Section IV Nicholas Qandah, Evan A. Houck, and Dan Miulli As with other medical conditions, neurosurgical conditions can be treated or ameliorated with medications. The foremost consideration when initiating care in the neurosurgical intensive care unit is to restore cerebral blood flow, thus delivering essential oxygen and substrates that would allow the brain to heal. The brain needs an adequate cardiac output and ample pulmonary function to survive. Blood pressure must be restored to a range that is not so low it leads to neuronal death or so high that it leads to hyperemia, increased edema, and even hemorrhage. This chapter examines the medications used in conjunction with neurosurgical procedures. We discuss hemodynamic medications for lowering and raising blood pressure, electrolyte solutions to assist the body in dealing with all manner of insult, blood products to replace losses, antiepileptics to control seizures, steroids to treat tumors or as an adjunct in certain types of spinal cord injuries, anticoagulants, sedatives to calm patients or decrease the cerebral metabolic rate of oxygen consumption, pain medications, and antiemetics; and when too much medication is given the agents to reverse the effects. Before treating increased blood pressure, it is important to rule out intracranial causes, such as Cushing’s reflex. Before choosing an agent, evaluate the effects of the drug on CPP and ICP. Always remember to order blood pressure and heart rate parameters when writing for a drug.1,2 Action: Reacts with oxyhemoglobin to form cyanide and nitric oxide (NO). NO stimulates cyclic guanosine monophosphate (cGMP) production, causing potent vasodilation (arterial > venous), hepatic and renal metabolism.1,3 Contraindications: Increased ICP, intracranial mass lesion (raises ICP), pregnancy1 Rx: Intravenous (IV) drip 0.25 to 8 μg/kg/minute. To prepare: 50 mg in 500 mL dextrose 5% in water (D5W) = 100 μg/mL; can be double concentrated to reduce fluid or glucose load1,4 Side effects: “Cerebral and coronary steal” phenomenon due to preferential peripheral vasodilation before cerebral vasodilation. Thiocyanate/cyanide toxicity causes neurologic deterioration and hypotension (cover bottle with foil: light sensitive). Nausea, diuresis, platelet inhibition; may increase ICP.1,3 Action: Releases NO, resulting in guanylyl cyclase stimulation of cGMP synthesis. Acts predominantly on venous capacitance vessels, affecting arterial vascular smooth muscle at higher concentrations. Primarily venodilation without reflex tachycardia1,3 Contraindication: Increased ICP or decreased cerebral perfusion1,2 Rx: IV drip 10 to 20 μg/minute (increase by 5–10 μg/minute q 5–10 minute)1,3,4 Side effects: Does not cause “coronary steal”; can cause transient increase in ICP, headache, hypotension, rebound hypertension, and methemoglobinemia1–4 Action: Blocks α-1 selective, β nonselective; hepatic glucuronide conjugation; may lower ICP1,3 Contraindications: Asthma, pregnancy1 Rx: Give each dose slow intravenous push (IVP) (over 2 minutes) q 10 minutes until desired blood pressure (BP) achieved; dose sequence: 20, 40, 80, 80, then 80 mg (300 mg total). Once controlled, use = same total dose IVP q 8 hours. Alternative: IV drip: add 40 mL (200 mg) to 160 mL of intravenous fluids (IVF) (result 1 mg/mL). Run at 2 mL/minute (2 mg/minute) until desired BP (usual effective dose 50–200 mg) or until 300 mg given, then titrate rate. Bradycardia limits dose; increase slowly because effect takes 10 to 20 minutes. Oral (PO) dose: start with 200 mg bid if converting from IV; otherwise, start 100 mg PO bid and increase 100 mg/dose q 2 days, maximum 2400 mg/day.1–4 Side effects: Fatigue, dizziness, orthostatic hypotension1,3 Action: Direct arteriolar smooth muscle vasodilator; may act through NO or calcium1,3 Contraindication: Liver metabolism; slow acetylators should not receive >200 mg/day—may induce lupus-like syndrome.1,3 Rx: 10 to 20 mg q 15 to 20 minutes, maximum 40 mg; repeat prn1,3,4 Side effects: Nausea/vomiting, headache, increased intracranial blood flow, reflex tachycardia1,3 Action: Short-acting selective β-1 antagonist; metabolized by red blood cell (RBC) esterase, urinary excretion; may lower ICP1,3 Contraindication: Avoid in congestive heart failure (CHF)1 Rx: Mix 5 g/500 mL normal saline (NS), give IV 500 μg/kg loading dose over 1 minute, follow with 4 minute infusion starting with 50 μg/kg/minute. Repeat loading dose and increment infusion rate by 50 μg/kg/minute q 5 minutes. Rarely >100 μg/kg/minute required. Doses >200 μg/kg/minute add little.1,2,4 Side effects: Dose-related hypotension; resolves within 30 minutes of discontinuation (D/C). Less bronchospasm than other β-blockers.1,2 Action: Slow calcium-channel antagonist; relaxes vascular smooth muscle without reflex tachycardia1 Contraindications: Sick sinus syndrome, wide complex tachycardia, Wolff-Parkinson-White (WPW) syndrome, second-degree or greater atrioventricular (A-V) block and concurrent β-blockers1,3 Rx: 20 mg IV over 2 minutes; 0.25 mg/kg. May repeat 1 × in 15 minutes if response is inadequate. Not suggested as a drip for neurosurgical patients.1 Side effects: Hepatitis, edema, blurred vision, flushing, injection site reaction1,3 Action: Short-acting calcium-channel blocker. Decreases systemic vascular resistance; increases cardiac index, cerebral blood flow (CBF) (by 10–20%), glomerular filtration rate (GFR), and Na+ retention1,3 Contraindications: Hypersensitivity, acute myocardial infarction (MI)1,3 Rx: PO 10 to 20 mg, faster onset with sublingual/buccal administration (puncture capsule) or if chewed. If no response after 20 to 30 minutes, give additional 10 mg.1,3,4 Side effects: Flushing, headache, palpitation, edema, reflex tachycardia1,3 Action: The only second generation IV dihydropyridine calcium channel blocker. Contraindications: Can often cause neurologic worsening in patients with stroke, intracerebral hemorrhage, and subarachnoid hemorrhage. Nicardipine IV drip is the relative large volume of fluid needed (up to 150 cc/hour). Has been shown to increase intracranial pressure in some limited animal and human studies. Rx: Nicardipine drip 25 mg/250 cc in 250 cc of normal saline (NS), on a pump for a concentration of 0.1 mg/mL Induction at a rate of 0.2 μg/kg/min, or 5 mg/hour (50 mL/hour), and may be increased in increments of 2.5 mg/hour every 5 to 15 minutes, depending upon the need to rapidly or gradually control blood pressure, to a maximum of 15 mg/hour (150 mL/hour). Once the desired level is achieved decrease rate to 3 mg/hour (30 mL/hour). Nicardipine drip is not compatible with sodium bicarbonate injection or lactated Ringer’s solution. Side effects: Dizziness, fainting, unusual weakness, lightheadedness, headache, flushing, nausea, vomiting, tiredness, swelling of the ankles/feet, frequent urination, shortness of breath, irregular heartbeat, joint/muscle pain, tingling of the hands/feet, mood changes, ringing in the ears (Candesartan, Cilexetil, Eprosartan, Irbesartan, Losartan, Mesylate, Olmesartan, Telmisartan, Valsartan) Contraindications: Hypersensitivity, pregnancy. Rx: The oral dosage depends on the specific medication used. Side effects: Headache and dizziness. Other side effects may be diarrhea, stomach problems, muscle cramps and back and leg pain, insomnia, nasal congestion, cough, sinus problems, and upper respiratory infection. Less likely to cause a cough when compared to angiotensin-converting enzyme blockers. Action: Angiotensin converting enzyme (ACE) inhibitor; may lower ICP1,3 Contraindication: Pregnancy1 Rx: Initially, start IV 1.25 mg slow over 5 minutes, then 1.25 to 5 mg q 6 hours response seen in 15 minutes; may repeat 0.625 mg in 1 hour if response is inadequate. Maximum 5 mg q 6 hours.1,3,4 Side effects: Hyperkalemia ~1%; can cause renal insufficiency, angioedema, agranulocytosis1,3 Action: Inhibits sympathetic outflow by acting on cardiovascular control receptors in the medulla oblongata1,3 Contraindication: Hypersensitivity1 Rx: Rapid control: 0.2 mg PO, then 0.1 mg PO q 1 hour; stop at 0.8 mg total or if orthostatic. Maintenance dose: 0.1 mg PO bid or tid; increase slowly to maximum 2.4 mg/day (usual 0.2–0.8 mg/day). Patch 0.1 mg, 0.2 mg, 0.3 mg/week titrate to desired effect; maximum 0.6 mg/week.1,3,4 Side effects: Tachycardia rare; mild confusion/sedation; fluid retention, dry mouth, constipation, rebound hypertension1 The appropriate evaluation of the patient’s volume status and monitoring, including central venous pressure (CVP), Swan-Ganz catheterization, and arterial line, are essential to treat hemodynamic instability. IVF is always first line.2 Action: Primarily a vasoconstrictor; 25% of dopamine given is rapidly converted to norepinephrine (NE). At doses >10 μg/kg/minute, α, β, and dopaminergic effect (essentially giving NE). At 2 to 10 μg/kg/minute, primarily β-1, positive inotrope. At 0.5 to 2.0 μg/kg/minute, primarily dopaminergic, vasodilating renal, mesenteric, coronary and cerebral vessels, positive inotrope.1,3 Contraindication: Pregnancy class C1,3 Rx: Mix 800 mg/250 mL NS, central line. Start with 2 to 5 μg/kg/minute and titrate for response; maximum 20 μg/kg/minute.1–4 Side effects: Tachycardia, peripheral vasoconstriction, arrhythmias, hyperglycemia1,3 Action: Racemic mixture: L-isomer is α-agonist, D-isomer nonspecific; β-agonist comparable to dopamine and nitroprusside1,3 Contraindication: Hypertrophic cardiomyopathy1 Rx: Mix 500 mg/250 mL NS. Usual range 2.5 to 10.0 μg/kg/minute; rarely, doses up to 40 μg used. To prepare: Put 50 mg in 250 mL D5W to yield 200 μg/mL.1–4 Side effects: Tachycardia, possibly platelet function inhibition1,3 Action: β-1 and α-1 receptor agonist1 Contraindications: Hypertrophic obstructive cardiomyopathy, tetralogy of Fallot (right ventricular [RV] outflow tract obstruction)1,3 Rx: Mix 4 mg/250 mL NS. Initial rate 0.5 to 1.0 μg/minute. Average 4 to 16 μg/minute; maximum 30 to 47 μg/minute1,3 Side effects: Vasoconstriction (splanchnic and renal), arrhythmias1 Action: Pure α vasoconstrictor; causes reflex increase in parasympathetic tone with resultant slowing of pulse. Useful in hypotension associated with tachycardia.1–3 Contraindication: Spinal cord injuries Rx: Mix 40 mg/500 mL NS to yield 80 μg/mL; rate of 8 mL/hour = 10 μg/minute. Pressor range: Initial 100 to 180 μg/minute; maintenance 40 to 60 μg/minute1–3 Side effects: Cardiac output and renal blood flow may decrease.1 Action: Inotrope-vasodilator; inhibits phosphodiesterase III; resembles dobutamine hemodynamically with less tachyphylaxis1,3 Contraindication: Thrombocytopenia1,3 Rx: 0.75 mg/kg IV slow bolus over 2 to 3 minutes, then 5 to 30 μg/kg/minute infusion. May rebolus 0.75 mg/kg IV slow 30 minutes after starting therapy.1,3,4 Side effects: Vasodilation hypotension, 2% thrombocytopenia, and hepatotoxicity1,3 Action: Nonspecific adrenergic agonist has β-2 activity unlike NE and twice as potent ionotrope.1,3 Contraindications: Hypertrophic obstructive cardiomyopathy, tetralogy of Fallot (RV outflow tract obstruction)1,3 Rx: 0.5 to 1.0 mg of 1:10,000 solution IVP; may repeat q 5 minutes (may bolus per endotracheal tube). Drip: Start at 1 μg/minute; titrate up to 8 μg/minute (to prepare: put 1 mg in 100 mL NS)1,3,4 Side effects: Vasoconstriction (splanchnic and renal), arrhythmias1 Action: Nonselective β-receptor agonist, potent inotrope (β1), and peripheral vasodilator (β2); second-line agent after dopamine for bradycardia unresponsive to atropine1,3 Contraindications: Digitalis bradycardia, angina1 Rx: Mix 1 mg/500 ml NS = 2 μg/mL; start at 2 μg/minute, titrate up to 10 μg/minute1,4 Side effects: Tachycardia, vasodilation, increased myocardial oxygen demand1,3 Electrolytes function within a narrow therapeutic range to promote health and ameliorate disease. Increasing amounts of electrolytes are needed at times of stress but still less than would cause further harm. Hyper: Phos-Lo (calcium acetate) 2 tablets NG/PO tid with meals1,3 Action: Combines with dietary phosphate to form insoluble calcium phosphate1 Contraindications: Hypersensitivity to components, hypercalcemia, renal calculi1 Side effects: Hypercalcemia1 Hypo: Potassium phosphate 1 to 2 g qid divided NG/IV tid1,4 Action: Elevates serum phosphorus and serum potassium levels1 Contraindications: Hyperphosphatemia, hyperkalemia, hypocalcemia, hypomagnesemia, renal failure1 Side effects: Diarrhea, nausea, stomach pain1 Hyper: Treat aggressively with 0.9 NS infusion to correct volume deficit. Follow with loop diuretic (i.e., furosemide 20–40 mg IV/PO q 2–4 hours). May use zoledronate 4 mg IV over 15 minutes qid if unresponsive to loop diuretic.1,4 Hyper: Calcium gluconate 2.25 to 14 mEq slow IVP or 500 to 2000 mg PO bid/tid. Calcium chloride 500 to 1000 mg slow IVP q 1 to3 days.1,4 Action: Elevation of serum calcium1,3 Contraindications: Hypersensitivity, hypercalcemia1,3 Side effects: Extravasation necrosis, hypotension1,3 Hypo: Magnesium sulfate 1 g of 20% solution IM q 6 hours × 4 doses or 2 g IVP over 1 hour (note: monitor for hypertension); 1 g will raise serum magnesium 0.4 mEq/dL1,4 Action: Elevation of serum magnesium1 Contraindications: Heart block, serious renal impairment, myocardial damage, hepatitis, Addison’s disease1 Side effects: Hypotension, asystole, CNS depression, diarrhea, decreased neuromuscular transmission1 Hyper: Treat with D5W, IV calcium and insulin administration if severe. Kayexalate (sodium polystyrene) 1 g/kg up to 15 to 60 g PO q 6 hours prn.1,4 Action: Exchanges sodium ions for potassium ions in the intestines1 Contraindications: Hypersensitivity, hypernatremia1 Side effects: Hypokalemia, hypocalcemia, hypomagnesemia, sodium retention1 Hypo: Potassium chloride 20 to 40 mEq PO bid or 10 to 20 mEq IVP over 1 hour (note: monitor for cardiac arrhythmias)1,4 Action: Elevation of serum potassium and serum chloride1 Contraindications: Severe renal impairment, untreated Addison’s disease, hyperkalemia, severe tissue trauma1 Side effects: Diarrhea, nausea and vomiting, bradycardia, hyperkalemia, weakness, dyspnea1 Patients in the NICU should have a CBC checked daily. Blood products should be administered as needed to keep hemoglobin at ~10.0 mg/dL Platelets and plasma should be administered on a case-by-case basis. Generally, INR should be kept at 1.3 or below, platelet count >100,000.2 Each unit of packed red blood cells (PRBC) will raise hemoglobin by 0.8 mg/dL Plasma transfusion is indicated in patients with documented coagulation factor deficiencies and active bleeding, or who are about to undergo an invasive procedure with suspected coagulation factor deficiencies. Deficiencies can be secondary to congenital or acquired diseases such as liver disease, warfarin anticoagulation, disseminated intravascular coagulation, or massive replacement with red blood cells and crystalloid/collid solutions. One unit is approximately 250 mL and must be ABO compatible but not Rh factor compatible. The usual dose is 4 units to improve coagulation status by increasing factor levels of at least 10%. However, the amount will vary depending on the patient’s size and clotting factor levels. Platelets are indicated in patients with disorders of hemostasis. Platelets are collected from pooled random donors for from a single donor. If given pooled platelets, the dosage is 4 to 6 units, whereas if given from a single donor a standard pack is equivalent to 4 pooled units and a large pack is equivalent to 6 pooled units. Functional platelet count should be maintained above 100,000/microliter for patients undergoing neurosurgical procedures. Abnormal platelet function can be seen with medications such as aspirin, and with kidney disease, liver disease, malignancy, sepsis, and tissue trauma. If platelet dysfunction is present, the patient will require higher levels of platelets to achieve hemostasis. The number of units required to increase the number of platelets is dependent upon weight, being anywhere from 5000/microliter per unit for 200 lb/91 kg to 22000/microliter per unit for a 50 lb/23 kg patient. Contains fibrinogen, von Willebrand factor, factor VIII, factor XIII, and fibronectin. It comes in concentrates of 6 units. Each unit provides about 350 mg of fibrinogen. Usually 6 bags or 1 pooled bag is given, which raises the fibrinogen by 1560 mg or 45 mg/dl. Cryoprecipitate is also used to make fibrin glue. Action: Modulates voltage-gated Na and Ca neuron channels and enhances Na/K adenosinetriphosphatase (ATPase) neuronal and glial activity. Reduced repetitive firing in neurons caused by slowing in the rate of recovery of channels due to enhanced inactivation of Na central nervous system (CNS) depressant, reduces seizure propagation, induces cerebellar-vestibular dysfunction; also weak antiarrythmic, inhibits insulin release.1–3 Contraindication: Hypersensitivity to medication; class C pregnancy1,3 Rx: Loading dose 15 to 20 mg/kg IV. Do not exceed 50 mg/minute IV. Usual 1 g load IV slow over 1 hour, then maintenance of 100 mg IV tid. Always check levels after 3 days. Phosphenytoin formulation can be given faster IV because it does not contain propylene glycol. Before infusion, it should be diluted in 5% dextrose in water or 0.9% NS to a concentration of 1.5 to 25.0 mg/mL (phenytoin equivalents; PE). To avoid hypotension, do not exceed 150 mg PE/minute. For seizure prophylaxis, loading dose is 16 to 18 mg/kg IV or intramuscularly (IM). Daily maintenance dose is 4 to 6 mg PE/kg/day IV or IM, divided into 2 or more doses.1–4 Side effects: Hypotension, hyperglycemia, arrhythmia, peripheral neuropathy, gingival hyperplasia, megaloblastic anemia (rare), hepatotoxicity (rare), Stevens-Johnson syndrome1 Action: Inhibitor of γ-aminobutyric acid (GABA) transaminase and glutamate decarboxylase1,3 Contraindication: Pregnancy1 Rx: 600 to 3000 mg/day; start at IV/PO 10 to 15 mg/kg/day. If dose >250 mg per day, it should be divided.1,4 Side effects: Gastrointestinal (GI) upset, pancreatitis, liver failure if <2 years of age, teratogenic, drowsiness, hyperammonia, hair loss, weight gain, tremor1 Action: Blocks voltage-dependent Na channel in neuronal cell membrane; hepatic metabolism. Before starting, check complete blood count (cbc), platelet count, and serum Fe. Do not start or stop if white blood (cell) count (WBC) < 4, hematocrit (HCT) < 32, platelet count (Plt) < 100, reticulocyte (Retic) < 3, Fe >150.1,3 Contraindication: Hepatic failure or insufficiency1 Side effects: Aplastic anemia, ataxia, drowsiness, transient diplopia, Stevens-Johnson syndrome, syndrome of inappropriate antidiuretic hormone (SIADH), hepatitis1 Action: Opens postsynaptic Cl ion channels, decreasing Na and Ca influx1,3 Contraindication: Multiple drug interactions1,3 Rx: IV/PO/IM loading 20 mg/kg/day; slow maintenance 30 to 250 mg/day divided bid/tid; therapeutic level 15 to 30 μg/mL1,3,4 Side effects: Cognitive impairment, paradoxical hyperactivity1,3 Action: Same as phenobarbital1,3 Contraindication: Multiple drug interactions1 Rx: Start 125 mg/day × 1 week; increase slowly to avoid sedation, 250 to 1500 mg/day, divide bid1 Side effects: Fewer side effects, more significant in seizure control; loss of libido1 Action: Antiseizure1 Contraindication: Hypersensitivity to succinimides; use with caution in pregnancy. Rx: Oral/nasogastric (NG) only 500 to 1500 mg/day. In children, start at 250 mg/day, titrate up to 500 mg/day divided bid.1 Side effects: Lethargy, hiccoughs, headache, Stevens-Johnson syndrome, systemic lupus erythematosus (SLE)–like syndrome, psychotic behavior1 Action: Benzodiazepine used short term in acute setting; not for long-term use.1,3 Contraindication: Long-term use1 Rx: Start IV/nasogastric [NG] at 1.5 mg/day, divided tid, increased by 0.5 mg q 3 days. Usual dosage range 1 to 12 mg/day; maximum 20 mg/day.1,4 Side effects: Ataxia, drowsiness behavior changes1 Contraindication: Hypersensitivity1 Rx: Start 300 mg PO/NG q HS (hold for loose stools); increase slowly over 3 days to 300 to 600 mg until therapeutic1 Side effects: Dizziness, ataxia, fatigue, nystagmus, viral infection1,3 Action: Inhibits release of glutamate and voltage-sensitive Na channels1,3 Contraindication: Hypersensitivity to pregnancy class C1 Rx: Start 50 mg PO qid × 2 weeks, then bid × 2 weeks1,4 Side effects: Headache, fatigue, nausea/vomiting, pancreatitis, peripheral