Introduction
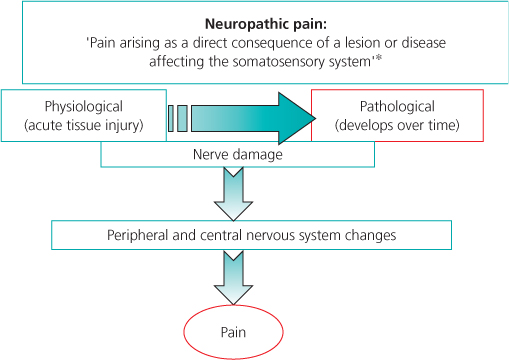
Neuropathic pain can be initiated by, or is secondary to, an abnormality in normal sensory processing in the central or peripheral nervous system. It can be acute, for example, immediately following surgery, or may persist and become chronic (Figure 6.1). The neuropathic pain of some patients may be idiopathic in origin and, conversely, patients with clear evidence of lesions in the nervous system may have no pain at all.
Figure 6.1 Neuropathic pain may occur as a result of changes within the peripheral or central nervous system. *Treede, R-D, Jensen, TS, Campbell, JN, Cruccu, G, Dostrovsky, JO, Griffin, JW, et al. (2008) Neuropathic pain. Redefinition and a grading system for clinical and research purposes. Neurology, 70, 1630–1635.
Epidemiology
The exact prevalence of neuropathic pain is difficult to determine, with figures varying from 3–18% depending on the population being studied and how neuropathic pain is diagnosed (Chapter 1; Table 6.1). Neuropathic pain has been shown independently to be associated with older-age, women, unemployment and lower educational attainment. Persistent pain after surgery may continue for months or even years, with some evidence that if it is present six months after surgery, then it is likely to remain.
Table 6.1 Prevalence of neuropathic pain in the community
| Neuropathic pain disorder | Incidence per 100,000 |
| Post-surgical pain | 2000–70,000 |
| Post-stroke (central) pain | 2000–6000 |
| Post-herpetic neuralgia (PHN) | 40 |
| Trigeminal neuralgia (TGN) | 27 |
| Complex regional pain syndrome (CRPS) type 1 | 26 |
| Painful diabetic neuropathy (PDN) | 15 |
| Post-amputation pain, e.g. phantom limb pain | 1 |
An awareness of when neuropathic pain may occur, a high index of suspicion when pain responds poorly to standard analgesics and asking about the characteristics of the pain may aid in identifying neuropathic pain.
Mechanisms of Neuropathic Pain
This is covered more fully in Chapter 2, but some of the key features are summarised in Box 6.1.
Peripheral Mechanisms
- Reduced threshold required to activate nociceptors
- Spontaneous activity in primary sensory neurons, in the absence of any peripheral stimulus
- Altered neurotransmitter production in the dorsal root ganglia
Central Mechanisms
- Increased sensitivity or ‘wind-up’ in the spinal cord (n-methyl-d-aspartate (NMDA) receptor important role)
- Increased spontaneous background activity (balance of inhibition to excitation altered)
- Increased activity within the brainstem
- ‘Central sensitisation’
Aetiology
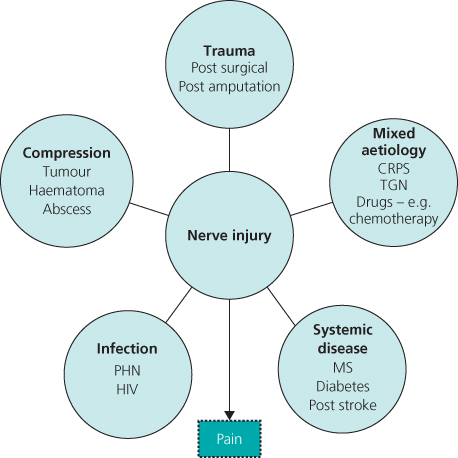
There are many possible causes of neuropathic pain, ranging from anything causing neural compression through to specific infection with varicella zoster, as occurs in post-herpetic neuralgia (Figure 6.2). This wide range of potential aetiologies reflects the fact that neuropathic pain is not a single disease, but a spectrum of disorders that presents with specific signs and symptoms which need to be elicited in order to make a correct diagnosis.
Figure 6.2 Causes of neuropathic pain. CRPS = Complex Regional Pain Syndrome; TGN = Trigeminal Neuralga; PHN = Post-Herpetic Neuralgia; HIV = Human Immunodeficiency Virus.
Diagnosis
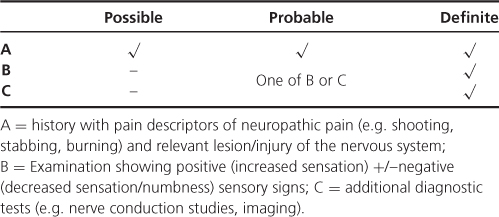
Doctors can find making the diagnosis of neuropathic pain challenging. There is no standard diagnostic procedure or test, with diagnosis based predominantly on an accurate history and examination. Recent guidelines on the diagnosis of neuropathic pain have attempted to classify it more specifically than previously (Table 6.2).
Table 6.2 Diagnosis of neuropathic pain
Screening Tools
Many studies have used screening tools to identify pain with neuropathic features. These do have some role in the non-specialist setting to highlight the possibility of a neuropathic type pain, but may miss 10–20% of cases. All the screening tools use a variable number of descriptors about the nature and site of the pain +/−clinical examination to define the likelihood of neuropathic pain (Table 6.3).
Table 6.3 Screening tools for neuropathic pain
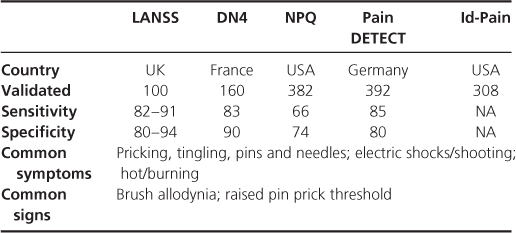
These screening tools include the LANSS (Leeds Assessment of Neuropathic Symptoms and Signs) or the painDETECT questionnaire, with a simplified version of the LANSS (the s-LANSS) being designed for self-completion by patients. The s-LANSS has also been validated for use in postal surveys (Box 6.2).
- Draw on a diagram where you feel your pain
- Any pins and needles?
- Any change in skin colour of painful area?
- Is skin abnormally sensitive to touch?
- Does your pain come in bursts?
- Any burning pain?
- How does rubbing the area feel?
- How does pressing the area feel?
Features of Neuropathic Pain
Patients with neuropathic pain may complain of a wide range of sensory disturbance, with both increased and decreased sensation potentially occurring in the affected area. Some of the characteristics of neuropathic pain are outlined in Box 6.3.
Spontaneous Pain
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








