Neurophysiologic Testing in Pain Management
Annabel D. Edwards
Lisa S. Krivickas
As to pain, I am almost ready to say the physician who has not felt it is imperfectly educated.
—R. Weir Mitchell
I. INTRODUCTION
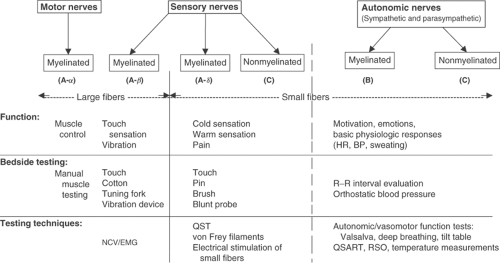
When physiologists learned that nerve transmission is based on electrical principles, they began to devise ways to measure neuronal activity. Pain signals are communicated through the peripheral and central nervous systems and are interpreted supraspinally. The understanding that small and large sensory fibers play different roles in various pain states has led to differential nerve fiber testing. Parts of the nervous system that are not normally involved in pain messaging, such as the sympathetic and parasympathetic systems, can become involved in certain disease states, after injury, and/or following sensitization. Neuronal activity in various afferent systems can overlap and connect or change functionally (both anatomically and at a cellular and molecular level), creating a particularly complex challenge for the diagnosis and treatment of some pain problems. Evaluation of such a potentially confusing network of neurons can be a challenge.
Neurophysiologic testing is broad in scope and has developed over a long time. Although electrodiagnostic studies were said to have been performed by Swammerdam in the 1600s, it was not until the mid-1900s that the testing progressed to the point of clinical usefulness. Electrodiagnostic studies can assess the function of large-diameter sensory and motor nerve fibers, localize focal peripheral nerve lesions, and evaluate overall peripheral nerve function. Autonomic nervous system (ANS) testing helps
elucidate the role of sympathetic and parasympathetic nerves in the processing and modulation of pain states, although there is no clearly defined pattern of ANS response that is recognized as demonstrating the presence of “chronic pain.” Quantitative sensory testing (QST) techniques [warm sensation (WS) and cool sensation (CS), hot pain (HP) and cold pain (CP), electrical stimulation, etc.], although not as objective as electrodiagnostic testing, can help evaluate the function of small-diameter nerve fibers (nociceptive fibers) in the entire sensory pathway, and cannot be used to localize nerve lesions. Used in combination, these neurophysiologic tests can provide information about the neuronal mechanism(s) involved in pain.
elucidate the role of sympathetic and parasympathetic nerves in the processing and modulation of pain states, although there is no clearly defined pattern of ANS response that is recognized as demonstrating the presence of “chronic pain.” Quantitative sensory testing (QST) techniques [warm sensation (WS) and cool sensation (CS), hot pain (HP) and cold pain (CP), electrical stimulation, etc.], although not as objective as electrodiagnostic testing, can help evaluate the function of small-diameter nerve fibers (nociceptive fibers) in the entire sensory pathway, and cannot be used to localize nerve lesions. Used in combination, these neurophysiologic tests can provide information about the neuronal mechanism(s) involved in pain.
Neurophysiologic testing is useful because it
helps detect underlying pathology;
helps define pain mechanisms;
helps anatomically localize pain instigators;
helps focus treatments on mechanisms;
helps predict if patients will respond to particular treatments by clarifying mechanisms;
used sequentially, helps monitor disease progress and response to treatment;
may have medico-legal applications;
advances pain research by providing quantitative and reproducible measurements of pain and its various mechanisms.
In clinical practice, neurophysiologic testing is useful when a diagnosis is elusive or when a pain problem has been refractory to treatment. Neurophysiologic testing can be time-consuming and is not appropriate for all patients. Patients should be tested only if their condition is likely to be better managed because of the results. Figure 1 summarizes the utility of various tests for different parts of the nervous system.
II. ELECTRODIAGNOSTIC TESTING
Electrodiagnostic testing is used to diagnose peripheral nervous system disorders. These include radiculopathies, plexopathies, mononeuropathies, and generalized peripheral neuropathies. Occasionally, myopathic disorders such as myotonic dystrophy type II present with pain as a chief complaint. A more focused treatment plan can be devised by localizing the source of a patient’s pain to a specific location in the peripheral nervous system. A normal electrodiagnostic evaluation can also help narrow the differential diagnosis when the pain is of unclear etiology. Electrodiagnostic studies are normal in patients with only central nervous system pathology and in those with only small fiber neuropathy or sources of pain.
Routine electrodiagnostic evaluations [often referred to as EMG (electromyogram)] comprise nerve conduction studies (NCSs) and needle electrode examination (NEE). An electrodiagnostic study must include both components to provide a complete assessment of peripheral nervous system function. The results can assist in determining the severity of a lesion and the prognosis for recovery.
1. Nerve Conduction Studies
NCSs are performed by electrically stimulating a nerve and then by recording a response from either the nerve itself or a muscle it innervates. The two basic types of NCS are motor and sensory. An additional category of study is called the “late response,” which includes detection of a characteristic wave (F wave) or a reflex (H reflex). The parameters assessed in NCSs are the amplitude of the response, the latency (time between nerve stimulation and response generation), and the nerve conduction velocity (NCV). These parameters are compared with established sets of normal values. The amplitude reflects the number of intact axons, and the distal latency and conduction velocity reflect the integrity of the myelin sheath. Therefore, amplitude is reduced in axonal nerve lesions, and conduction velocity is reduced in demyelinating lesions.
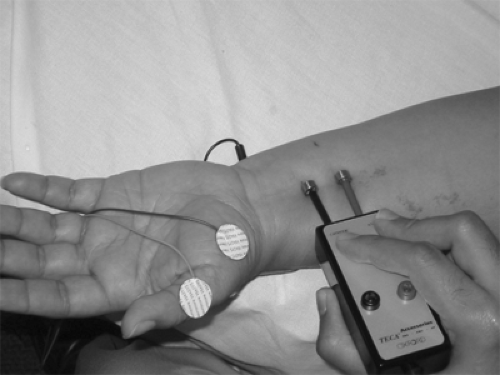
Motor NCSs are performed by stimulating a motor nerve and by recording a compound motor action potential (CMAP) from the belly of a muscle innervated by that nerve. For example, the median motor study is performed by stimulating the median nerve at the wrist and by recording a CMAP from the abductor pollicis brevis (APB) muscle, as pictured in Figure 2. The nerve is then stimulated at a more proximal site so that a conduction velocity may be calculated between the two sites of stimulation.
Sensory NCSs are performed by stimulating sensory nerves and by recording sensory nerve action potentials (SNAPs). For example, the median sensory study is performed by stimulating the median nerve at the wrist and by recording a SNAP from the digital nerves of the second finger. SNAPs are much smaller in amplitude than CMAPs because they are nerve-generated potentials rather than muscle-generated potentials.
When assessing the results of NCSs, amplitude measurements are as important, if not more important, than NCV because most nerve lesions are primarily axonal rather than demyelinating. Amplitudes correspond to clinical symptoms such as pain, weakness, and sensory loss, whereas demyelination itself does not cause any symptoms.
2. Needle Electrode Examination
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree