Neuropathic pain
Prevalence
Neuropathic pain is estimated to affect about 1.5-3% of people worldwide1,2. The incidence of neuropathic pain varies among different pain syndrome categories (6.1)3. Diabetes mellitus is the most common medical condition resulting in neuropathy. Polyneuropathy occurs in one of every 4-5 patients with diabetes4,5. Painful neuropathy more commonly occurs in diabetics with long-duration illness and older age.
Painful neuropathies constitute a diverse collection of individual disorders, including conditions associated with direct nerve compression or trauma, such as mononeuropathy, radiculopathy, deafferentation pain, and reflex sympathetic dystrophy, and neuropathies related to other medical illnesses, such as peripheral polyneuropathy (Table 6.1). Several common unique neuropathic pain conditions are postherpetic neuralgia (PHN), trigeminal neuralgia, and complex regional pain syndrome (CRPS).
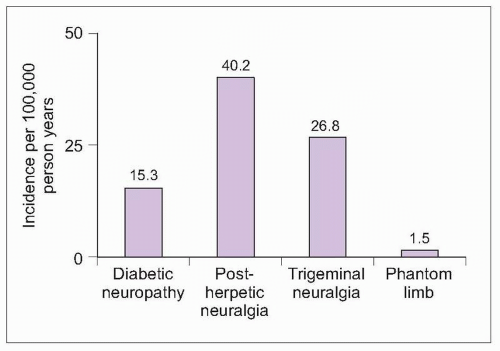 6.1 Incidence of painful neuropathies. A survey of 686 primary care practices in the United Kingdom identified the incidence of common painful neuropathies. (Based on Hall GC, et al., 20063.) |
Table 6.1 Diverse neuropathic pain syndromes | ||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Postherpetic neuralgia
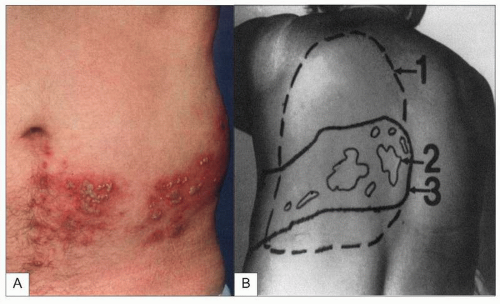
Herpes zoster characteristically begins with dermatomal pain or sensory disturbance, followed within hours to days by a painful papular rash in a dermatomal distribution (6.2). Papules change to vesicles and then become crusted. The acute zoster rash typically heals within 3-4 weeks. PHN is defined as pain that persists for >1 month after the onset of herpes zoster.
PHN occurs in about 30% of patients following acute zoster, and lasts 1 year in about 10% (6.3)6. The prevalence of PHN by dermatomal region and likelihood of improvement by region are shown in 6.47. PHN most commonly affects the trunk or face. Among patients with trigeminal distribution PHN, the ophthalmic division is usually affected. Risk factors for the development of PHN include female gender, older age, experiencing pain or sensory disturbance before the development of the rash, greater pain severity during acute herpes zoster, and larger distribution for zoster rash8. Persistent PHN increases in patients with older age and greater pain severity.
Case presentation
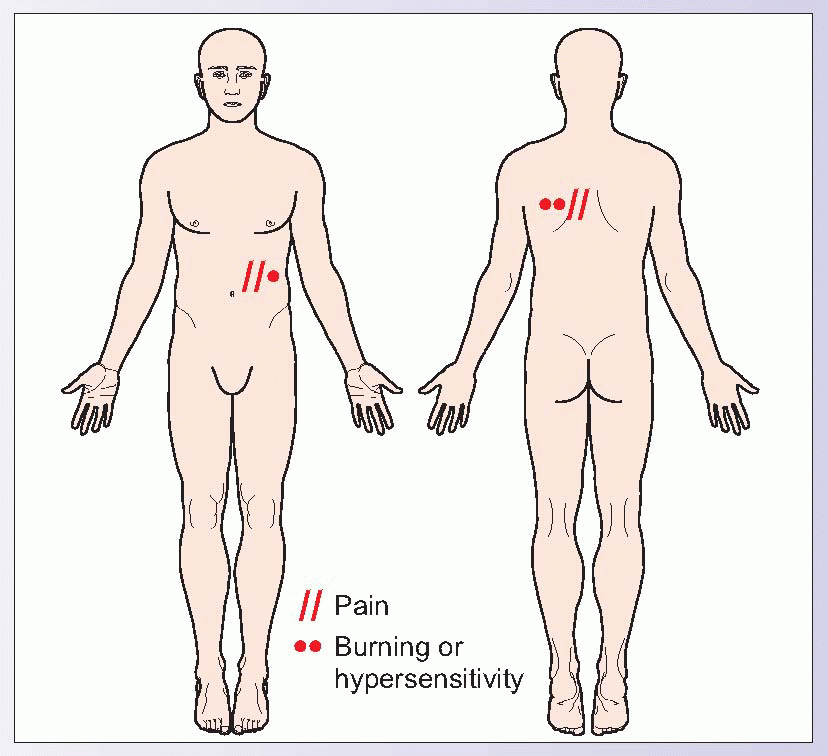
A previously active 75-year-old woman reports feeling depressed and hopeless due to pain over her left chest. Four months ago, she developed a small band of itchiness around her left chest under her breast. After a couple of days, she noticed small blisters that quickly crusted over, which she assumed was a heat rash. This was followed by a searing, unbearable pain in this same area that has persisted. Her pain drawing is shown. She reports, “I feel silly complaining about a little pain when my health is so good, but I can’t stand it anymore. If anyone touches my back or chest, I just want to scream.”
This case of PHN was effectively treated with a low-dose antidepressant and a 5% lidocaine patch, which reduced her pain and provided protection from inadvertent touch over the painful area. Despite the often small area involved in PHN, the pain is frequently intolerable and is the leading cause of suicide in elderly patients with chronic pain.
|
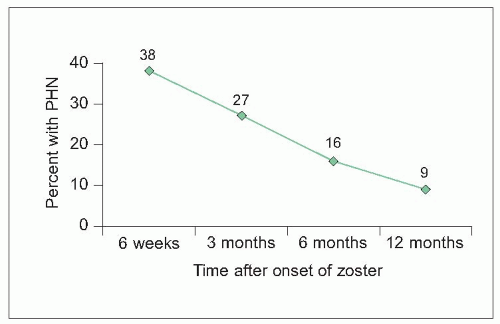 6.3 Prevalence of PHN in patients with herpes zoster. A total of 204 primary care patients with acute shingles of ≤7 days with the diagnosis confirmed by laboratory testing were followed for up to 1 year in a prospective, observational study. Optimal antiviral therapy was started within 72 hours of symptom onset in 54% of patients, and delayed until after 72 hours in 25% of patients, usually due to delayed presentation to the family doctor. Antiviral therapy was predominantly with acyclovir (91% of treated patients). Patients >50 years old and those with moderate-severe pain at presentation were significantly more likely to develop PHN. (Based on Scott FT, et al., 20036.) |
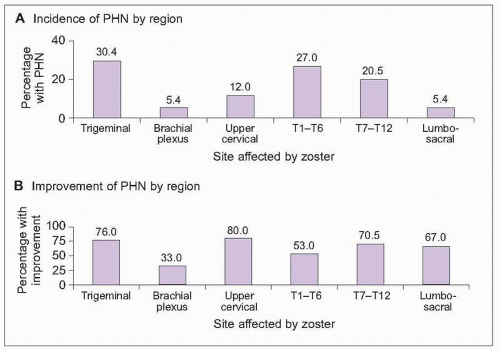 6.4 Epidemiology of PHN after herpes zoster. Pain features were retrospectively reviewed in 191 consecutive PHN patients, with a mean age of 68 ± 11 years. PHN most typically affected trigeminal and thoracic dermatomes (A), with pain right-sided in 52% of patients. Improvement by 75% or better (B) depended on pain location, with the best outcome for patients with pain in the face (especially the jaw), neck, and trunk. (Based on Bowsher D, 19967.) |
Case presentation
A 37-year-old homemaker presented with severe pain in her lower jaw and teeth. She was referred by her dentist due to persistent pain despite repair of dental caries. She comes to the office holding her face and limiting verbal responses. With each verbal response, she winces in pain, reporting jolts of pain with talking, brushing her teeth, or touching the jaw. Her only previous medical complaints were two remote episodes of arm and hand numbness that resolved over several weeks and an episode of vertigo. Her examination is limited due to her refusal to permit full examination of the face and jaw. She does endorse a small area of numbness over her jaw and chin and has positive Babinski’s.
Although her current pain complaint was typical of trigeminal neuralgia, this patient’s relatively young age, history of neurological episodes, and abnormal neurological examination warrant further evaluation. An imaging study of the brain revealed white matter abnormalities consistent with multiple sclerosis.
Trigeminal neuralgia
Trigeminal neuralgia is experienced as a unilateral, intermittent, electric-shock-like jolt of pain into one or more of the divisions of the trigeminal nerve, usually over the cheek or jaw (6.5). Interestingly, pain more commonly affects the right side of the face9,10. Pain is typically triggered by activating a discrete trigger point on the face, such as with touching, shaving, talking, or chewing, often limiting the patient’s cooperation with a careful examination of the face and mouth. Curiously, patients with trigeminal neuralgia, as in the case presentation, will often sit holding the painful side of the face, possibly to prevent stimuli from activating their trigger point. In between pain episodes, some people experience a residual low level of pain over the face or jaw. Trigeminal neuralgia generally affects adults after age 40. Younger patients and patients with bilateral symptoms should be evaluated for multiple sclerosis. Although sensory loss occurs in a minority of patients with idiopathic trigeminal neuralgia, identifying sensory loss warrants evaluation with neuroimaging studies.
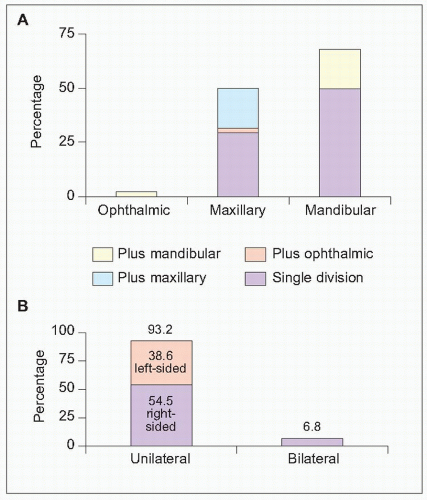 6.5 Location of trigeminal neuralgia pain. A: Nerve division affected; B: side of face affected. Pain distribution was evaluated in 44 patients treated at university settings in Singapore and Malaysia. There were no cases of trigeminal neuralgia pain affecting the ophthalmic division alone (A). Ophthamic plus maxillary pain occurred in one patient (2.3%). Most patients had mandibular pain (68.2%), with pain limited to the mandibular distribution for 50% of trigeminal neuralgia patients. Pain affected the maxillary division alone for 29.5% of patients and maxillary plus mandibular regions for 18.2%. Most patients had unilateral pain, more often affecting the right side of the face (B). (Based on Loh HS, et al., 19989.) |
Table 6.2 Epidemiology of CRPS | ||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||
Complex regional pain syndrome
CRPS is a neuropathic pain that develops following limb injury or a period of limb immobilization (e.g. casting). CRPS may be divided into Type I (occurring in the absence of a nerve injury; formerly called reflex sympathetic dystrophy) and Type II (occurring after injury to a specific large nerve; formerly called causalgia). CRPS is characterized by excessive splinting and guarding of the painful extremity. Sympathetically-maintained pain and sympathetically-mediated pain are also terms formerly used to describe this syndrome. Failure of relief from sympathetic blocks, particularly in patients with long-standing complaints, led to the discontinuation of these terms.
The incidence of CRPS differs between the United States and Europe, although other epidemiological features are similar (Table 6.2)11,12. In the United States sample, symptoms resolved in 74% of cases, with a mean symptom duration of 1 year and a range of 1-60 months. Most patients rated treatment effectiveness good for physical therapy (87%), sympathetic blocks (79%), and prescription medication (80%).
Case presentation
A 45-year-old woman arrived at the clinic on a hot summer day with a wool shawl draped across her shoulders and right arm. She held her arm in a flexed position, splinted to her body. The nails on her left hand were clipped close, while those on the right were long and abnormally angled. She reported severe pain in the right upper extremity for the last 8 months, following removal of a cast for a seemingly uncomplicated wrist fracture after a skating accident. She claimed to wear the shawl because her arm was always cold and sometimes sweaty. She also reported being unable to clip her nails due to their abnormal shape and pain while attempting to cut them. She had already seen three other doctors, each of whom referred her to psychiatry with a diagnosis of malingering or conversion disorder. Another doctor refused to see her because he assumed she was planning litigation from the skating accident and fracture repair. Her pain drawing is shown.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree