Key Clinical Questions
Introduction
This chapter will present the thought processes behind general guiding principles for neurologic imaging. This chapter does not provide an exhaustive array of images because the goal is not to train hospitalists to interpret medical images but rather to provide a framework so that they can more effectively communicate with radiologists and order the most appropriate imaging modality to optimize timely evaluation and treatment. It will always be the responsibility of practitioners to provide radiologists with relevant clinical information so that recommendations regarding specific imaging and the actual interpretation are made in the context of the patient. A number of cases will be presented that highlight the limitations of imaging when this process does not occur.
Any patient with new neurologic symptoms and signs requires prompt imaging and appropriate specialty consultation to avoid catastrophic effects upon patient outcome. This is particularly true for processes that profoundly affect the homeostasis of anatomy and physiology with or without preexisting abnormality. Therefore, this chapter will review the characteristic findings to be expected for key “do-not-miss” diagnoses that would require the practitioner to contact the appropriate specialty services for emergent consultation and/or initiate steps for transfer to a tertiary care facility.
Corelation of Neurological Examination with Imaging
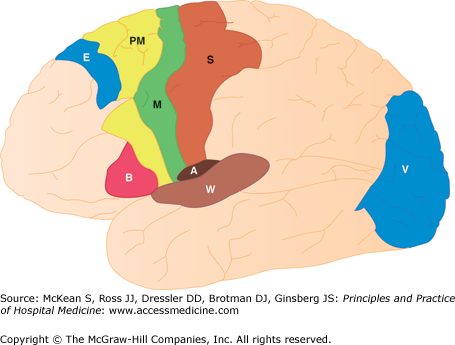
Correlation of the neurological examination with any imaging study obtained is of paramount importance. Anatomic references may help clinicians localize abnormalities. When subtle, as at the onset of a stroke syndrome, the conviction that a potential finding is in the precise location indicated by the focal neurological deficit can make the difference between the radiologist overlooking the possibility and confidently confirming the abnormality. In turn, this approach leads to decreased imaging during the acute illness. The workup of incidental findings can also then be deferred for outpatient workup when the imaging study will often be of higher quality due to the greater ability of the recuperated patient to understand and cooperate for the imaging study.
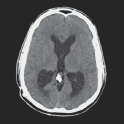
Several drawings accompany this text to refresh memory of neuroanatomy. It can be invaluable to consult an interactive Internet atlas, especially when immediate radiologic consultation is not available, and particularly in situations in which the patient condition evolves during the hospitalization. The clarity of anatomy is greater on MRI than CT so it may prove most helpful to use an MRI reference atlas, even for looking at the more commonly obtained in the acute care setting CT scan (Figure 111-1).
Selection of Imaging Modality
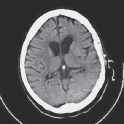
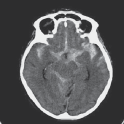
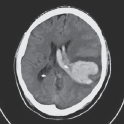
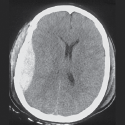
Neurologic imaging requires considerations of anatomy and function and an appreciation for the limitations of each imaging modality. CT has the highest spatial resolution; however, the superior tissue characterization of MRI allows the most exquisite demonstration of neuroanatomy in a physiologically relevant manner. CT images lesions by the degree of hyperdensity in the following decreasing order of density: bone (the highest density); clotted blood; liquid blood; subacute or approximately two weeks of blood similar to brain tissue; CSF equal to the density of water (0–10 HU), and fat the least dense (a negative HU value). This means that a resolving phase of hemorrhage may have a density equal to brain tissue, making it inapparent. Hyperdense lesions suggest recent blood, hemorrhagic lesions such as metastases, hypercellular lesions like lymphoma, and meningioma, calcification, and bone. Hypodense abnormalities include infarcts greater than 12 hours, brain tumors, inflammation, old blood, edema, traumatic changes, fat, cysts, and air. Enlargement of the ventricles suggests atrophy, obstruction, or NPH. MRI can identify ring-enhancing lesions (abscess, partially thrombosed aneurysm, resolving stroke or infection, metastatic lesions, active demyelination, and radiation necrosis), amyloid angiography, arteriovenous malformations, brainstem lesions (especially if thin cuts obtained), dissection of cranial vessels, edema, hemorrhage (although in general not as well as CT in the acute setting), and tumor (with characteristic T1 and T2 densities for each type, location, presence, or absence of hemorrhage, edema, calcification) (Table 111-1, Table 111-2, and Table 111-3).
Commonly used MR imaging techniques are the following:
|
Nuclear medicine tests such as SPECT brain scan can provide functional information regarding Alzheimer’s and other neuro-dedenerative diseases, stroke and seizure. PET-CT scans, increasingly being used to provide global assessment for metastases in patients with known cancer, have important limitations. The total body PET-CT does not provide adequate screening for brain metastases. In many centers, the application of this to the head is regarded as a separate examination. Centers that include the head on total body PET-CT scans may be doing so primarily to compare foci of increased activity with brain activity as a standardization procedure.
CT and MRI are both utilized for a wide variety of increasingly specific examinations, although the choice of CT or MRI may not be based upon the small differences in the value of the data obtained. One primary issue is the rapidity with which the examination can be obtained and interpreted. In acute neurological disease changes, time is of the essence, negating any benefit of more sophisticated imaging even if it would result in less ionizing radiation or possibly provide further information or a specific diagnosis that could effect less urgent treatment decisions.
It is extremely important to consider the effect the neurological event is having upon the patient. The ability of the patient to tolerate the examination may be diminished by the neurological event even as it is evolving. A CT scan is a significantly shorter examination than an MRI. The value that might be added by MRI can easily be negated by patient motion during the lengthy data acquisition sequences; thus the additional information that is often obtained from MR needs to be balanced by the logistics and added time for MR exam on a case by case basis. The one exception is in acute stroke in which a fast diffusion sequence (a minute and half) can provide a definitive answer, especially when the CT is negative. Neurologic imaging for chronic neurological findings may be deferred and performed on an elective basis following discharge.
|
Abnormalities on Neuroimaging
Visualization of brain structure on imaging is generally based upon differences in gray and white matter and upon alterations of CSF spaces. Some disease processes are diffuse and others are focal. Focal abnormalities may be accompanied by changes in surrounding tissue. The importance of the identification of blood cannot be overstated, whether in an extra-axial collection, subarachnoid hemorrhage, or hemorrhage into brain tissue itself. Blood degradation over time leads to different MRI signal characteristics that identify blood and provide a timeline (Table 111-4 and Table 111-5).