CHAPTER 28 Nucleoplasty
Description
Terminology and Subtypes
Nucleoplasty, also termed minimally invasive nuclear decompression, refers to an intervention in which a probe is inserted through a catheter and into the nucleus of an injured intervertebral disc (IVD) thought to be responsible for symptoms of chronic low back pain (CLBP), and energy is targeted at a portion of the nucleus in order to eliminate it.1 This procedure can be considered minimally invasive when it is compared with traditional surgical discectomy because it does not require direct visualization of the structures and it can be delivered through a very small skin incision. The type of energy used during nucleoplasty is a form of radiofrequency termed coblation, which involves disrupting molecular bonds in the surrounding plasma with only minimal production of heat.1 The terminology surrounding nucleoplasty is not standardized, and various names have emerged emphasizing one or more of its characteristics. Nucleoplasty has also been referred to (sometimes incorrectly) as minimally invasive disc decompression, percutaneous disc decompression, percutaneous disc decompression using coblation therapy, percutaneous nucleotomy, percutaneous radiofrequency thermomodulation, percutaneous plasma discectomy, or coblation nucleoplasty.
History and Frequency of Use
The IVD was first proposed as a potential source of CLBP when the concept of disc herniations was proposed by Mixter and Barr in 1934.2 Since that discovery was made, numerous surgical interventions have been devised to address and correct perceived injuries to the IVD. Traditional operative disc decompression has long been accepted as the standard treatment for large disc herniations resulting in progressive or severe neurologic deficits or unbearable lower extremity symptoms. Although advances are continually made in traditional disc decompression in an attempt to increase its efficacy and safety, it remains a surgical procedure that involves substantial disruption to surrounding tissues in order to expose the targeted IVD. Clinicians and scientists have relentlessly pursued progressively less invasive approaches to disc decompression to increase the accessibility and use of this procedure in selected patients.3,4 Some of the innovative interventions that have been offered as percutaneous alternatives to traditional decompression include automated percutaneous lumbar discectomy (APLD), laser disc decompression, hydrodiscectomy (e.g., SpineJet MicroResector), and intradiscal electrothermal therapy (IDET); the latter is discussed in Chapter 27 of this text.
During percutaneous endoscopic discectomy, surgeons have often noted an inflamed outer annulus adjacent to the disc protrusion.5 Removing the herniated disc within the protrusion was commonly thought to remove the source of inflammation and decrease pressure on the innervated outer annulus and adjacent posterior longitudinal ligament and nerve roots. However, percutaneous techniques using medium and smaller diameter cannulae were not designed to remove nucleus material directly behind the protrusion. Unlike larger 3- to 5-mm outer diameter cannulae used for “surgical” percutaneous disc decompression, those performed though smaller 2.5- to 3-mm cannulae used in APLD, laser disc decompression, or hydrodiscectomy are designed to allow easy access only to the disc nucleus and not to herniated nucleus material located within posterior annular fissures or protrusions. These techniques primarily eliminate injured tissue by cutting, aspirating, or vaporizing the nucleus within the center of the disc, and do not necessarily remove nuclear material within the protrusion unless the protrusion is located along its access path.
Procedure
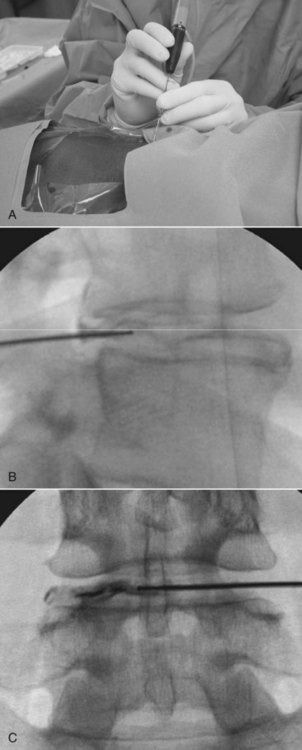
Nucleoplasty uses the Perc-D SpineWand bipolar radiofrequency device manufactured by ArthroCare (Sunnyvale, CA). The procedure begins with the patient wearing a medical gown and lying prone on a treatment table (Figure 28-1A). The area to be treated is typically cleaned with sequential alcohol or betadine wipes. The procedure can be performed under conscious sedation to minimize patient discomfort or anxiety. Nucleoplasty is performed under image guidance using fluoroscopy. A 17 gauge (G) introducer needle is first inserted through the skin, subcutaneous tissue, and muscle, and advanced to the annulus-nucleus junction using standard posterolateral access techniques; catheter position is critical to a successful nucleoplasty procedure.
Once the needle is in place, the nucleoplasty “wand” is introduced through the needle placed into the annular-nuclear junction. The nuclear tissue is then ablated using a high-voltage (typically 100 to 300 V) electrical current produced by bipolar radiofrequency energy and delivered at a frequency of 120 KHz. In hydrated-tissue conductive medium containing normal saline, this current creates a plasma field approximately 75 mm thick that is composed of highly ionized particles with sufficient energy to break organic molecular bonds and thus vaporize tissue. By advancing the wand in ablation mode and retracting the probe while delivering a bipolar radiofrequency coagulation, 1 mm channels are created in the nucleus (see Figures 28-1B and 28-1C).
Theory
Mechanism of Action
The precise mechanism of action through which nucleoplasty can help patients with CLBP is unclear, but is thought to involve decreased pressure in the nucleus, thereby reducing nerve root tension and allowing a protrusion to implode inward, reducing any contact pressure between the protruding disc and spinal nerve root. Although pressure on a nerve root is considered a primary cause of radicular low back pain (LBP), few studies have validated this mechanism. Takahashi and colleagues measured the contact pressure between the nerve and annulus in patients under general anesthesia in a prone position before and after removing a herniated disc.6 Pressure ranged from 7 mm Hg to 256 mm Hg (mean 54.2) before discectomy and decreased to 0 mm following the procedure, and was directly correlated with the amount of trunk list and degree of neurologic deficit before the operation.
Because nerve edema can be induced by pressure of only 50 mm Hg sustained for only 2 minutes, this study suggests that nerve not compression could in fact contribute to radicular CLBP.7 One might logically conclude that removing a herniated disc would relieve pressure on an affected spinal nerve root. However, the effect of lowering nuclear pressure by removing a small amount of nucleus from the center of the disc is conceptually harder to understand, especially if the desired effect is to lower annular tension for the purpose of decreasing axial CLBP. This mechanism was confirmed by histologic examination after channel “coblation” (coagulation ablation) in harvested sheep discs in which there was no evidence of collateral tissue or cell destruction.8 The main explanations that have been offered for the effects of nucleoplasty are the pressure theory, implosion theory, and chemical theory; each is briefly summarized here.
Pressure Theory
The concept of lowering pressure was postulated by surgeons to justify nuclear decompression using laser heat ablation. Case and colleagues measured a rapid rise in the pressure of cadaver discs while slowly infusing normal saline into the disc nucleus.9 These findings were consistent with the concept that the nucleus, surrounded by a relatively inelastic annulus and solid vertebral end plates, acts like a tight hydraulic space where large pressure rises occur with a small increase in volume. On the basis of these findings, it was suggested that small decreases in volume must lead to large decreases in intradiscal pressure.9
In a follow-up study using a 1000-J Nd:YAG 1.32-micron laser delivered through a quartz fiber, the mean intradiscal pressure in cadaver discs was decreased by 43%.10,11 Likewise, using a 350 Nd:YAG laser, Yonezawa and colleagues vaporized central nuclear tissue in rabbit discs, creating a hole in the nucleus that, over an 8-week period, gradually filled with fibrous tissue and lowered the vertically measured disc pressure by approximately 50%.12 Removing even less nuclear material by creating six channels in the nucleus of cadaver discs, Chen and colleagues showed a 100% drop in pressure in normal discs from young cadavers, but only a negligible drop in pressure in degenerated discs.13
In addition to direct pressure measurements in animal models, Hellinger and colleagues indirectly studied disc pressure changes in 21 patients by comparing the disc densities in computed tomography (CT) scans before and after nonendoscopic Nd:YAG laser nuclear ablation.14 Density within disc protrusions showed a statistical difference of 66.3 Houndsfield units, corresponding to a 20% postoperative density reduction. Therapeutic results were attributed to improved flow of venous and cerebrospinal fluid. Although these studies suggest that pressure is lowered within the nucleus immediately after ablation, little is known about the effect on tensional forces in the outer annulus or the duration of decreased pressure. Because injecting the disc with fluid will increase outer annular pressure when radial annular tears extend to the outer annulus, one might reasonably conclude that lowering the fluid pressure would decrease annular tension.15
Several studies suggest that it may be preferable to remove a smaller amount of nuclear material through ablation. Mochida and colleagues performed percutaneous discectomy on 47 young (average age 27 years) patients with herniations causing radicular pain.16 They compared results of 25 cases in which an average of 3.8 g of tissue was removed from the central nucleus to 22 cases in which an average of only 1 g was removed from the posterior protrusion. Although 2-year outcomes were comparable at about 70% in both groups, 10-year results were favorable in 71% for the group that had less tissue removed compared with only 36% in those having more tissue removed. More importantly, disc space collapse greater than 30% was observed in 57% of the group with more tissue removed, compared with 20% of the group with less tissue removed. A decrease in disc herniation size did not correlate with outcome.
Further supporting these findings, another study showed that in elite athletes a more extensive arthroscopic removal of tissue was associated with an acute worsening of symptoms and a delayed return to sports activity.17 Similarly, Carragee and colleagues had better outcomes after open surgical removal of herniated discs when less nuclear material was removed.18 The study compared removal of all the free fragments through an annulotomy incision to a more limited removal of the herniated mass alone. Although recurrent herniation rate was higher in the group with limited disc material removal, clinical outcomes measured by satisfaction, pain, and function were superior to the group with more removed disc material.
Although removing nuclear tissue will decrease disc pressure in the inner and middle annular fibers, little effect is seen on the outer and more commonly innervated collagenous layers.19 In addition, during creep loading the reduced nuclear tension allows the inner layers to bulge inward, reducing height and compressive strength, and potentially leading to lateral segmental instability.20 Reduced nuclear pressure shifts load to the relatively thin outer annulus causing high, irregular stress concentrations that may cause pain.20–24 In addition, the lowered pressure in the nucleus and the elevated pressures in the annulus will suppress chondrocyte metabolism leading to further disc dehydration and reduction of osmotic forces.25,26
Wognum and colleagues showed that decreased osmotic pressure exposes the tips of annular tears to increased stress concentrations, causing cracks to open, potentially increasing the risk of herniation.27 In addition, a drop in nuclear pressure will cause disc space narrowing and disc bulging. In hydrated cadaver discs, Brinckmann and colleagues28 showed a significant drop of pressure when up to 3 g of nuclear material was removed. For every gram of tissue removed from the nucleus, disc height collapsed by an average of 0.8 mm and the disc bulged by 0.02 mm. Similarly, Castro and colleagues showed that removal of 4.6 g of nuclear material by APLD narrowed the disc space by 1.42 mm and increased the disc bulge by 0.45 mm.29
Interpreting findings of decreased IVD pressure is challenging, because the majority of discs selected for this procedure may already have lowered nuclear pressures from end-plate injury or disc herniations. With the nucleus already decompressed, the benefits of further decompression may be questionable, but removing less disc material would perhaps cause less harm in such cases. Interestingly, studies have suggested that elevating nuclear pressures may be theoretically beneficial in those cases where an annular tear alone is present in an otherwise healthy hydrated nucleus.19 Although elevated pressure will increase the risk of disruption, decreased chondrocyte metabolism should eventually relieve the pressure.30 Furthermore, nuclear decompression typically occurs after injuries such as an end-plate fracture, annular tear with herniation, outer rim lesion, or concentric annular tears.31,32 One could postulate that minimal nuclear decompression might initiate, assist, or hasten this response. Further studies, however, are required to understand the effects of nucleoplasty on disc pressure and the potential role for this phenomenon to explain clinical outcomes in CLBP.
Implosion Theory
Another goal of central nuclear decompression is to allow room for the herniated fragment to implode inward and reduce the tension on the nerve root and annulus. There is little evidence to support this theory. In fact, Delamarter and colleagues reviewed the magnetic resonance imaging (MRI) scans of 33 patients with radicular pain as the result of a disc herniation before and after APLD and saw no measurable changes at 6 weeks.33 At the L4-5 level and above, a more lateral approach will facilitate posterior needle placement and targeted tissue removal.34
Indication
The following indications have been proposed for nucleoplasty and primarily radicular CLBP36:
The following indications have been proposed for nucleoplasty and primarily axial CLBP36:
Assessment
Prior to receiving nucleoplasty, patients should first be assessed for LBP using an evidence-based and goal-oriented approach focused on the patient history and neurologic examination, as discussed in Chapter 3. Clinicians should also inquire about medication history to note prior hypersensitivity/allergy or adverse events (AEs) with drugs similar to those being considered, and evaluate contraindications for these types of drugs. Advanced imaging such as MRI or CT is required to help guide the spine specialist to target the appropriate spinal levels involved in a patient’s CLBP.37 Findings on advanced imaging that may be of interest to nucleoplasty include MRI or CT findings of substantial disc herniations concordant with patient symptoms. Interventional diagnostic testing may also be used prior to recommending or performing nucleoplasty, especially in cases of symptoms that persist for more than 6 months and prove recalcitrant to exhaustive conservative treatment measures. The use of provocative discography for CLBP remains controversial, but is used by some clinicians to identify painful disc herniations that may subsequently be targeted with other interventions, including nucleoplasty.