neuropathy1 Contraindication: Hypersensitivity1 Rx: PO/NG 500 mg bid, titrate to effective maximum 3000 mg daily1 Side effects: Somnolence, weakness1 Action: Short-acting barbiturate, depressing cortical activity1,3 Contraindications: Hypersensitivity, hepatic impairment, dyspnea, porphyria, pregnancy1,3 Rx: For induction of coma: Loading dose of 10 mg/kg IV over 30 minutes, then 5 mg/kg q hour × 3 doses, then maintenance 1 mg/kg/hour titrating to 1–2 burst per page. For status epilepticus: IV start at 65 to 95 mg/minute, titrate up to 1400 mg total dose.1,2,4 Side effects: Bradycardia, hypotension, syncope, rash, exfoliative dermatitis, Stevens-Johnson syndrome1 Many animal models have demonstrated that corticosteroids stabilize cell membrane structures, stabilize the blood–spinal cord barrier reducing vasogenic edema, enhance blood flow in the spinal cord, inhibit endorphin release, prevent free radical accumulation, and moderate the inflammatory response. However, corticosteroids have many side effects and must be used with caution. These side effects include sepsis, pneumonia, death due to respiratory complications, and other complications. See Table 19–1. Action: Decreases inflammation by suppressing immune response, inhibiting polymorphonuclear (PMN) neutrophil leukocytes migration1–3 Contraindications: Hypersensitivity, active untreated infections1,3 Rx: Brain tumor protocol for cerebral edema: 10 to 20 mg loading dose, then 4 to 10 mg q 6. Minimal 10 day taper for weaning.2 Side effects: Cushing’s syndrome, hypersensitivity reactions, immuno-suppression, insomnia, agitation, vertigo, psychosis, delirium, pseudotumor cerebri, increased appetite1–3 Action: Decreases inflammation by suppressing immune response, inhibiting PMN migration1,3 Contraindications: Hypersensitivity, active untreated infections1 Rx: Spinal shock protocol: 30 mg/kg IV over 15 minutes, followed 45 minutes later by infusion of 5.4 mg/kg/hour × 23 hours1,2 Side effects: Cushing’s syndrome, hypersensitivity reactions, immuno-suppression, insomnia, agitation, vertigo, psychosis, delirium, pseudotumor cerebri, increased appetite1–3 Nonsteroidal anti-inflammatory drugs (NSAIDs) inhibit isoforms of the enzyme cyclooxygenase (COX 1-3) blocking prostaglandin synthesis. NSAIDs alone may be given for pain that is 4 or less. They should be with held back for 4 to 10 days after mild bleeding and not given at all with severe bleeding, and they should be given with a stomach protectant and adequate hydration to help prevent side effects. NSAIDs belong to multiple drug groups with each group affecting individual patients differently. Therefore, if one group of NSAIDs does not work consider treatment with another. When pain is 4 to 8, NSAIDs can be given with other pain-altering medications. See Table 19–2. Action: Enhances synaptic inhibition mediated by GABA1,3 Contraindications: Allergy to egg or soybean. Reduce doses for elderly, hypovolemic, or those with concomitant use of narcotics.1,3 Rx: Sedation: IV bolus 0.1 to 1.0 mg/kg, titrate slowly to the desired effect (onset of slurred speech); infusion 20 to 75 μg/kg/minute, monitoring respiratory/cardiac function continuously. Anesthetic induction: IV 2 to 4 mg/kg (give slowly over 30 seconds in 2–3 divided doses). Anesthetic maintenance: IV bolus 25 to 50 mg, then infuse at 100 to 200 μg/kg/minute. Antiemetic: 10 mg IV.1–3 May also be used for burst suppression but ability to provide neuronal protection is controversial. Side effects: Hypotension from myocardial depression, decreases systemic vascular resistance (SVR). Depresses laryngeal reflexes more than barbiturates or etomidate. Pain on injection into small veins, histamine release with rapid injection, anaphylaxis.1,3 Action: Binds to GABA receptors containing gamma subunits, half-life 1.5 to 3 hours1,3 Contraindications: Hypersensitivity, narrow-angle glaucoma, pregnancy1 Rx: Conscious sedation: Slow IVP 1 to 2 mg over 2 minutes (do not exceed 2.5 mg with initial dose), wait 2 to 3 minutes, repeat up to total of 0.1 to 0.15 mg/kg. IM preop: 0.07 to 0.08 mg/kg (5 mg/70 kg) ~1 hour preop. Induction general anesthesia: Initial dose slow IVP. For unpremedicated average adult age <55 years: 0.25 mg/kg; for >55 years, American Society of Anesthesiologists (ASA) class I or II 0.2 mg/kg; for ASA class III or IV, 0.15 mg/kg. To maintain, repeat 25% initial dose.1,3 May also be used for burst suppression but ability to provide neuronal protection is controversial. Side effects: Decreased tidal volume/respiratory rate, hypotension, drowsiness, oversedation, nausea and vomiting1 Action: A benzodiazepine with antianxiety, sedative, and anticonvulsant effects which interacts with the γ-aminobutyric acid (GABA)-benzodiazepine receptor complex. Contraindications: Hypersensitivity to benzodiazepines or their vehicles (polythylene glycol, propylene glycol, and benzyl alcohol). It should not be used in patients with acute narrow-angle glaucoma, or in non-intubated patients with sleep apnea syndrome or severe respiratory insufficiency. The use of Ativan injection intra-arterially is contraindicated because, as with other injectable benzodiazepines, inadvertent intra-arterial injection may produce arteriospasm resulting in gangrene, which may require amputation. Rx: Mild sedation: IV 0.5 to 2 mg (0.044 mg/kg). Conscious sedation: up to a total of 4 mg (0.05 mg/kg). Can also be used IM reaching peak concentration in 3 hours. Orally 0.5 to 1 mg 2 to 3 times per day. Can also be used for burst suppression but ability to provide neuronal protection is controversial. As with benzodiazepines, its action can be reversed with flumazenil (Romazicon) but resedation may occur. Flumazenil action begins less than 2 minutes after administration and peaks in 6 to 10 minutes. The initial dosage is 0.2 mg IV repeated at 1 minute intervals to a maximum of 1mg. Side effects: Respiratory depression, fetal damage. Action: Fast acting barbiturate with 3 to 4 hour duration of action. Contraindications: Hypersensitivity, status asthmaticus, severe cardiovascular disease, porphyria. Rx: Load intravenous 10 mg/hour. Give as 2.5 mg/kg/hour slowly every 15 minutes for 4 doses. Hold if blood pressure drops inappropriately. Then continue at 10 mg/kg/hour for 3 additional hours. Next continue maintenance dose at 1 to 3 mg/kg/hour. Titrate for 1 to 2 burst per page. If the loading dose achieves burst suppression then continue at maintenance dose. Watch for inadequate blood pressure/cerebral perfusion pressure. If using to salvage brain function, ICP should decrease within the hour after burst suppression has occurred. Check daily complete blood count (cbc) and blood cultures to monitor for infection and sepsis. Check pentobarbital level 1 hour after completing loading dose and daily thereafter. May also be used for burst suppression but ability to provide neuronal protection is controversial. Side effects: Hypotension, inability to rapidly diagnose infection Action: Blocks postsynaptic D1 and D2 receptors in the brain; depresses reticular activating system; depresses hypothalamic hormones1,3 Contraindications: Hypersensitivity, Parkinson’s disease, severe cardiac or hepatic disease, bone marrow suppression, coma1 Rx: Sedation: IV/IM/IVPB (intravenous piggyback); may repeat bolus doses after 30 minutes until calm achieved, then administer 50% of the maximum dose every 6 hours. Agitation: mild 0.5 to 2.0 mg; moderate 2.5 to 5.0 mg; severe 10 to 20 mg.1 Side effects: Hypotenstion/hypertension, anxiety, extrapyramidal and dystonic reactions, pseudoparkinsonian reactions, tardive dyskinesia, neuromalignant syndrome, akathisia1 Action: Short-acting barbiturate1,3 Contraindications: Hypersensitivity, status asthmaticus, severe cardiovascular disease, porphyria1,3 Rx: Adults: Initial concentration should not exceed 2.5%. Give 50 mg test dose moderately rapid IVP; if tolerated, give 100 to 200 mg IVP over 20 to 30 seconds (500 mg may be required in large patient).1,3,4 May also be used for burst suppression but ability to provide neuronal protection is controversial. Side effects: Dose-related respiratory depression, myocardial depression, hypotension in hypovolemic patients, irritation if extravassated, intraarterial injection—necrosis, agitation if injected slowly1 Action: Potentiates GABA and depresses reticular activating system1,3 Contraindication: Hypersensitivity Rx: IV induction: 0.1 to 0.6 mg/kg. Infusion: 0.25 to 1.00 mg/minute (5 to 20 mg/kg/minute). Continuous infusion not recommended. Rectal: In children 6 months to 6 years old, 6.5 mg/kg produces reliable hypnosis in 4 minutes but maintains a rapid recovery without any untoward effects.1 May also be used for burst suppression but ability to provide neuronal protection is controversial. Side effects: Pain on injection into small veins, high incidence of thrombophlebitis (24% compared with thiopental 4%), myoclonus. Lowers seizure threshold, nausea and vomiting, adrenocortical suppression.1 Action: Direct effect on the cortex and limbic system, producing cataleptic-like state, dissociated from surroundings1 Contraindications: Increased ICP, hypertension, hypersensitivity, aneurysms, thyrotoxicosis, CHF, angina1,3 Rx: 1 to 2 mg/kg IV over 1 to 2 minutes or 4 mg/kg IM induces 10 to 20 minute dissociative state.1 May also be used for burst suppression but ability to provide neuronal protection is controversial. Side effects: Concurrent atropine minimizes hypersalivation; hallucinations, vivid dreams, hemodynamic instability1 Most neurosurgical intensive care unit (NICU) patients are immobilized for one reason or another. Deep venous thrombosis (DVT) prophylaxis should be implemented as soon as possible. Always begin with sequential compression devices and thigh-high compression stockings. Patients who will be long-term immobilized should be considered for anticoagulation drugs. Depending on the pathology, patients with traumatic intracranial hemorrhage (ICH) with no sequelae 72 hours posthemorrhage may be started on anticoagulation drugs.2 Action: Prevents the conversion of fibrinogen to fibrin1,3 Contraindications: Hypersensitivity, severe thrombocytopenia, uncontrolled bleeding1 Rx: 5000 units subcutaneous (SQ) tid1,3,4 Side effects: Bleeding, vasospasm, thrombocytopenia, bruising1,3 Action: Prevents the conversion of fibrinogen to fibrin1,3 Contraindications: Hypersensitivity to pork products, uncontrolled bleeding1 Rx: Prevention: 40 SQ qid. Treatment, DVT or PE: 1 mg/kg bid1,3,4 Side effects: Bleeding, fever, bruising1,3 The most commonly prescribed medications for severe pain are opioids, which stimulate mu, kappa, delta and nociceptin/orphanin FG (N/OFQ) receptor. The first and most widely used opioids are the group that stimulates the mu receptor; these include morphine, demerol, dilaudid, and fentanyl. Clinically, the effect of opioids is to raise the pain threshold, increasing the minimal intensity needed to feel pain. At the anatomic level, opioids act by inhibiting nociceptive transmission to the spinal cord, activating descending inhibitory pathways, and altering higher center activity of pain perception. Just as NSAIDs belong to different groups with considerable variability in efficacy, opioid groups vary in ability to treat pain, even in the same individual. Action: Topical analgesic1 Contraindications: Hypersensitivity, broken skin barrier; but still can place adjacent to incision1 Rx: Place 1 to 3 patches 12 hours per day (12 hours on, 12 hours off); when using on fresh surgical incision, apply both sides but not over.1 Side effects: Local edema, erythema, urticaria, anaphylaxis1,3 Action: Suspected to be cyclooxygenase-3 (COX-3) inhibitor at very high doses1,3 Contraindications: Hypersensitivity, chronic alcohol abuse, impaired liver function1,3 Rx: Adults: 650 to 1000 mg PO/PR (far point of accommodation) q 4 to 6 hours, not to exceed 4000 mg/day; children: 10 to 15 mg/kg PO/PR q 4 to 6 hours1,3,4 Side effects: Hepatic toxicity1,3 See Table 19–3. Action: Inhibits prostaglandin synthesis; only parenteral nonsteroidal anti-inflammatory drug (NSAID) approved for use in pain control in the United States1,3 Contraindication: Hypersensitivity to NSAIDs, active peptic ulcer disease, recent GI perforation, renal impairment, bleeding. Do not use prophylactically before major surgery.1,3 Rx: 10 mg PO q 4 to 6 hours; IM/IV 30 to 60 mg q 6 to 8 hours, use only continuously for 72 hours. Acute pain after surgery when bleeding is controlled: 120 mg in 500 cc normal saline to run at 10 cc/hour until completed over 50 hours. Must have initial loading dose of 30 to 60 mg IV. Stomach protectants must be given.1,3 Side effects: Bleeding time prolonged by platelet function inhibition, gastric mucosal irritation, and erosion, even though given in IV or IM form. Side effects are worse in the elderly and with prolonged use.1,3 Action: Kappa agonist, mu antagonist1,3 Contraindications: Hypersensitivity, head injury, impaired pulmonary or liver function, pregnancy, elderly patients1 Rx: IV 0.15 to 2.5 mg/kg q 3 to 6 hours Side effects: Respiratory depression, severe bradycardia, severe hypotension, sedation, headache, dysphoria1,3 Action: Kappa agonist, mu agonist and antagonist1,3 Contraindications: Hypersensitivity; substance abuse; impaired liver, renal, and pulmonary function. Use caution in head-injured patients and CNS depression.1,3 Rx: IV 2 mg, IM 0.5 to 4.0 mg q 3 to 4 hours, 0.25 to 32.0 mg/day maximum; intranasal (IN) 1 mg spray q 3 to 6 hours1 Side effects: Respiratory depression, substance abuse, severe hypotension, severe bradycardia, sedation, nausea/vomiting1,3 Action: Affects mu opioid receptors1,3 Contraindications: Hypersensitivity, ethanol intoxication, substance abuse history. Use caution with head-injured patients, those with CNS infections or lesions, and patients with elevated ICP.1–3 Rx: 50 to 100 mg PO q 4 to 6 hours prn1 Side effects: Hypoventilation, constipation, bradycardia. Large dose given rapidly may cause chest wall rigidity, dysconjugate gaze, headaches.1,3 Action: Weak opioid1 Contraindications: Hypersensitivity, respiratory depression, paralytic ileus. Use caution in patients with elevated ICP, seizure disorder, or head injury.1 Rx: Adults: 30 to 60 mg IM/PO q 3 hours; children: 0.5 to 1 mg/kg/dose q 4 to 6 hours1 Side effects: Respiratory depression, CNS depression, hypotension, bradycardia, syncope, cardiac arrest, elevated ICP, seizures, paralytic ileus, dependency, shock, anaphylactoid reactions. More common side effects include dizziness, nausea and vomiting, sedation, and constipation.1 Contraindications: Hypersensitivity, respiratory depression, paralytic ileus, CNS depression, head injury, elevated ICP, seizure disorder1,3 Rx: Available in 5.0, 7.5, and 10.0 mg doses with acetaminophen dose, 1 or 2 tablets PO q 4 to 6 hours; not to exceed 60 mg hydrocodone in 24 hours, not to exceed 4000 mg acetaminophen per 24 hours1,3 Side effects: CNS depression, respiratory depression, dependency, paralytic ileus, increased ICP, hypotension, nausea and vomiting, sedation1,3 Action: Binds to mu opiate receptor in the CNS, inhibits pain pathway. Opiate potency 100 × morphine. In small doses, lasts 20 to 30 minutes. Supplied in concentration 50 μg/mL. Increases CBF.1,3 Contraindications: Hypersensitivity, increased ICP, respiratory depression, pregnancy1,3 Rx: 25 to 100 μg (0.5–2.0 mL) IVP, repeat prn. Also available as transdermal patch, which is changed every 72 hours, delivering 25, 50, 75, or 100 μg/hour.1 Side effects: Hypoventilation, constipation, bradycardia. Large dose given rapidly may cause chest wall rigidity, dysconjugate gaze.1 Action: Binds to mu opiate receptor in the CNS; inhibits pain pathway, increases CBF1,3 Contraindications: Hypersensitivity, increased ICP, respiratory depression1,3 Rx: Drip: mix 100 mg/100 mL NS, start 2 mg q hour, titrate to effect maximum 10 mg q hour. IVP: start 2 mg q 1 to 2 hours, increase prn.1–4 Side effects: Respiratory depression, miosis, hypotension, bradycardia, apnea, pulmonary edema, dysconjugate gaze1,3 Nausea and vomiting are frequent problems for patients in the NICU due to stimulation of the chemoreceptor trigger zone (CRTZ). Phenothiazine derivatives, such as Phenergan, should be avoided in general, due to a lowering of the seizure threshold.2 Action: Selective 5-hydroxytryptamine (5HT)-receptor antagonist; blocks serotonin on vagus nerve terminals and in the CRTZ1,3 Contraindication: Hypersensitivity to ondansetron1 Rx: 4 to 8 mg IV q 6 to 8 hours prn nausea/vomiting1,2 Side effects: Malaise, fatigue, headache1 Action: Selective 5-HT-receptor antagonist. Blocks serotonin both peripherally and centrally at CRTZ.1,3 Contraindication: Hypersensitivity to granisetron1 Rx: 1 mg PO q 12 hours or 2 mg PO q 24 hours1 Side effects: Headache, constipation, dizziness, insomnia, anxiety1,3 Contraindications: Hypersensitivity to trimethobenzamide or benzocaine. Injection contraindicated in children.1,3 Rx: 250 to 300 mg PO tid/qid, 200 mg IM/PR tid/qid1 Side effects: Hypotension, depression, coma, disorientation, jaundice, muscle cramps, blurred vision1,3 Action: Competitively inhibits benzodiazepine at receptor sites1,3 Contraindications: Pregnancy, patients chronically treated with benzodiazepines where antagonism may provoke a withdrawal syndrome and/or seizures. May provoke a panic attack.1 Rx: 0.2 mg IV q minute × 1 to 5 doses; maximum dose 1 mg, 3 mg/hour1 Side effects: Seizures—high risk in patients on benzodiazapines for long-term sedation, hypoventilation, arrhythmias, and resedation1,3 Action: Oxymorphone derivative, competitively binds to opioid receptors, half-life (t½) ~4 to 60 minutes1,3 Contraindication: Hypersensitivity; may cause acute withdrawal from opioids in individuals who are physically dependent. Rx: Load: 1 to 4 μg/kg, infuse at rate of 5 to 15 μg/kg/hour. Titrate IV in small doses 20 to 40 μg.1,4 Side effects: Severe unmasked pain can lead to sympathetic and cardiovascular stimulation: hypertension, dysrhythmias, pulmonary edema, and cardiac arrest.1,3 Action: Oxymorphone derivative, competitively binds to opioid receptors, t½ > 10 hours1 Contraindication: See naloxone. Rx: Oral: 100 mg or greater1,3 Side effects: See naloxone
Care of the Patient
19
Neuropharmacology
 Hemodynamic Agents
Hemodynamic Agents
Hypertension
Sodium Nitroprusside (Nipride)
Nitroglycerin (Tridil)
Labetalol (Normondyne)
Hydralazine (Apresoline)
Esmolol (Brevibloc)
Diltiazem (Cardizem)
Nifedipine (Procardia)
Nicardipine (Cardene)
Angiotensin II Receptor Blockers
Enalaprilat (Vasotec)
Clonidine (Catapres)
Hypotension
Dopamine (Inotropin)
Dobutamine (Dobutrex)
Norepinephrine (Levophed)
Phenylephrine (Neosynephrine)
Inamrinone (Inocor)
Epinephrine (Adrenaline)
Isoproterenol (Isuprel)
 Electrolytes/Intravenous Fluids
Electrolytes/Intravenous Fluids
Sodium and Intravenous Fluids
Phosphorus
Calcium
Magnesium
Potassium
 Blood Products
Blood Products
Packed Red Blood Cells
Fresh frozen plasma
Platelets
Cryoprecipitate
 Antiepileptic Medications
Antiepileptic Medications
Phenytoin (Dilantin)
Valproic Acid (Depakene)
Carbamazepine (Tegretol)
Phenobarbital (Luminal)
Primidone (Mysoline)
Ethosuximide (Zarontin)
Clonazepam (Klonipin)
Gabapentin (Neurontin)
Lamotrigine (Lamictal)
Levetiracetam (Keppra)
Pentobarbital (Nembutal)
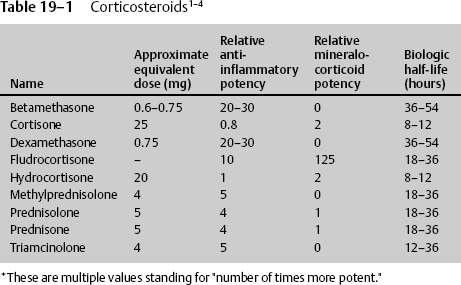
 Corticocosteroids
Corticocosteroids
Dexamethasone (Decadron)
Methylprednisolone (Solu-medrol)
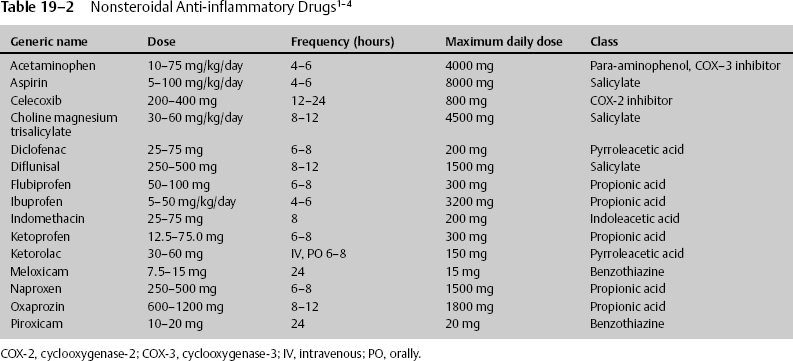
 Nonsteroidal Anti-inflammatory Drugs
Nonsteroidal Anti-inflammatory Drugs
 Sedatives
Sedatives
Propofol
Midazolam (Versed)
Lorazepam (Ativan)
Pentobarbital (Nembutal)
Haldol
Thiopental (Pentothal)
Etomidate
Ketamine
 Anticoagulants
Anticoagulants
Heparin
Lovenox
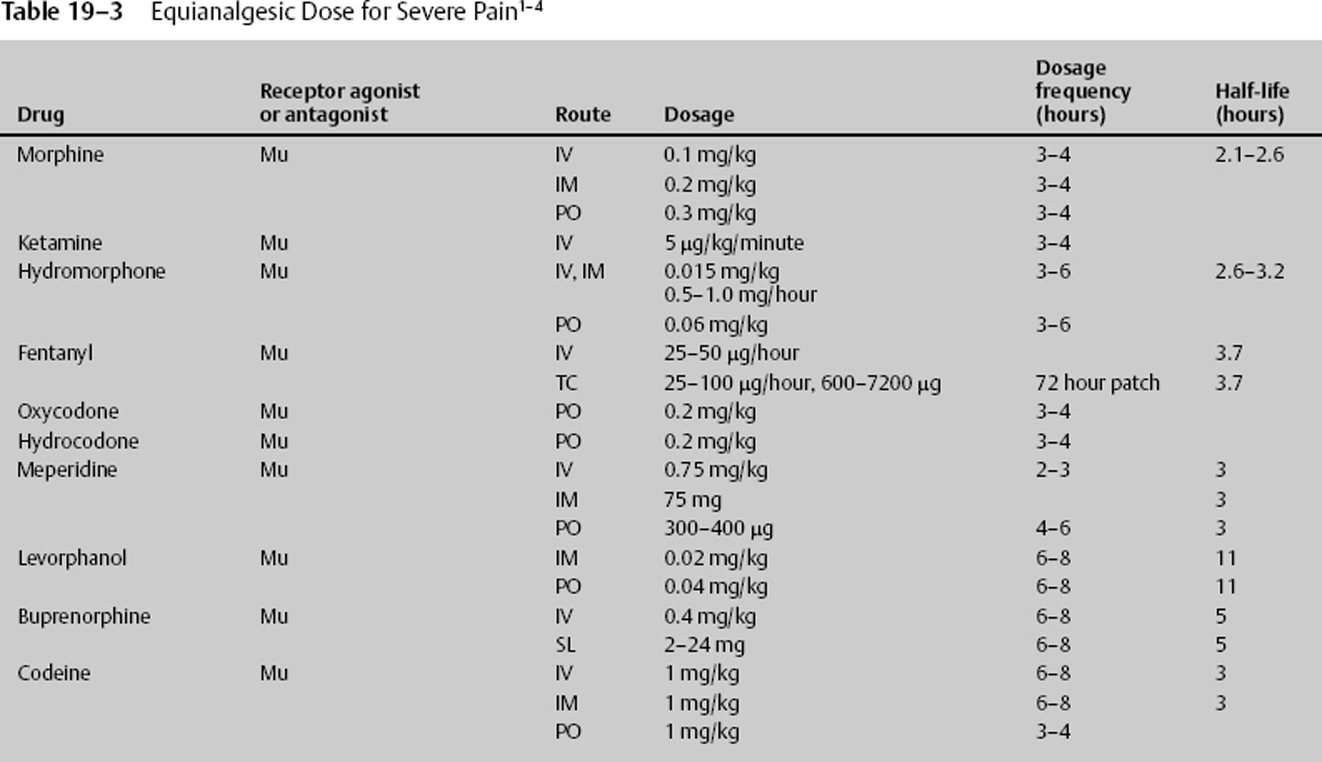
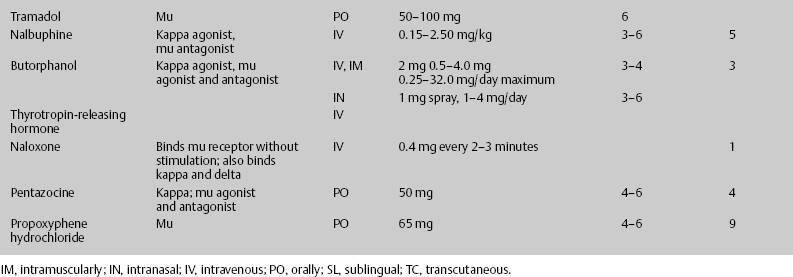
 Pain Medications
Pain Medications
Lidocaine Patch (Lidoderm 5%)
Acetaminophen (Tylenol)
Equianalgesic Doses for Severe Pain
Ketorolac (Toradol)
Nalbuphine (Nubain)
Butorphanol (Stadol)
Tramadol (Ultram)
Codeine
Hydrocodone
Fentanyl
Morphine
 Antiemetics
Antiemetics
Ondansetron (Zofran)
Granisetron (Kytril)
Trimethobenzamide (Tigan)
 Reversal Agents
Reversal Agents
Flumazenil
Naloxone
Naltrexone
< div class='tao-gold-member'>
Neuropharmacology
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree