation in lab measurement of 25-hydroxyVit-D levels, accurate dx of hypovitaminosis D is problematic, thus until better standardization is achieved, clinicians should be cautious about drawing conclusions from a single 25-OHD measurement (J Clin Endocrinol Metab 2004;89:3149-57).
Low 25(OH)D: seen with nutritional Vit-D deficiency (insufficient Vit-D intake).
Low 1,25(OH)2D: likely from a disturbance in the renal synthesis of 1,25(OH)2D3, particularly levels are low in the face of a normal concentration of 25(OH)D.
PTH levels: Parathyroid hormone levels increase with increasing 25-hydroxyvitamin D levels of more than 20 ng/mL. Elevated PTH levels (secondary hyperparathyroidism) are used as a functional indicator of Vit-D deficiency as circulating levels of 25(OH)D of at least 30 ng/ml appear optimal. PTH is typically >42 pg/ml with Vit-D deviciency, insufficiency and resistance (when have normal VitOH25).
When to Check Levels: Anytime. The lowest vitamin D levels are observed in the first part of the year, although an argument could be made to check for peak 25(OH) vitamin D levels in September and trough levels in March, however, the seasonal contribution to vitamin D deficiency is overshadowed by ongoing vitamin D deficiency throughout the year (JAMDA 2010;11:128-131)….Thus, it may be prudent to test for vitamin D deficiency in patients presenting with fatigue, myalgias, and arthralgias regardless of the season of presentation.
S/s & Info: Serum 25-hydroxyVit-D (25[OH]D) concentrations <40 nmol/L are associated with lower musculoskeletal function in ambulatory pt’s >60yo, regardless of activity level, sex, age, race or ethnicity, and calcium intake (Am J Clin Nutr 2004;80:752-758), for optimal function, concentrations as high as 100 nmol/L appear advantageous.
• PTH response is blunted in about two-thirds of pt’s with hypovitaminosis D, and while this may protect against bone loss through decreased bone turnover, it is associated with disrupted calcium homeostasis (Bone 2004;35:312-219).
• The elderly are at risk for Vit-D deficiency for several reasons, including inadequate exposure to sunlight, consumption of low amounts of Vit-D -containing foods and the use of certain drugs which interfere with the absorption and/or metabolism of Vit-D. A serum 25-OH Vit-D level <20 ng/mL is associated with physical decline in older adults (J Clin Endocrinol Metab 2007;92:2058-65).
• There appears to be an association between low serum Vit-D concentrations and the risk of acute respiratory tract infection (Am J Clin Nutr 2007;86:714-717)….those with low Vit-D levels were more likely to contract respiratory infections than controls.
• Because dark skin acts as a barrier to sunlight, the Vit-D supplementation recommended for postmenopausal African-American women may need to be higher (Am J Clin Nutr 2007;86:1657-1662)…..higher amounts, ranging from 50 µg/d (2000 IU) to 70 µg/d (2800 IU) may be needed. Low serum vitamin-D levels are associated with a higher prevalence of peripheral artery disease (PAD) (Arterioscler Thromb Vasc Biol. 2008;28:online April 16). ….Vitamin-D receptors have a broad tissue distribution that includes vascular smooth muscle, endothelium, and cardiomyocytes……higher rates of coronary heart disease and hypertension in populations farther away from the equator with less exposure to the sun have been observed.
• Low levels of vitamin D were associated with an increased risk for peripheral arterial disease (PAD) in a large, cross-sectional study (Arterioscler Thromb Vasc Biol 2008;DOI: 10.1161/ATVBAHA.108.165886)…..For every 10 ng/mL that vitamin D levels decreased, the risk was increased by 35% (PR 1.35, 95% CI 1.15 to 1.59). Vitamin D deficiency is common in patients with chronic migraine suggests that this patient group, like other vitamin D deficient populations, is at increased risk for cardiovascular disease, malignancy, and other serious illnesses that have been linked to low levels (American Headache Society 50th Annual Scientific Meeting: Abstract S33. Presented June 28, 2008).
• A study with 3258 patients followed for a median of 7.7 years suggests a link between low levels of vitamin D and both cardiovascular mortality (HR, 2.22) and all-cause mortality (HR, 1.61) regardless of the extent of coronary artery disease (Arch Intern Med 2008;168:1340-1349).
• Depression in older adults may be related to poor vitamin D status and elevated parathyroid hormone levels according to a population-based study (Arch Gen Psychiatry 2008;65:508-512)(cannot establish whether the association is causal)……both major and minor depression in older adults was associated with 14% lower serum 25-hydroxyvitamin D levels than seen in those who did not suffer from depression…..Average parathyroid hormone thyroid levels were 5% higher with minor depression and 33% higher with major depressive disorder.
• A vitamin D deficiency has been associated with twice the risk of a myocardial infarction over a decade for men with undiagnosed coronary disease at baseline, a nested case-control study found (Arch Intern Med 2008;168:1174-1180).
• A study on 3258 patients that were followed for a median of 7.7 years found an independent association of low serum 25-hydroxyvitamin D and 1,25-dihydroxyvitamin D levels with all-cause and cardiovascular mortality (Arch Intern Med 2008;168:1340-1349)….Hazard ratios for all-cause mortality for Quartile 1, 2, 3 and 4: 25-hydroxyvitamin D @ 2.08, 1.53, 1.24 and 1 (reference). 1,25-dihydroxyvitamin D @ 1.61, 1.26, 1.16 and 1 (reference)……Adjusted for age, sex, body-mass index, exercise, smoking, diabetes, blood pressure, albumin, cystatin C, triglycerides, N-terminal pro-brain natriuretic peptide, low-density lipoprotein (LDL), high-density lipoprotein (HDL), and use of bronchodilators, aspirin, statins, beta blockers, and ACE inhibitors………..Low 25-hydroxyvitamin-D levels were also significantly correlated with markers of inflammation (CRP and IL-6), oxidative burden (serum phospholipid and glutathione levels), and cell adhesion (vascular cell adhesion molecule-1 and intercellular adhesion molecule-1 levels)……these results show that a low 25-hydroxyvitamin-D level can be considered a strong risk indicator for all-cause mortality in women and in men.
• Vitamin D insufficiency is associated with increased body fat and decreased height but not with changes in peak bone mass, according to the results of a cross-sectional study in 90 postpubertal women aged 16 to 22 years and living in California (J Clin Endocrinol Metab. 2008;Published online November 4)……Insufficiency of 25(OH)D, defined as a serum level of 29 ng/mL or less, was present in approximately 59% of participants, and the remaining 41% had sufficient 25(OH)D levels, defined as a serum level of 30 ng/mL or more. Higher vitamin D levels correlated with better muscle power and force in adolescent girls (J Clin Endocrinol Metab 2009;94:559)…..After adjustment for body weight, vitamin D levels were positively associated with jump velocity (P=0.002), jump height (P=0.006), fitness index (P=0.003), and force (P=0.04)…….Because milk intake (a major source of vitamin D) by adolescents has decreased significantly during the last 20 years, supplementation with vitamin D might be necessary.
• A low level of vitamin D in older patients is associated with a higher risk (2-fold) of cognitive impairment (J Geriatr Psych Neurol 2009:Jan)….the study design which does not allow conclusions about causalityn.
• Evidence suggests for people over 65 years old, taking vitamin can decrease nonvertebral fracture risk by 20%, and hip fracture risk by 18%…..treating 93 seniors with 800 IU of vitamin D daily for 1 to 7 years will prevent one nonvertebral fracture (Arch Intern Med 2009;169:551-61).
• Lower 25-hydroxyvitamin D [25(OH)D] levels in older men are associated with slower psychomotor processing speed, according to the results of a population-based, cross-sectional study (J Neurol Neurosurg Psychiatry. 2009;Published online May 21).
• Vitamin-D deficiency may be associated with a higher disability score and increased rate of disease progression for patients with MS (Consortium of Multiple Sclerosis Centers (CMSC) 23rd Annual Meeting: Abstract P07. Presented May 29, 2009)….21.8% of patients were deemed deficient in vitamin D (serum levels were < 20 ng/mL)……”Vitamin D has multiple effects, including the fact that it can downregulate the immune response, which we think is important in MS; it can interact with the genes that predispose to MS, potentially upregulating or downregulating those genes.”
• Vitamin D levels in children were inversely associated with measures of allergy and asthma severity (Am J Respir Crit Care Med 2009;179:765)….next step is to determine whether vitamin D supplementation is beneficial, and to establish the supplemental dose required for prevention and treatment of asthma.
• Low vitamin D levels (<10 ng/mL) are associated with impaired cognition (Neurology 2009 Sep 30;e-pub ahead of print)…..the low-level group had significantly lower mean cognitive scores and a significantly higher prevalence of scores below the cut-off for cognitive impairment (17%, vs. 9% in the normal-level group)…..Testing 25(OH)D levels in our patients with cognitive problems seems reasonable, but the value of routine testing to determine the need for preventive supplementation in those with normal cognition is unclear.
• Vitamin D supplementation and pharmacist review of medications may help reduce falls in elderly nursing home residents according to a analysis if 41 trials, enrolling a total of 25,422 participants, meeting selection criteria (Cochrane Database Syst Rev. Published online January 20, 2010).
• In adults with asthma, low vitamin D levels are linked with lower lung function, increased propensity for bronchospasm, and reduced response to glucocorticoids (Am J Respir Crit Care Med 2010;online Jan).
• In older men, fracture risk was elevated only among those with serum 25-hydroxyvitamin D levels <16 ng/mL according to data on 1194 older men (mean age, 71) followed for an average of 11 years (J Clin Endocrinol Metab 2010;95:2637).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








