Fig. 27.1
Abdominal CT at admission to Ziv Hospital
One day after her admission, an explorative laparotomy was done. A surgical pad in the LUQ with puss around, a pigtail drain inside the small bowel, and a huge pelvic mass, partially necrotic, vascularized, reaching the umbilicus were found. The pad was removed, the puss was washed and drained, the pigtail drain was removed, and the mass was biopsied. Final pathology confirmed the tumor to be dysgerminoma. After 1 week of broad-spectrum antibiotics, she was reoperated; excision of the pelvic mass and lymph nodes sampling with preservation of uterus and right ovary was performed. In pathological evaluation, a 1600 g weight, size 9 × 16 × 18 cm mass, and three para-aortic lymph nodes 1.3 cm were found. This mass was dysgerminoma: with PLAT strongly positive, C-KIT positive, and high KI-67, two of three lymph nodes with metastases. Following surgery she started treatment with four courses of BEP chemotherapy combination which includes bleomycin, etoposide, and cisplatin. She was hospitalized for all the treatment period, 4.5 months. Abdominal CT after third course of BEP was normal (Fig. 27.2). The patient was sent back home to Syria in very good performance status.
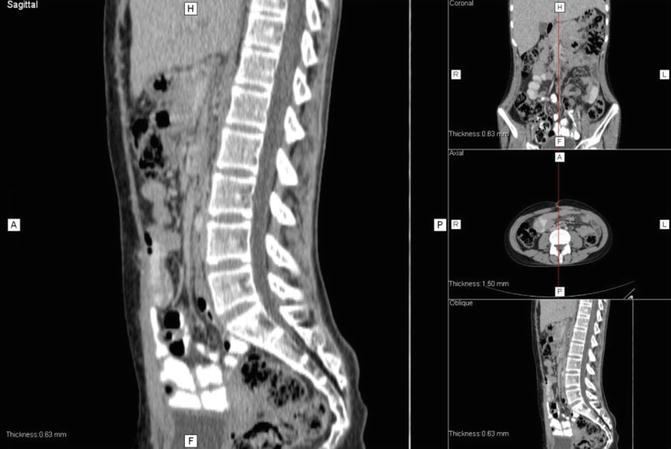
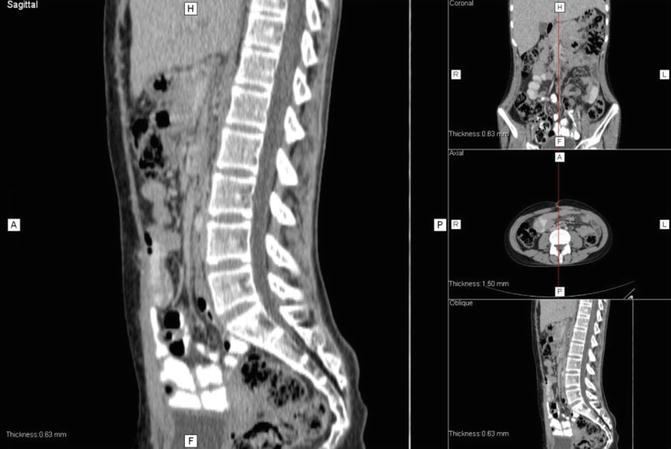
Fig. 27.2
Abdominal CT after third course of chemotherapy
27.2 Discussion
Dysgerminoma is the most common germ cell tumor in the ovary. Dysgerminomas are mostly diagnosed at stage I, but they may spread to retroperitoneal lymph nodes [1]. It is acceptable to operate this tumor by laparotomy and not by laparoscopy. In most cases fertility may successfully be preserved by not excising one ovary and uterus. In our case is a young adolescent that was operated in Syria and few days later was admitted to our hospital with sepsis, huge mass in the lower abdomen, acute abdomen, and surgery complication without any diagnosis or any documents about what was done at her country. Treating in these circumstances is more challengeable, and thus the surgery is more difficult although no serious complications were observed after surgery in our hospital. Patients with stage II–IV are treated by surgery and chemotherapy. This tumor is very sensitive to chemotherapy [2]. BEP combination is the acceptable combination since it was used by MD Anderson Cancer Group at 1984 [3]. Six-year event-free and overall survival rates are 86–93%, respectively [4]. In this case the patient was stage III, and it is acceptable after several complicated surgical interventions to start treatment with BEP. Doing so the girl had to stay at our hospital for long period and need not just medical treatment but social and logistical support as well. Israeli patients are hospitalized for the surgery treatment and after that are discharged home, and they come back to the chemotherapy treatment in daily hospitalization setting. For this girl we have to arrange treatment in different setting and to offer all the treatment regime according to the best medical standards although it is more challengeable than for our citizens. At the end, she was in complete response, and the multi-professional staff accompanied the girl in her struggle against the disease in a foreign country. The girl got back home with a probability of 5-year survival and preserving fertility >90%.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







