ACUTE BACTERIAL SINUSITIS
Acute bacterial sinusitis is bacterial infection of one or more of the paranasal sinuses lasting <30 days.1 The most common predisposing factor is a viral upper respiratory infection (URI). The incidence of viral URIs in children age 6 months to 35 months is approximately six episodes per patient-year, with approximately 8% of those becoming complicated by acute bacterial sinusitis. Bacterial sinusitis in children is most common in the 12 to 23 months age group, probably because these children are most likely to be in daycare, predisposing them to URIs.2 The cost of acute pediatric bacterial sinusitis in the United States is approximately $20,000 per hospitalized patient, and a large geographic variation in healthcare utilization exists.3 In 1996, total healthcare costs in the United States incurred from treating sinusitis in children <12 years of age had been estimated at $1.8 billion a year.4
The sinuses are air cavities lined with ciliated columnar epithelium that helps mucus clearance by pushing mucus and debris out of the sinus ostia into the nasal cavity. Blockage of the ostia by mucus and inflammation predisposes to bacterial sinusitis. The ethmoid and maxillary sinuses are present at birth and are most commonly involved in sinusitis in children. The sphenoid sinuses form at 3 to 5 years of age. The frontal sinuses do not appear until 7 to 8 years of age and remain incompletely pneumatized until late adolescence. The most common predisposing factors for acute bacterial sinusitis are diffuse mucositis secondary to viral rhinosinusitis in about 80% and allergic inflammation in about 20%.5 Less common predisposing factors include nonallergic rhinitis, cystic fibrosis, dysfunctional or insufficient immunoglobulins, ciliary dyskinesia, and anatomic abnormalities.6
The most common pathogen of acute bacterial sinusitis is Streptococcus pneumoniae, recovered in 30% of children with acute sinusitis. Nontypeable Haemophilus influenzae and Moraxella catarrhalis are each recovered in 20%.6,7
Children with acute bacterial sinusitis typically present with high fever and purulent nasal discharge. Headache, particularly behind the eye, is variable. Complaints of facial pain in children are rare.2 The physical examination findings of acute bacterial sinusitis are often similar to those of uncomplicated viral sinusitis, with swollen and erythematous turbinates and mucopurulent discharge. However, reproducible unilateral tenderness to percussion or direct pressure of the frontal or maxillary sinus may indicate acute bacterial infection, and periorbital edema might indicate ethmoid sinusitis.2 Transillumination of the maxillary sinuses is unreliable in children <10 years of age.8
Although the gold standard for diagnosis of acute bacterial sinusitis is the recovery of ≥104 colony-forming units/mL of bacteria from the paranasal sinuses, sinus aspiration is painful and impractical in the ED.6 Therefore, diagnosis is often based on clinical criteria that help to distinguish acute bacterial sinusitis from an uncomplicated viral URI in an ill-appearing child (Table 120-1).1
| Persistent symptoms lasting >10 d without improvement | Nasal or postnasal discharge and/or Daytime cough |
| Worsening course | Worse or new onset of nasal discharge, daytime cough, or fever after initial improvement |
| Severe onset | Fever ≥39°C (102.2°F) Purulent nasal discharge for ≥3 d |
Imaging studies should not be obtained to differentiate acute bacterial sinusitis from viral URI because of the high incidence of sinus mucosal abnormalities in patients with simple upper respiratory symptoms or no clinical symptoms at all.1 In one study, mucosal sinus changes were evident in 97% of infants who had a URI in the 2 weeks preceding a cranial CT done for unrelated reasons.10 Plain films have limited utility because they require correct positioning that is technically difficult in young children, and there is only a 70% to 75% correlation of culture confirmation with abnormal-appearing sinus radiographs.11 A paranasal sinus CT with contrast or an MRI with contrast is, however, recommended for suspected orbital or CNS complications of bacterial sinusitis, including preseptal or postseptal cellulitis, subperiosteal abscess, cavernous sinus thrombosis, osteomyelitis of the frontal bone (Pott’s puffy tumor), subdural empyema, epidural or brain abscess, and meningitis.1,11
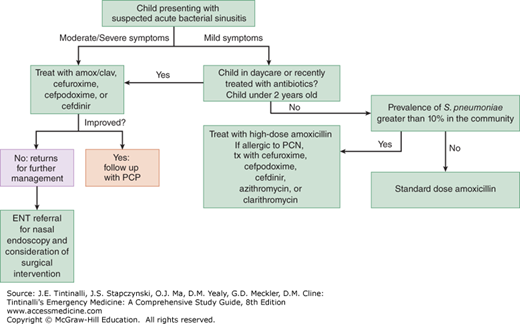
Patients with mild symptoms suggestive of a viral infection can be observed for 7 to 10 days, with no antibiotics prescribed. However, if symptoms persist or are severe (Table 120-1), suspect acute bacterial sinusitis and prescribe antibiotics to speed recovery, prevent suppurative complications, and minimize asthma exacerbations in susceptible children (Figure 120-1).1
Antibiotic treatment for acute sinusitis is outlined in Table 120-2.
| Clinical Scenario | Additional Factors | Treatment | Duration of Treatment |
|---|---|---|---|
| Mild symptoms or age >2 y | Not in daycare, no antibiotics in past 4 wk | Amoxicillin 22.5 milligrams/kg PO twice daily | 10–28 d or 7 d beyond resolution of symptoms |
| >10% Streptococcus pneumoniae prevalence | Amoxicillin 40–45 milligrams/kg PO twice daily | ||
| Moderate-severe symptoms or age <2 y | Attending daycare or recent amoxicillin administration | Amoxicillin 40–45 milligrams/kg with clavulanate 3.2 milligrams/kg PO twice daily | |
| Vomiting, noncompliant | Ceftriaxone 50 milligrams/kg IV/IM once a day | Substitute PO agent when tolerable | |
| Penicillin allergic | Cefdinir 7 milligrams/kg PO twice daily or Cefuroxime 15 milligrams/kg PO twice daily or Cefpodoxime 5 milligrams/kg PO twice daily | 10–28 d or 7 d beyond resolution of symptoms |
Decongestants, antihistamines, and nasal irrigation are not effective for children with acute bacterial sinusitis.12 Adjunctive therapy with intranasal steroids (e.g., fluticasone propionate, one to two sprays per nostril daily, or beclomethasone, one to two sprays per nostril twice a day) has modest benefits and may be considered.1,13,14
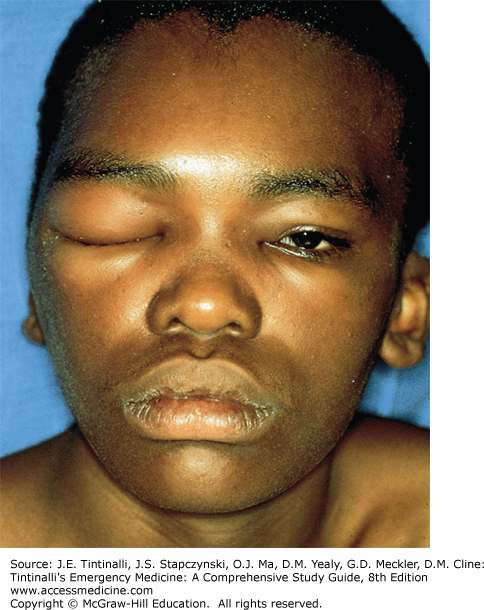
Complications of acute bacterial sinusitis are rare but usually involve the orbit or CNS. If suspected, obtain a contrast-enhanced CT scan or an MRI if possible.15 Proptosis or impairment of extraocular muscle movement suggests orbital inflammation, usually from extension of an ethmoidal infection (Figure 120-2). Frontal and sphenoidal inflammation can lead to intracranial extension, causing frontal lobe and subdural abscesses as well as meningitis and empyema. IV antibiotics are needed, and surgical management may be necessary. Consult an ophthalmologist and/or neurosurgeon promptly for complications.1 For further discussion of the management of periorbital and orbital sinusitis, see chapter 119, “Eye Emergencies in Infants and Children.”
FIGURE 120-2.
Sinusitis. Adolescent with pansinusitis complicated by periorbital cellulitis. The patient was also found to have osteomyelitis of the frontal bone (Pott’s puffy tumor). [Reproduced with permission from Knoop K, Stack L, Storrow A: Atlas of Emergency Medicine, 2nd ed. © 2002, McGraw-Hill, New York.]
CHRONIC BACTERIAL SINUSITIS
Chronic rhinosinusitis is an inflammatory process involving the mucosa of the nose and sinuses that lasts >3 months.16 Factors associated with chronic sinusitis include older age, allergic rhinitis, recurrent viral URIs, immunodeficiency, ciliary dyskinesia, anatomic abnormalities, and fungal colonization of the sinuses.17 The most common organisms identified are α-hemolytic Streptococcus, H. influenzae, and S. pneumoniae.18 Chronic sinusitis has been linked to asthma, and treatment of chronic sinusitis reduces asthma symptoms.19
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree