Noninvasive Studies for Detection of Coronary Disease
The importance of diagnosing coronary heart disease (CHD) is underscored by its prevalence and serious consequences, as well as the availability of therapies that can improve quality of life and prolong survival (see Chapters 18, 30, and 31). A host of noninvasive stress-testing modalities have been the mainstay of identifying persons who need referral for consideration of invasive angiographic study, but they remain imperfect. Only about a third of patients who undergo elective coronary angiography for suspected atherosclerotic heart disease prove to have significant stenoses. The advent of noninvasive angiographic imaging technologies holds promise for better risk stratification.
The design of an effective workup for suspected CHD and proper test interpretation benefit from a clinical estimate of the pretest probability for CHD (see Chapters 18 and 20) and knowledge of the performance characteristics, costs, advantages, and disadvantages of available testing modalities. This chapter focuses on the noninvasive testing modalities for CHD; their application is addressed in separate chapters focused on screening, diagnosis, and management of CHD (see Chapters 18, 20, 30, 31).
THE RESTING ELECTROCARDIOGRAM (ECG, 1-3)
The resting ECG, while essential to the evaluation of persons with chest pain, does not add significant predictive value as a screening test for CHD over that provided by the Framingham Risk Score (FRS) (see Chapters 18 and 20) to warrant its use in unselected, asymptomatic adult populations. Its inadequate contribution to risk stratification has led the U.S. Preventive Services Task Force, the American College of Cardiology, and the American Heart Association to recommend against its routine use in asymptomatic adults at low CHD risk. For persons at higher risk, the data are insufficient for the U.S. Preventive Services Task Force to render an opinion. The high prevalence of ECG abnormalities and CHD among the elderly has attracted the interest of investigators to explore its performance as a screening modality for CHD in asymptomatic elderly adults (e.g., ages 70 to 79 years). Presence of minor changes (minor ST- and T-wave changes) and major ECG abnormalities (pathologic Q waves, QS pattern, high voltage, delta waves, complete bundle branch block, atrial fibrillation/flutter, major ST-and T-wave changes) were found to add to the risk assessment after correcting for standard risk factors (hazard ratios 1.35 and 1.51, respectively). However, when combined with the FRS, the Net Reclassification Index was insignificant at 5.7%. Most of the contribution to restratification was for persons free of ECG abnormalities, who were reclassified into the lower-risk group, limiting the impact on overall care.
STRESS TESTING (2,4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40 and 41)
Physiologic Basis of the Test
Stress testing assesses the ability of the coronary circulation to meet the enhanced myocardial oxygen requirements of exercise- or drug-induced stress. Because the rate of oxygen extraction by the heart is relatively fixed, increased oxygen demand must be met by an increase in coronary blood flow. When coronary artery stenosis critically limits the blood supply, oxygen demand may so exceed supply that myocardial ischemia ensues, manifested by transient changes in ECG ST segments, ventricular wall motion, and radionuclide distribution. In addition, the patient may experience abnormal blood pressure and heart rate responses, angina, or an anginal equivalent such as severe dyspnea.
The demand placed on the coronary circulation can be quantified: The product of heart rate times systolic blood pressure closely parallels the measured myocardial oxygen consumption during isotonic exercise and is designated in metabolic equivalents (METs), where 1 MET = 3.5 mL of O2 consumed/kg/min. Heart rate alone provides a good approximation of oxygen consumption. Because known quantities of work are being performed, the exercise stress test can also provide a measure of exercise capacity and aid in the detection, quantification, and localization of coronary disease.
Approaches to Stress Testing
The stress test may use exercise or pharmacologic measures to challenge the capacity of the coronary circulation. Exercise remains the simplest means, usually achieved by treadmill or stationary bicycle activity. Pharmacologic approaches stress the coronary circulation by inducing either reflex tachycardia or intracardiac vasodilation.
Exercise-Based Testing
Exercise testing for the detection of coronary disease uses dynamic (isotonic) rather than sustained-contraction (isometric) exercise. Isotonic exercise permits smooth increases in the rate-pressure product to be accomplished, allowing the patient’s ischemic threshold to be approached gradually. Nevertheless, isometric exercise testing (e.g., by sustained handgrip) can be of use in special situations (e.g., assessing the safety of isometric activities in patients with known coronary disease).
Many different exercise protocols are available for the treadmill and the bicycle. Although the staged Bruce protocol is very popular and widely used, it has the disadvantages of unequal changes in work load between stages and a very abrupt increase in work load at stage IV, which is too vigorous for many cardiac patients. Walking protocols are generally preferred over protocols that require running for diagnostic purposes in unfit populations. Bicycle ergometer protocols usually consist of 2- to 3-minute stages in which workload is increased by 10 to 30 W per stage, depending on the level of physical conditioning of the subject. For both treadmill and bicycle tests, it is best to select a protocol that will allow the patient to reach maximal exertion within a 10- to 12-minute period. A longer test may be limited by the subject’s endurance, and a shorter test usually increases the workload too rapidly.
The testing protocols for isotonic exercise testing are divided into maximal and submaximal types, depending on the level of exercise achieved during the test. Testing methods include ECG monitoring, echocardiographic imaging, and radionuclide imaging.
The Maximal Test.
Maximal testing is defined as testing in which systemic oxygen consumption reaches a plateau before exercise is terminated. Maximal effort is usually approximated by exercising the individual to an age-adjusted predicted maximal heart rate. Values for maximal predicted heart rate can be obtained from standardized tables or regression formulas, but the values 220 minus age in years for men and 210 minus age in years for women provide reasonable approximations of the true maximal heart rate. Tests terminated before the maximum predicted heart rate has been achieved are less sensitive for diagnosis of CHD. In general, it is best to continue the test to the predicted maximum heart rate or to the maximum perceived effort or until angina, ischemia, arrhythmia, or hypotension occurs. If a patient is receiving a β-adrenergic blocking agent, the endpoint of heart rate is supplanted by having the patient exercise to exhaustion. If the perceived effort is “very hard” (19 or 20 on the Borg scale) at the termination of the test, it can be reasonably assumed that maximal exertion has been closely approximated.
The Submaximal Test.
By definition, a submaximal test is one in which maximal systemic oxygen consumption is not achieved. The test may be terminated prematurely by design (at a certain percentage of predicted maximal heart rate or at a given level of systemic oxygen consumption), or it may be terminated because of the appearance of angina, marked ischemic ECG changes, cardiac arrhythmias, severe hypertension, or hypotension. Submaximal testing has been shown to be useful and safe for the early determination of prognosis soon after myocardial infarction. When conducted within 2 weeks of infarction, a submaximal exercise test to a 5-MET level identifies patients at increased risk for subsequent coronary events and death. Many cardiologists prefer to perform a symptom-limited exercise test 1 month after myocardial infarction in lieu of an earlier submaximal test.
Staged (Graded) Testing.
Most exercise tests are staged, meaning that graded amounts of work are performed in a progressively increasing manner. The rationale for graded exercise is to obtain the greatest increase in heart rate before musculoskeletal fatigue limits the amount of exercise that the patient can perform. The onset of muscle fatigue before the achievement of maximum heart rate reduces test sensitivity. The treadmill and bicycle ergometer are the most popular devices for exercise testing. Slightly higher values for maximal oxygen consumption can usually be obtained on the treadmill than on the bicycle ergometer because a somewhat larger muscle mass is called on during treadmill exercise.
Electrocardiographic Monitoring.
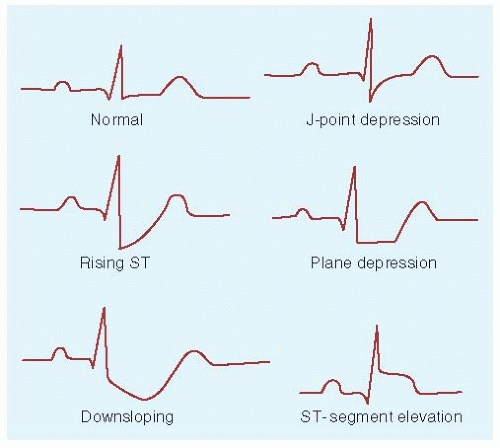
Continuous ECG monitoring is used during exercise testing, as is periodic determination of blood pressure and symptoms. Multilead systems have replaced the traditional single modified V5 ECG lead (CM5). Sensitivity is greatly enhanced by the use of multiple leads, especially for the detection of inferior ischemia. Twelve-lead monitoring is commonly performed multiple times during the test, and three to six leads are monitored continuously; adding another three leads over the right precordium appears to enhance the detection of ischemia due to right coronary or left circumflex disease (see later discussion). The ST segments are assessed for change with exercise. The depth, configuration, and extent of any ST-segment depressions correlate with the presence and severity of coronary disease (see later discussion and Fig. 36-1), as do blood pressure responses and time to development of symptoms. Because ischemic changes may not occur on the ECG until after exercise, monitoring is continued for at least 5 to 7 minutes into the recovery phase.
Radionuclide Imaging.
Radioisotopes can be administered as part of exercise testing to help image myocardial perfusion. Technetium sestamibi and thallium-201 are the two radionuclides in most widespread use. Their regional distribution in the myocardium is proportional to regional coronary blood flow; underperfused areas will take up less of the isotope and will appear as “cold” spots on the perfusion scan. Areas of viable but ischemic myocardium will appear underperfused during exercise but will “fill in” at rest. Therefore, sequential scanning during exercise and at rest is required to diagnose hemodynamically significant coronary stenoses and distinguish them from areas of previous infarction.
Sestamibi testing requires a 2-day protocol, with a 1-hour resting scan on day 1 and a 2-hour exercise and imaging session on day 2. Thallium study is done all in 1 day but requires 2 hours for exercise imaging and a 3-hour wait before a 1-hour imaging session at rest. Sestamibi administration allows for the determination of ejection fraction. Thallium provides images of pulmonary uptake, which parallel pulmonary capillary wedge pressure and correlate with prognosis. Single-photon emission computed tomography (SPECT) is replacing planar scanning technology for image production because it provides better sensitivity.
Radionuclide imaging of myocardial perfusion provides a substantial radiation dose (estimated to be the equivalent of between 200 and 2,000 chest x-rays). Because the test is often repeated, it can account for a substantial percentage of a patient’s cumulative radiation exposure. By one estimate, it is the single greatest contributor among medical diagnostic imaging sources to total radiation burden, accounting for about 22% of the total.
Echocardiographic Imaging.
Stress echocardiographic study provides information on global ventricular function in response to exercise (by measuring the change in ejection fraction and end-systolic volume) and on segmental myocardial perfusion (by comparing regional ventricular wall motion at rest and during or just after maximal exercise). Ischemic manifestations include failure to increase ejection fraction with exercise and new regional wall-motion abnormalities. Compared with radionuclide testing, less time is required, there is no radiation exposure, and cost is lower; in addition, results are immediately available. Test sensitivity for ischemia is reduced by the presence of resting wall-motion abnormalities.
Pharmacologic Stress Testing
Patients who cannot exercise are potential candidates for pharmacologic approaches to testing the adequacy of the coronary circulation, whether by inducing reflex tachycardia or coronary vasodilation. Because the sensitivity of ST-segment changes associated with pharmacologic stress testing is low, cardiac
imaging (either radionuclide or echocardiographic) is required. Although probably not as sensitive as exercise tress testing that achieves maximum predicted heart rate, pharmacologic stress testing does provide results that correlate with and help to predict long-term cardiac outcomes.
imaging (either radionuclide or echocardiographic) is required. Although probably not as sensitive as exercise tress testing that achieves maximum predicted heart rate, pharmacologic stress testing does provide results that correlate with and help to predict long-term cardiac outcomes.
Adenosine or Dipyridamole with Radionuclide Scanning.
These agents rapidly induce coronary vasodilation when given by intravenous infusion, usually over 4 to 6 minutes. Normal coronary arteries respond by dilating and markedly increasing regional myocardial blood flow. Diseased vessels are unable to respond in such fashion. The net result is a steal phenomenon, in which blood flow is diverted away from the areas of myocardium supplied by the stenosed vessels, exacerbating the differences in regional perfusion. Radionuclide (thallium or technetium sestamibi) is administered in conjunction with the vasodilator infusion to provide images of regional myocardial perfusion and detect any significant differences suggestive of clinically important coronary disease. Adenosine is the shorter acting of the two vasodilators (half-life 10 seconds vs. 20 minutes) and is preferred by many because adverse effects (e.g., flushing, nausea, headache, chest tightness, hypotension) are shorter lived, although more common, than with dipyridamole. Methylxanthines (e.g., theophylline, caffeine) block the actions of these agents and should be withheld for up to 3 days before testing.
Dobutamine with Echocardiography.
Dobutamine is a relatively selective β-agonist that is used to stress coronary circulatory capacity by inducing an increase in myocardial oxygen demand through simulative effects on heart rate and myocardial contractility. Underperfused areas show up on ultrasound as thickened hypokinetic myocardium. Sometimes, the muscarinic blocking agent atropine is infused in addition to dobutamine if at least 85% of the maximum predicted heart rate is not achieved by dobutamine alone. Side effects of dobutamine include chest pain, palpitations, dysrhythmias, and blood pressure changes. They usually resolve quickly with cessation of the infusion. Test safety is similar to that for exercise.
Dipyridamole with Positron Emission Tomography.
Positron emission tomography (PET) involves the administration of the vasodilator dipyridamole along with rubidium-82. The isotope’s myocardial uptake is measured by PET, providing a very sensitive and specific, albeit expensive, means of imaging ischemia.
Stress Testing for Diagnosis of Coronary Heart Disease: Test Sensitivity, Specificity, and Predictive Value
Gold Standard, Workup Bias, and Test Limitations
The gold standard for the diagnosis of CHD remains the coronary angiogram. A significant stenosis is defined as an angiographic narrowing of the vessel lumen by 50% or greater. Stress-test performance characteristics (sensitivity and specificity) are determined by comparing test results against angiographic findings. However, the figures cited in the literature for sensitivity and specificity may be subject to workup bias from the preferential enrollment of study patients likely to have coronary disease and therefore willing to undergo angiography. The consequence of such bias is an exaggeration of test sensitivity and an underestimation of test specificity. Workup bias always needs to be considered when interpreting published studies of sensitivity and specificity (see Chapter 2).
Another limitation of stress testing is that it does not identify lesions that may become the cause of sudden death; it only detects impaired blood flow. Most patients who die suddenly from coronary disease do not succumb from a chronic flow-limiting atherosclerotic plaque. Rather, they may die from the acute rupturing and thrombosis of a nonoccluding plaque. Exercise testing does not help to identify such non-flow-limiting lesions, although it can provide an estimate of prognosis by determining the extent and severity of disease, which correlate with overall risk (see later discussion). Direct identification of dangerous plaques is an area of active investigation.
Importance of Pretest Probability in Patient Selection and Predictive Value Determination
With an emphasis in the stress-test literature on test performance characteristics (i.e., sensitivity and specificity), it is easy to confuse them with predictive value (the probability of CHD, given a “positive” stress test). The latter is the relevant probability for the clinician caring for the patient with suspected coronary disease and necessitates considering not only test sensitivity and specificity but also the patient’s pretest probability for CHD. Figures for the predictive accuracy of the exercise stress test have varied greatly from series to series and between men and women, often because of wide differences in the prevalence of underlying coronary disease in the populations studied. The predictive accuracy of any diagnostic test is directly related to the prevalence of the disease in the population examined (see Chapter 2).
A stress test will have a low predictive accuracy when disease prevalence is low, regardless of how sensitive and specific the test is. Proper test interpretation necessitates knowing not only the sensitivity and specificity of the test but also the patient’s pretest likelihood of CHD. A positive test in a person with a low pretest probability is far more likely to be a false positive than a true positive. Careful estimation of the patient’s pretest probability of CHD (see Chapter 20) is essential to proper stress-test interpretation. The prevalence of coronary disease has been found to be 16% in patients with nonanginal chest pain, 50% in those with atypical pain, and 89% when typical angina is present.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree