Neurophysiology of Tension-Type Headaches
Jean Schoenen
Lars Bendtsen
Various neurophysiologic methods have been used in patients with tension-type headache. By far, the most frequent reports have dealt with electromyographic (EMG) recordings of pericranial muscle activity. This situation is explained easily by the fact that in the former Headache Classification of the Ad Hoc Committee (1), tension headache was used as a synonym for muscle-contraction headache, and was considered to be “associated with sustained contraction of the skeletal muscles in the absence of permanent structural change, usually as part of the individual’s reaction to life’s stress.” Contrary to the first edition, the second edition of the Headache Classification prepared by a subcommittee of the International Headache Society (ICDH-II) (30) has abandoned this concept, since the three-digit code subtypes are now identified according to presence (code 1) or absence (code 2) of pericranial tenderness without reference to pericranial muscle contraction.
Recently, attention has focused on the inhibitory reflexes of the jaw-closing muscles (66). Other neurophysiologic methods, in particular those exploring the activity of the brain, such as electroencephalography (EEG), have not disclosed any clear-cut abnormality in tension-type headache (63), as is also the case for contingent negative variation, an event-related potential, which is abnormal in migraine between attacks but normal in tension-type headache (63). By contrast, abnormalities have been found in tension-type headache with nociceptive-specific laser-evoked potentials (16).
ELECTROMYOGRAPHY
Contraction of head and neck muscles has been thought to play a pathogenetic role in some patients with tension-type headache. Contradictory results have been reported by recording pericranial muscular activity in tension-type headache or, as previously termed, muscle-contraction headache. Relevant data obtained with surface EMG recordings are summarized in Table 71-1, in which positive data are those that favor a role of increased muscular activity in the pathogenesis of tension-type headache, and negative data represent those that do not. Most of the EMG studies published up to 1983 were critically reviewed by Pikoff (53): About half of the studies appeared to be normal, and in the other half, it was concluded that pericranial EMG levels were increased. Most subsequent studies, however, tend to indicate concordantly that EMG levels are abnormal compared with controls, despite wide variations in experimental conditions. For instance, EMG levels were found to be increased in tension headache sufferers during postural changes (71), during mental stress (17), and during the headache phase compared with the headache-free interval (54) by analyzing the increment of EMG between rest and maximal contraction (74) or by comparing different electrode placements (29). In a recent study (26) of episodic tension-type headache sufferers recorded in the headache-free phase, higher levels of average temporal EMG levels were found in the patient group compared with controls. Because only 11% of headache subjects had elevated (two or more standard deviations higher than the mean of controls) EMG activity in at least one muscle, it was believed that EMG data were of little use in assigning individual subjects to diagnostic groups.
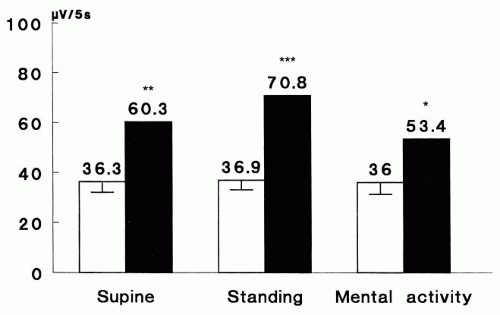
We recorded EMG activity in 32 female patients suffering from chronic tension-type headache (code 2.2) over the frontalis, temporalis, and trapezius muscles in supine and standing positions as well as during a mental task (66). On average, EMG activity was significantly higher in patients compared with healthy female volunteers of comparable ages, and this was the case in all three muscles studied and under any condition (Fig. 71-1). Of the patients, 62.5% had at least one EMG level exceeding the mean control values by two standard deviations. Among these patients, five
had one abnormal value (of a maximum of six), and only two patients had six abnormal values. If one muscle and one condition were considered, for example, the frontalis in the supine position, 11 patients (34%) would have been considered abnormal. No correlation was found between EMG levels and headache severity or the score on an anxiety scale or pressure pain thresholds. After 10 sessions of muscular biofeedback therapy, EMG levels tended to decrease in all muscles, but this modification was significant only in some muscles and under certain recording conditions. After biofeedback therapy, a slight but significant positive correlation was found between improvement in the headache severity index and maximal reduction of EMG levels; that is, the EMG level that decreased the most considering the three recording sites and the three conditions. Another study found no significant clinical difference between patients with abnormal EMG values and those in whom all EMG recordings were normal (67).
had one abnormal value (of a maximum of six), and only two patients had six abnormal values. If one muscle and one condition were considered, for example, the frontalis in the supine position, 11 patients (34%) would have been considered abnormal. No correlation was found between EMG levels and headache severity or the score on an anxiety scale or pressure pain thresholds. After 10 sessions of muscular biofeedback therapy, EMG levels tended to decrease in all muscles, but this modification was significant only in some muscles and under certain recording conditions. After biofeedback therapy, a slight but significant positive correlation was found between improvement in the headache severity index and maximal reduction of EMG levels; that is, the EMG level that decreased the most considering the three recording sites and the three conditions. Another study found no significant clinical difference between patients with abnormal EMG values and those in whom all EMG recordings were normal (67).
TABLE 71-1 Pericranial Surface EMG Activity | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||
Studies of the possible relation between pericranial EMG activity and stressful situations have produced conflicting results. Increased EMG activity during laboratory stressors have been reported in tension headache patients (13,18,75). Conversely, a large group of investigations did not find a reliable difference between the EMG activity of tension-type headache patients and headache-free controls in their response to laboratory stressors (3,4,7,17,19,44,66,72,76). In a recent study using ambulatory EMG recordings, higher levels of EMG activity were found on “high-stress days” both in headache-free students and in students with episodic tension-type headache; however, no statistically significant difference was found between the two groups (26,58).
Evidence has been found that pericranial and neck muscle activity is neither quantitatively nor chronologically related to head pain. The EMG levels are not higher in more severely affected patients (31,58,61,67); during prolonged ambulatory EMG recordings, muscle activity varies with daily activities and stress but not with pain levels (12,58). During an actual headache, EMG levels increased over the frontalis muscle in only one population-based study (34), but not in patients (12,35). No difference in EMG levels was found between chronic tension-type headache associated (code 2.2.1) or unassociated (code 2.2.2) with a muscular disorder in one study (67); on the other hand, levels were higher than those in healthy controls in only the 2.2.1 subgroup in another study in which normal EMG levels were found in both subgroups of episodic tension-type headache (32). Two subgroups of episodic tension-type headache sufferers were distinguished on the basis of their pericranial EMG response to experimental pressure-induced pain over the temples, one group with an exaggerated EMG activity and the other with an abnormally low EMG response (23).
Ischemic pain induced in the arm by a tourniquet was not accompanied by higher EMG levels in tension-type headache sufferers compared with controls, although the headache patients rated the tourniquet as more painful (39). Tooth clenching may induce headache in tension-type headache sufferers and has been used as a model to study pathogenetic mechanisms (35). The headache, however, increases gradually over several hours and is associated with pericranial EMG levels that are somewhat lower than the initial ones (35); these levels also can be produced in 54% of migraine patients (33).
It has been argued that myofascial pain syndromes could be related to changes in the viscoelastic properties of muscles, that is, so-called thixotropy (70). The recent findings (using a new device, the muscle hardness meter) of increased muscle stiffness in tension-type headache sufferers, irrespective of the presence of headache (6,59) favors such a mechanism. Within the same concept, the pain in tension-type headache might be caused by muscle contracture; in this case, increased electric activity would be localized at the level of trigger points (70). With monopolar needle EMG recordings, increased activity was found at trigger points in patients with chronic tension-type headache (28), more often during experimental stress (45). It is not clear whether the EMG activity was recorded from muscle spindles or from the motor end plate zone, and some investigators did not find any abnormality when placing needle electrodes in trigger points. In one recent study, botulinum toxin injections decreased after 12 weeks temporalis EMG levels in patients with chronic tension-type headache, but not the headache, which another indication that muscle activity per se is not the culprit in chronic tension-type headache (56).
To summarize, EMG recordings have no diagnostic usefulness in tension-type headache, although they may help in understanding its pathogenesis. Contradictory results have been reported for EMG levels of pericranial and neck muscles. Some of these contradictions may be attributable to the different recording conditions. Taken together, however, the published results indicate that there is no causal relationship between the headache and surface EMG activity, although some patients may have EMG levels over certain muscles that exceed those of control subjects. In this respect, the findings may be comparable to those reported in chronic low back pain, where muscle activity is considered a normal protective adaptation and not the cause of pain (5,43). It remains to be determined whether muscular contracture and muscle hardness or localized muscle fiber contraction under trigger or tender points play a role in the initiation or the boosting of pain in tension-type headache. In future studies it is also worthwhile to explore more accurately frequency-related subtypes of tension-type headache by using the new ICHD-II subdivision into infrequent (<1 day per month), frequent (>1 but <15 days per month), and chronic (>15 days per month) forms, and the more stringent diagnostic criteria for TTH proposed in the ICDH-II appendix (A2) (30).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree