Nonaccidental Trauma
Michelle Shouldice MD, FRCPC
EPIDEMIOLOGY
A survey of over 10,000 Canadian adults indicated that 10% of adults experienced severe physical abuse during childhood.1
Eleven percent of women and four percent of men reported a history of severe sexual abuse during childhood.1
Rate of suspected cases reported to Children’s Aid Societies (CAS) (child protection agencies) in Canada is just over 2%.2
Likely due to lack of recognition or under-reporting.
In a retrospective review of children presenting to a pediatric emergency department who were referred to child protection agencies:3
The mean age was 6.4 years old.
The majority (55%) were referred for suspected physical abuse.
There were on average 4 to 5 previous emergency department visits.
The majority of reported cases did not have any physical findings (especially sexual abuse and neglect cases).
Of those with injuries, bruises were the most frequent injury reported.
HISTORY-TAKING
Document source of history (parent, chart, CAS worker, etc.)
Document thoroughly, in historian’s own words, during the time history is taken.
Give careful thought and consider consultation before directly questioning a young child if abuse is suspected.
Avoid extensive questioning, especially of young children.
When appropriate to question the child, ask only open-ended, non-leading, developmentally appropriate questions. For example, “Can you tell me how you hurt your leg?” not “Did your daddy hurt you?”
Child’s motor and language development.
Injuries/possible physical abuse:
Thorough history of injury event, including location, time, who was present, detail of the injury event, symptoms in child, response of caregiver.
Previous injuries.
Family history as appropriate to the injury: Easy bruising, bleeding disorders, recurrent fractures, bone disorders.
Possible sexual abuse/assault:
Determine whether child has active bleeding from the genital area and requires urgent assessment, and when the reported sexual contact occurred.
If no urgent need to assess/treat injuries, consult local child abuse expert PRIOR to beginning assessment.
If available, assessment by trained expert with medicolegal and child abuse experience is preferred.
For younger children, history from caregiver, preferably without the child present.
Reason for concern.
History of vaginal bleeding or discharge.
Other possible sources for bleeding: History of accidental injury, urinary symptoms, constipation, early signs of puberty, redness/irritation.
For older children and adolescents, history taken directly as discussed above:
History of events—time and date of assault, type of contact (skin, oral, genital, anal), pain, bleeding or discharge at the time of the assault or since, was a condom used, memory loss or confusion, possible consumption of mind-altering substances, other injuries.
Assailant’s age, risk factors for sexually transmitted infections (STI) (multiple partners, previous sexual assault/incarceration, IV drug use, known previous or current STI).
History of previous sexual activity, last menstrual period, previous sexually transmitted infection, pregnancy.
Where adolescent lives, supports available. Are parents aware and discuss whether and how adolescents wish to inform parents.
Symptoms of fear, self-harm, suicidality.
Likelihood of forensic evidence available—has child bathed, showered, changed clothes, eaten, voided, defecated.
Discuss consent to inform police, complete a forensic evidence kit if appropriate (see below).
Red Flags in History for Nonaccidental Trauma
History is inconsistent with mechanism or amount of force required to cause injury.
History is inconsistent with the child’s developmental level.
History is inconsistent or changes.
Delay in seeking medical attention without reasonable explanation.
PHYSICAL EXAMINATION
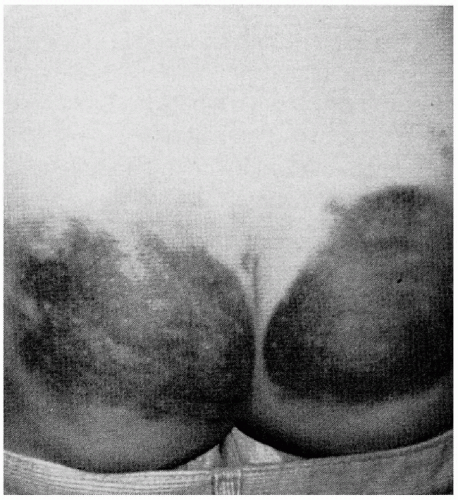
Careful, thorough examination. Ensure all skin areas are seen, including ears, genitalia, buttocks, back.
Clearly document any skin markings, preferably on a body diagram, and labeled with location, color, measured size, pattern.
Take photographs of all concerning skin injuries and store them in patient’s record.
If photography is unavailable, CAS or police can organize photographs.
Document growth parameters including head circumference.
Assess fontanel and perform fundoscopic exam.
Mouth: Look at upper lip frenulum, palate, and tongue frenulum.
Abdominal exam: Tenderness, bruising.
Palpate all body areas for pain, swelling, deformity, or callus.
Examination for Sexual Abuse Concerns:
External genital examination only in prepubertal children, no internal vaginal examination or digital rectal examination (unless specific indication).
Tanner stage of breast and pubic hair development.
External genitalia—redness, bruising—document location, size, pattern, discharge, abrasions/lacerations.
Labia should gently be retracted in a posterolateral direction to allow visualization of the hymen.
Carefully document redness, bruising, or injury (partial or complete transection) of the hymen.
Any abnormal hymenal findings should be reviewed with a clinician who has expertise and training in interpreting hymenal findings.
The source of any bleeding must be sought.
A gynecology consultation is required for ongoing internal bleeding to assess need for surgical intervention.
External anal examination—document redness, bleeding, fissures, other acute injuries (lacerations).
A general surgery consultation is required for deep anal injuries or ongoing anal bleeding.
Red Flags in Physical Examination for Nonaccidental Trauma
Any bruising in a developmentally immobile (prior to cruising) child.
“Those who don’t cruise rarely bruise.”4
Bruises of the cheeks, ears, or buttocks (Fig. 19-1).
Patterned skin injuries (bruises or burns) (Fig. 19-2), including parallel linear bruises (Fig. 19-3), looped skin marks (Fig. 19-4), immersion-pattern scald burns (Fig. 19-5).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree