Fig. 32.1
Frame-based stereotactic guidance for deep brain lead placement (left). Frameless stereotactic guidance for deep brain lead placement (right)
Stereotactic localization of bilateral entry points is performed and these areas are then marked. The head is shaved, prepared, and draped in the standard sterile fashion. Incisions are opened and meticulous hemostasis achieved. Two 14-mm bur holes are then drilled bilaterally centered over the prior stereotactic localization points. A number of frame, miniframe, or frameless systems are now available; however, the general principles are similar. Registration is performed with the intraoperative navigation station and less than 0.5 mm error is preferred.
Once exposure is achieved, physiological microelectrode recording is performed to achieve optimal electrode positioning. It is a key point to remember that the stereotactic coordinates represent the starting point for target identification, but that the end target is identified in the operating room.
The dura, pia, and cortical surface are coagulated and incised on one side, beginning contralateral to the patient’s worst symptoms. The trajectory is aligned using the previous target and entry projection. Initial depth is commonly set to 10 mm above target, ensuring that the patient’s blood pressure is normotensive. Electrophysiological activity is typically used to identify exact targets. This is done by microelectrode recording and microelectrode stimulation followed by macrostimulation. The microelectrode is advanced in a stepwise fashion, continuously recording. A DBS electrode is then measured to the appropriate length and introduced to the target point (Fig. 32.2). Test stimulation is carried out with the goal of minimal adverse effects with good therapeutic benefit. Once the lead position has been confirmed, the outer cannula is withdrawn and a skull fixation device is fastened to ensure that the electrode is held firmly in place. The leads are connected to temporary externalized extensions for a trial phase of stimulation.
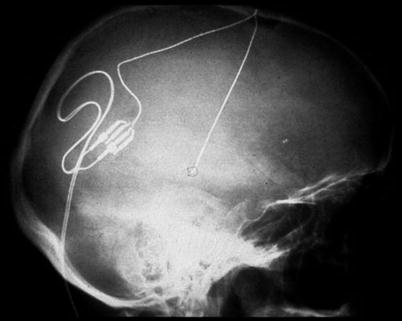
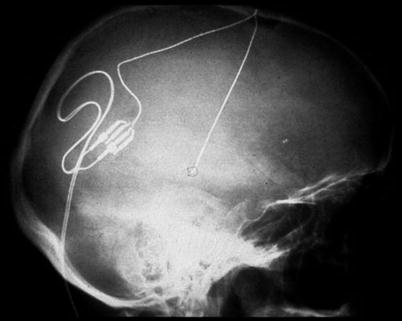
Fig. 32.2
Final lead placement for DBS target
In the postoperative period, close attention to blood pressure control is performed and the postoperative CT or MRI performed to confirm accurate electrode placement and to rule out any evidence of intracranial hemorrhage. In general, combined stimulation of periventricular gray (PVG) and ventral posterior lateral thalamus (VPL) has been superior to single-lead stimulation. In most patients a certain subperception threshold is needed to produce a pain-relieving effect. If appropriate and acceptable pain relief is achieved, the patient is brought back to the operating room, where the temporary connector is removed and a permanent extension cable is used to connect to the lead to the implanted pulse generator. A subcutaneous pocket is prepared for the internal generator and the extensions are passed through the subcutaneous tissue to connect the system. If the system fails to provide relief, the patient is not a candidate for a permanent device, and the lead is explanted.
32.3 Risk Assessment
1.
Mortality from DBS is a rare complication that occurs in less than 0.4 % of patients.
2.
Neurological compromise occurs in less than 1.3 % of patients on a permanent basis.
3.
The most devastating risk of DBS is intracranial hemorrhage. Hemorrhages are identified in 2–5 % of patients receiving DBS and can occur at the time of implant or at the time of removal. Asymptomatic hemorrhage occurs in 1.9 % of implanted patients, where symptomatic hemorrhage occurs in 2.1 % and hemorrhage resulting in death or permanent deficit in 1.1 %. Postimplantation infarcts occur in under 1 % of patients [1].
4.
Infection rates vary among institutions and have been reported between 1% and 13 %. Infectious complications can include meningitis, encephalitis, skin infection, sepsis, and death [2].
5.




Hardware-related complications including lead fracture, short circuit, and electrode migration occur in under 4 % of cases. Loss of effective stimulation coupled with imaging evidence of fracture or persistent high or extremely low impedance readings across several contacts of the electrode are most indicative of a hardware failure [3].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








