New Drugs of Abuse
K. Sophia Dyer
Alcohol still holds the lead as the most common drug of abuse and “social lubricant.” However, many other drugs are used and abused by people from all strata of American society, and, unfortunately, these drugs remain in ready supply from local sources and through the Internet. Many of the substances of abuse discussed in this chapter are called “club drugs,” Club drugs a name based on the use of these substances as part of the culture of nightclubs, raves, and dance parties. But their use is not limited to the world of nightclubs. Many adults, teenagers, and children seek and use these drugs. Some are chronically addicted and others are occasional experimenters.
The Spectrum of New Drugs of Abuse
Patterns of drug abuse differ by region. For example, methamphetamine might be seen commonly in one section of the country but unheard of in another. Some of these patterns are static; others reflect the gradual progression of the popularity of a substance. The types of drugs being abused in a community will likely be known to law enforcement agents. New drug patterns could first become apparent to emergency department physicians in a number of ways: a change in the number of intoxicated patients, an increase in the severity of their condition, or variation from the typical presentation of effect or overdose.
Laboratory examination of either the substance or biologic samples from patients can be helpful to public health officials and law enforcement officers. The detection of a contaminant or the introduction of a novel new drug can be vital information for both groups as they respond to community concerns about substance abuse. If the substance is the focus of a criminal investigation, the chain of custody must be preserved.
Variations imposed on chemical structures, which are not always intentional, can cause differences in clinical effect. For example, in an attempt to subvert existing regulations (the Controlled Substance Act), the amphetamine structure was modified and produced as 3,4-methylenedioxymethamphetamine (MDMA, Ecstasy). The Controlled Substance Act defined a substance as “controlled” only after the acceptance of its structure and effect—a retrospective approach that was changed by the Controlled Substance Analogue Enforcement Act of 1986. The 1986 act classifies chemical structures that are substantially similar to those of schedule I or II controlled substances. After this closing of the “loophole,” a substance was considered illegal if it was used as a stimulant, depressant, or hallucinogen and designed for that purpose. These acts continue to be updated, as legal forces attempt to keep pace with those who distribute substances. In March 2000, γ-hydroxybutyrate (GHB) was added to the schedule I list (i.e., drugs with high abuse potential, such as heroin). GHB does not bear any structural similarity to the other schedule I or II drugs, but because of rising concerns about abuse, it was added to the list.
During the past 25 years, “designer drugs” have been implicated in mass poisoning and isolated instances of contamination. Both situations require public health and legal investigations. The early identification of extreme reactions to ingested drugs, atypical emergency department presentations of people who abuse the substances, and an increase in the number of people seeking emergency care after using the drug should be communicated to public health officials in an effort to avoid an epidemic of severe reactions and overdoses.
In 1991, New York City saw a rise in opioid overdoses in a heroin-abusing population. Investigation revealed a drug packaged as “Tango and Cash,” which was found to contain a very potent form of fentanyl (1). A similar case involving heroin with a nonopioid contaminant occurred in several northeastern cities in the United States between 1995 and 1996. The heroin was contaminated with scopolamine, which caused a combined presentation of opiate and anticholinergic poisoning (2). In 1982, clandestine manufacturers intending to produce the meperidine analog MPPP (1-methyl-4-phenyl-4-propionoxypiperidine) actually made MPTP (1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine), which destroyed users’ substantia nigra, causing severe parkinsonism (3). Several comatose teenagers brought to an emergency department in Philadelphia had used the Internet to purchase the GHB they ingested at a party (4).
In addition to laboratory data, the history surrounding the presentation can be helpful to the emergency physician in the assessment and management of a patient suspected of being exposed to a drug of abuse. Suspicion or report of sexual assault should prompt an evaluation for sedative-hypnotics, hallucinogens, GHB or its analogs, benzodiazepines, or dissociative hallucinogens such as ketamine. The patient/victim might be able to identify the type of substance used (liquid, pill, injectable, inhalant) and the intended goal—hallucination, sedation, or stimulation. The report of pill or capsule ingestion suggests that a standard pharmaceutical might have been used. This possibility should be considered in the identification process for any “new” drug of abuse or “designer drug” presentation. The illegal procurement of pharmaceuticals has been reported and documented in relation to mass exposures. For example, in preparation for a dance party, teenagers stole baclofen from the doorstep of a neighbor who receives prescriptions by mail order. The results of distribution of the drug during the party were impressive: 14 children were evaluated at area hospitals, 9 of them requiring intubation (5). The intentional abuse of over-the-counter drugs remains an issue of concern. A poison control center evaluation of 2,214 intentional abuses among children aged between 6 and 14 showed that 38% involved nonprescription drug abuse, the most common being anticholinergics, caffeine, dextromethorphan (DXM), and ephedrine (6).
Testing for Drugs of Abuse
Emergency department physicians who request drug testing for a patient in their care should be aware of the strengths and limitations of the test methods available to them. Consultation with a clinical toxicologist, a clinical chemist, or a clinical pathologist can help identify the likely drug(s) in question. Important variables that should be considered in regard to the assessment of a patient for drug use are sample collection, the type of test to be performed, and the types of substances that could interfere with the accuracy of the results. The most common samples for drug testing are urine and blood; hair and meconium can also be used.
Before concluding that “the tox screen is negative,” the physician must know the methodology used by the laboratory. Does it perform comprehensive screens for multiple substances or single tests for specific xenobiotics? In addition, the physician should be aware of the test’s detection and confirmation limits, especially for new drug analogs. Some drugs (e.g., ketamine) are difficult to detect with standard screening methods; referral to a reference laboratory might be required. Other drugs of abuse, especially amphetamines, are often modified in clandestine “laboratories,” so it is difficult for medical facilities to remain current with analytic techniques and precautions against cross-reactivity.
For some substances, testing can indicate use of the drug but not necessarily intoxication with it. In an analysis for the presence of cocaine, for example, the screen detects benzoylecgonine, a metabolite formed soon after ingestion; therefore, a negative test excludes intoxication, within the appropriate detection levels in testing, but a positive test within the detection interval does not allow a conclusion to be made about if and when the patient was intoxicated. Detection intervals vary with manufacturers, and they can be influenced by the nature of the abuse (chronic vs. occasional). For interpretation of drug test results, physicians are encouraged to consult a medical toxicologist, who is specifically trained to interpret the patient’s presentation in relation to the results of the analysis.
Testing for drugs of abuse has applications in fields other than medicine; rapid testing is used by employers to screen potential and current employees for the presence of drugs. For jobs requiring a commercial driver’s license, most companies test for the NIDA 5, the five substances for which the National Institute on Drug Abuse (NIDA) (http://www.nida.nih.gov.easyaccess1.lib.cuhk.edu.hk) requires
testing for federal employment: cannabinoids, cocaine (benzoylecgonine), amphetamines, opiates, and phencyclidine (PCP). Commercial testing is also available for barbiturates, benzodiazepine, methadone, propoxyphene (Darvon and Darvocet), MDMA, and inhalants such as toluene and xylene. The “NIDA 9” are amphetamine, opiates cocaine, PCP, marijuana barbiturates, benzodiazepine, propoxyphene, and methadone.
testing for federal employment: cannabinoids, cocaine (benzoylecgonine), amphetamines, opiates, and phencyclidine (PCP). Commercial testing is also available for barbiturates, benzodiazepine, methadone, propoxyphene (Darvon and Darvocet), MDMA, and inhalants such as toluene and xylene. The “NIDA 9” are amphetamine, opiates cocaine, PCP, marijuana barbiturates, benzodiazepine, propoxyphene, and methadone.
Testing for drugs of abuse as workplace screening is regulated by legislative influences and must consider workers’ rights. It is common for laboratories to use one method of testing for initial screening and then confirm positive results with a different method. Laboratory testing is subject to governmental regulations. At the federal level, the Clinical Laboratory Improvement Amendments (CLIA) influence the testing of human specimens for medical purposes. Some point-of-care testing is exempt under CLIA, but most other testing is considered moderate to complex. Multiple requirements are listed under each degree of testing, ranging from written procedures to daily controls to on-site supervision. Further information on CLIA and its regulations can be found at http://www.cms.hhs.gov/clia.
Spectrochemical Tests
Many alcohol assays are based on spectrochemical analysis. This test method is based on chemical reactions that produce a light-absorbing product, typically using a specific wavelength of light. The quantity of a substance is determined by the amount of light (infrared or ultraviolet) absorbed. An example of spectrochemical testing is cooximetry used to determine the spectra of hemoglobins. Enzymes can be added to spectrochemical processes as catalysts for specific reactions.
Immunoassays
Immunoassays are one of the more common methods used to detect small concentrations of substances, typically in urine (other specimens can be used as well). The general principle of immunoassays is the use of selective and specific antibodies to recognize the composition of a drug. A limitation of immunoassays is their susceptibility to cross-reactivity. Examples of immunoassays are listed below:
Enzyme-Multiplied Immunoassay Technique (EMIT)
Fluorescence polarization immunoassay (FPIA)
Kinetic inhibition of microparticles in solution (KIMS)
Cloned enzyme donor immunoassay (CEDIA)
CEDIA and EMIT are commonly used as screens for drugs of abuse.
Thin-Layer Chromatography
Thin-layer chromatography (TLC) employs a thin silica gel designed to physically separate drugs and metabolites between its phases. After a solvent is allowed to migrate up the matrix, the gel is treated with reagents to analyze substances by color change. The addition of this identification step after separation made it possible for the technology to be used for drug screening. Some extraction techniques have the advantage of allowing measurement of the concentration of the substance being evaluated.
The advantage of TLC is that it can detect several substances. However, it is limited by a number of factors:
Detection can be hampered if the quantity of substance present is low.
TLC does not always allow the quantity to be determined.
TLC is labor intensive if multiple extractions are required (but new commercial kits have reduced the labor requirement for urine screening).
Detection limits vary with the test.
Preparation for chromatography can require the introduction of organic solvents for extraction.
High-Performance Liquid Chromatography
High-Performance Liquid Chromatography (HPLC) involves the application of high pressure to a stationary column. Drugs are identified by retention time in the column and ultraviolet spectroscopy—the amount of light absorbed is compared to a standard. The process has been automated to allow the processing of multiple columns with various solvents and light spectra. It has also been computerized to facilitate the comparison of retention times and spectra. The main disadvantage of high-performance liquid chromatography is its costly equipment.
Gas Chromatography/Mass Spectroscopy
Gas chromatography is available as a qualitative or quantitative method for volatile organic compounds. The compounds are separated by partitioning between the mobile gas phase and the stationary phase. Methanol, ethylene glycol, isopropanol, and basic drugs (sedatives, hypnotics, opioids) can be detected using this technique. The addition of mass spectroscopy can confirm, quantify, and identify
larger groups of substances; libraries can be built to identify hundreds of drugs and their metabolites.
larger groups of substances; libraries can be built to identify hundreds of drugs and their metabolites.
New Drugs of Abuse
γ-Hydroxybutyrate and Related Compounds
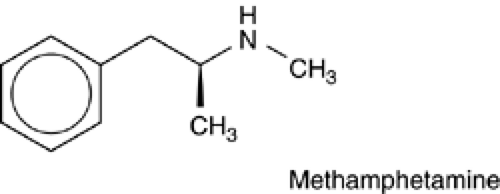
GHB and related compounds γ-butyrolactone (GBL) and 1,4-butanediol (BD) (Fig.12.1) are used to induce recreational euphoria, for intentional attempts to intoxicate (as in date-rape cases), and as a purported bodybuilding agent. GHB is also used for the treatment of cataplexy, under the trade name Xyrem (Orphan Medical, Inc., Minnetonka, Minnesota). Varied effects are attributed to GHB and its relatives: improved mood, decreased anxiety, enhanced libido, amnesia, sleep, and muscular development. These compounds, under multiple names (Table 12-1), and the recipes for their manufacture can be found on the Internet. Liquid preparations that are manufactured may have dye additives in a variety of colors, so the reported color of the liquid might not be useful in identification. Hygroscopic-powder versions of the substances can be found packaged in capsules. The precursors of GHB (GBL and BD) are components of cleaners, paint removers, and other industrial chemicals. GHB and its related compounds are typically ingested orally, at times with alcohol or other sedative/hypnotic agents.
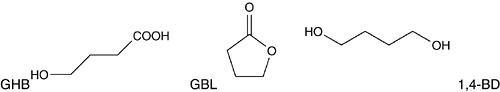 Fig. 12.1 Chemical structures of γ-hydroxybutyrate (GHB) and its precursors, γ-butyrolactone (GBL) and 1,4-butanediol (BD) |
Table 12.1. Street and Chemical Names for γ-Hydroxybutyrate and related compounds | ||||||||
|---|---|---|---|---|---|---|---|---|
|
GHB has gained considerable attention as an agent used to facilitate sexual assault; the liquid form of the product can be concealed in drinks, although some people describe a salty, soapy, or chemical taste. The true scope of GHB-facilitated sexual assault is unknown. Underreporting, lack of confirmatory laboratory testing, and the relatively short period of time the drug can be detected in urine compound the difficulty in determining the actual incidence. Most hospital laboratories do not test for GHB.
Detection Methods
Laboratory analysis for the presence of GHB can be challenging because the compound occurs naturally in the body (in the brain, kidney, heart, and skeletal muscle (7,8) and because ingested product is eliminated rapidly. GHB testing relies on the metabolism of BD and GBL in vivo. After analyzing samples from subjects presumed to be drug free, Elian (9) recommended cutoff values for endogenous levels of GHB of 1,000 μg per dL for urine and 500 μg per dL for blood. Chemists have also converted samples of GHB into GBL to facilitate analysis and have developed a method for direct analysis involving solid-phase and liquid–liquid extraction followed by gas chromatography/mass spectrometry (GC/MS) (10). Capillary electrophoresis has been reported as useful in the identification of GHB in both urine and serum (11). Availability of results depends on the capabilities of in-house or reference laboratories; many hospitals send specimens to reference laboratories.
It may be important for legal or forensic reasons to correctly identify the specific agent—GHB, GBL,
or BD—involved in a case. Some techniques for GHB identification can lead to shifts in chemical equilibrium between GHB and the lactone, GBL. But if the exact identification of GHB is needed, this should be communicated to the laboratory. Depending on the technique used, interference can come from urea or β-hydroxybutyric acid because of their similar spectral qualities but this can be controlled by laboratory techniques.
or BD—involved in a case. Some techniques for GHB identification can lead to shifts in chemical equilibrium between GHB and the lactone, GBL. But if the exact identification of GHB is needed, this should be communicated to the laboratory. Depending on the technique used, interference can come from urea or β-hydroxybutyric acid because of their similar spectral qualities but this can be controlled by laboratory techniques.
Other testing methods have been marketed to consumers concerned about the use of GHB and other substances for drug-facilitated sexual assault. An interesting drug-detection coaster is commercially available. The user is instructed to place a drop of a suspected drug-laced drink on the coaster. A color change indicates the presence of a “date-rape” drug. Analysis of this product showed that it does have some ability to detect GHB and ketamine, but its sensitivity is hampered by the need for high drug concentration, the matrix of the beverage, and the time requirement for the ketamine reaction (12).
Clinical Presentation
The clinical presentation of people intoxicated with GHB ranges from drowsiness to dose-related central nervous system depression, including respiratory depression. Alcohol can have an additive effect. Other reported effects include combative behavior and agitation. Symptoms can range from euphoria, amnesia, hypotonia, hypothermia, bradycardia, Cheyne-Stokes respiration Cheyne-Stokes respiration, coma (maybe altering with agitation), seizures or seizure-like activity, salivation, myoclonic movements, severe respiratory depression, and death (13,14,15,16). A more bizarre presentation involved self-mutilation: a woman under the influence of GHB extracted many of her own teeth (17).
Most patients will recover in 6 hours. In general, supportive care is sufficient, but respiratory support might be required in severe poisoning. Severe GHB presentation can be confirmed with GHB levels, but quantitative serum levels do not correlate with the degree of coma or time to awakening (18). Coingestions should be considered. In a study of blood specimens of 149 suspected GHB cases, 54 specimens confirmed GHB; other substances found were ethanol, MDMA, marijuana, methamphetamine, cocaine, and citalopram (19). Another interpretation of these findings is that many patients who present with GHB as the suspected cause of their symptoms are not confirmed by positive GHB test results. A withdrawal syndrome is recognized as a consequence of chronic dosing and dependence on GHB. Its manifestations can include anxiety, insomnia, psychosis, and, in some cases, severe delirium with autonomic instability (20).
Amphetamines
The use and abuse of methamphetamine (Dphenylisopropylmethylamine hydrochloride) (Fig. 12.2) and amphetamine (β-phenylisopropylamine) in the United States and other countries date back to the 1930s. From the 1960s through the 1980s, amphetamine derivatives (“designer amphetamines”) developed a following. Illicit “chemists” had two goals in mind when modifying the structure of amphetamine: to avoid regulations and to induce effects such as hallucination. Some of their creations are well known (Table 12-2), for example, Ecstasy (MDMA), which has become especially popular as a “club drug”; others, such as Para-methoxyamphetamine (PMA), have had waxing and waning popularity.
Table 12.2. Street and Chemical Names for “Designer” Amphetamines | ||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Because of the pleasure associated with their use, amphetamines are classified as “entactogens.” Entactogens are generally believed to lack the major changes in perception and thought that are induced by hallucinogens, but they induce feelings of closeness, euphoria, and, for some, empathy with fellow partygoers (21). These effects are likely related to the drug’s entactogen properties as well as its effects on seratonin, norepinephrine, and dopamine. Hallucinogenic properties of some amphetamine derivatives, methoxyamphetamines, have been described, including hallucinations and alterations in visual perception.
Props are associated with MDMA use in certain circles, for example, fluorescent light sticks and jewelry, mentholated ointments, and lollipops and infant pacifiers for mediation of the bruxism that can follow ingestion.
The most common route for ingestion of MDMA and related compounds is oral (through tablet, capsule, or drug-impregnated paper or sugar cube). It can also be taken intravenously, by nasal insufflation, and by smoking. Designer amphetamines in compressed pill format often have imprints such as cartoon characters or trademarks on one or both sides of the tablet. Websites such as http://www.dancesafe.org offer information about these imprints, but identification by this method is not definitive.
Detection Methods
Most hospital laboratories use the immunoassay technology to test for amphetamines. Some
immunoassays do not react with all of the designer amphetamines and therefore give false-negative reports regarding the presence of amphetamine derivatives. Any amphetamine analysis must consider cross-reactions with products such as pseudoephedrine, ephedrine, phenylpropanolamine, and L-methamphetamine (22,23,24). EMIT has a monoclonal antibody component for amphetamine and methamphetamine and therefore can be selective for those compounds as well as 3,4-methylenedioxyamphetamine (MDA) and MDMA. The FPIA, radioimmunoassay (also used for blood and tissue analysis), CEDIA, and enzyme-linked immunosorbent assay might be limited by cross-reactivity to varying extents with MDA and MDMA. Since so many detection methods are available, and improvements to them are being made continuously, the clinician should confirm the sensitivity and specificity of the laboratory’s analytic method before reaching a definitive conclusion about the results. Consultation with a forensic or clinical chemist should be considered. Case evaluation should include a review of the patient’s legitimate medication use. For example, L-deprenyl (Selegiline), used to manage Parkinson’s disease, is converted in vivo into L-methamphetamine and L-amphetamine but not into the D-enantiomers. This will present as a positive result on some amphetamine screens. The variety of amphetamines available makes the task of specific and rapid testing a challenge at best. The specific amphetamine can be typed definitively with GC/MS.
immunoassays do not react with all of the designer amphetamines and therefore give false-negative reports regarding the presence of amphetamine derivatives. Any amphetamine analysis must consider cross-reactions with products such as pseudoephedrine, ephedrine, phenylpropanolamine, and L-methamphetamine (22,23,24). EMIT has a monoclonal antibody component for amphetamine and methamphetamine and therefore can be selective for those compounds as well as 3,4-methylenedioxyamphetamine (MDA) and MDMA. The FPIA, radioimmunoassay (also used for blood and tissue analysis), CEDIA, and enzyme-linked immunosorbent assay might be limited by cross-reactivity to varying extents with MDA and MDMA. Since so many detection methods are available, and improvements to them are being made continuously, the clinician should confirm the sensitivity and specificity of the laboratory’s analytic method before reaching a definitive conclusion about the results. Consultation with a forensic or clinical chemist should be considered. Case evaluation should include a review of the patient’s legitimate medication use. For example, L-deprenyl (Selegiline), used to manage Parkinson’s disease, is converted in vivo into L-methamphetamine and L-amphetamine but not into the D-enantiomers. This will present as a positive result on some amphetamine screens. The variety of amphetamines available makes the task of specific and rapid testing a challenge at best. The specific amphetamine can be typed definitively with GC/MS.
TLC is used in several commercially available systems, such as TOXI-LAB (Varian, Palo Alto, California). The accuracy of TLC in detecting amphetamine and methamphetamine is limited, however, because many of the sympathomimetic amines (pseudoephedrine, phentermine, ephedrine) have color characteristics similar to theirs. Techniques have been added to some TLC technologies to allow differentiation of selected amines.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree