Neural Blockade of Oral and Circumoral Structures
Morton B. Rosenberg
Joseph A. Giovannitti Jr.
James C. Phero
The ability to provide safe, effective local anesthesia is the foundation of clinical dentistry. Neural blockade of oral and circumoral structures can be achieved via extraoral or intraoral techniques. With their in-depth knowledge of intraoral anatomy and familiarity with the oral cavity, most dentists use the intraoral approaches. However, there may be specific indications in which one method is preferred over the other. The presence of anatomic anomalies, infection, the nature of an injury and the extent of the procedure, or the use of local anesthetic techniques for diagnosis or management for acute and/or chronic pain syndromes, for example, may mitigate for or against a particular technique, drug, or approach. Generally, the extraoral approach is designed to provide anesthesia of a major nerve trunk (e.g., V2, V3). The effect of this type of blockade is to block neural conduction to a wide area of the face, head, or neck.
This chapter discusses the most common intraoral techniques used by dentists to anesthetize soft and hard tissues of the oral cavity. Local anesthetic techniques involving both intraoral and extraoral approaches to the trigeminal nerve are reviewed. In addition, the armamentarium unique to dentistry and the pharmacology of the local anesthetics routinely employed are presented.
Intraoral local anesthesia, as well as dental therapy, is often complicated by the existence of multifactorial psychological considerations associated with the delivery of dental care. Anticipation of pain is the most common cause of anxiety associated with a dental visit and accounts for the avoidance behavior of 6% to 9% of the U.S. population who neglect needed dental care (1), and it is responsible for the large number of dental phobics who find dental treatment highly stressful. It is imperative for health care professionals to understand and appreciate these issues and employ perioperative behavioral management strategies such as progressive relaxation, hypnosis, biofeedback, systematic desensitization, or the use of sedative drugs to reduce anxiety, fear, and apprehension to acceptable levels. Like any regional anesthetic technique, the effectiveness and utility of any intraoral injection depends upon patient considerations, the extent and duration of the procedure, and the skill and experience of the clinician. Every clinician should be aware of her skill limitations, as well as the limitations of the contemplated technique and agents. These factors must be clearly understood, as they will directly impact on successful outcomes and the potential for severe complications. The management of the apprehensive dental patient remains one of the most challenging problems in health care.
Preparation
As with any anesthetic, medical, dental, or surgical procedure, a careful and thorough preoperative evaluation including, but not limited to, a review of the medical history with special emphasis on past anesthetic experiences, focused physical examination, and determination of physical status and the potential of drug interactions must be conducted prior to selection of technique and agents. Based on this information and practitioner knowledge base, a reasonable and rational anesthesia plan, taking into account the risk–benefit balance, may be successfully formulated.
Special Injection Considerations
Patient Position
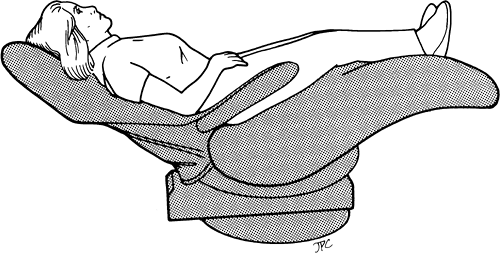
Intraoral injections are best achieved with the patient seated comfortably in a semireclining position (Fig. 18-1). This position offers at least two distinct advantages over the conventional upright or horizontal position. First, the oral cavity can be easily accessed and landmarks identified to provide optimal working conditions for the dentist. Second, this position provides a physiologically sound cardiovascular and respiratory position. Venous return is facilitated from both upper and lower extremities, and diaphragmatic movement is unrestricted. Vasodepressor syncope remains the most common medical emergency in dentistry and is often associated with the administration of local anesthesia. This may be due to the high incidence of phobia and stress or the anticipated (and sometime actual) pain that is often associated with intraoral injections.
Tissue Preparation
Tissue preparation for regional anesthesia at extraoral sites involves disinfection of the area with a suitable preparatory solutions and the use of appropriate aseptic technique. For local anesthetic injections within the oral cavity, true “asepsis” is neither necessary nor attainable. Nevertheless, certain basic principles may be adhered to, to reduce the risk of infection, particularly into deep structures. Prior to injection, the hands of the operator should be scrupulously cleansed and gloved. A surgical mask and eye protection is worn to protect the operator from inadvertent exposure to blood, saliva, or mucus. Prior to inserting a needle into the tissues of the oral cavity, the operator should dry the area with a sterile cotton-tipped
applicator or a 2 × 2 gauze sponge. A suitable topical antiseptic may then be applied to the site of injection, and the antiseptic wiped from the tissue to prevent its introduction into the tissues during needle penetration.
applicator or a 2 × 2 gauze sponge. A suitable topical antiseptic may then be applied to the site of injection, and the antiseptic wiped from the tissue to prevent its introduction into the tissues during needle penetration.
Topical Anesthesia
The topical application of a local anesthetic can play an important role in reducing the pain of needle insertion. It also provides psychological reinforcement to the patient that everything is being done to reduce pain. Topical anesthesia usually only reaches a depth of 2 to 3 mm and is usually achieved using high concentrations of benzocaine or lidocaine. A new addition to the dental topical local anesthesia armamentarium is the introduction of a periodontal topical eutectic local anesthetic gel consisting of 2.5% lidocaine and 2.5% prilocaine that is expressed as a liquid onto the gingiva and becomes an adherent gel at body temperature (2).
Supplies and Equipment
Although in theory similar to the armamentarium used for other types of neural blockade, the equipment used in dentistry for intraoral anesthesia is sufficiently different enough to warrant description. Traditional plastic syringes and needles with Luer-Lok hubs can be substituted for this specialized equipment, but are unwieldy in the dental environment. The equipment used in dentistry intraoral neural blockade (3) includes:
Glass cartridges containing the anesthetic solution
Aspirating syringes
Needles
Auxiliary equipment and supplies
Cartridge
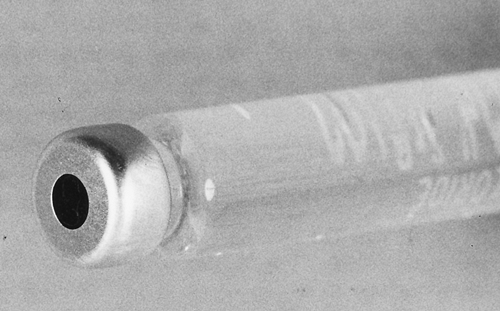
The introduction of the single-use local anesthetic cartridge for dentistry was a major advance because it ensured sterility, uniformity of solution composition, reduced cost, and integration into the dental aspirating syringe system. The cartridge is a glass tube sealed at one end by a movable rubber stopper that can be forced into the tube by the plunger of the cartridge-type syringe (Fig. 18-2). The other end of the tube is sealed by an aluminum cap over a rubber or latex-free diaphragm that is punctured by the cartridge end of the needle (Fig. 18-3). Cartridges are hermetically sealed and contain approximately 1.8 mL of local anesthetic solution.
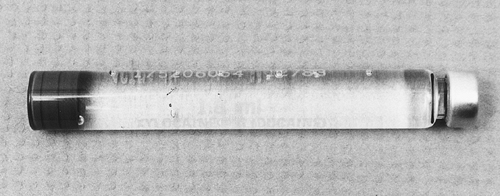 Figure 18-2. Needle end (right) of the cartridge is sealed with a metal cap. A rubber plunger at the other end is used to expel the contents. |
Cartridges are supplied by the manufacturer in either vacuum-packed cans or sealed cartons. Local anesthetic cartridges are color-coded as to their contents. After the package containing the cartridges has been opened, it is recommended that cartridges be stored in their original container at room temperature. Cartridges should not be placed or submerged in any germicide, since germicides may corrode the metal caps or penetrate the rubber stopper, and the potentially neurolytic germicidal agent may eventually seep into the cartridge.
The contents of a dental local anesthetic cartridge include the local anesthetic drug, sodium chloride, and sterile distilled water. A vasoconstrictor, such as epinephrine or levonordefrin, may often be present, as well as sodium bisulfite, which acts as a preservative for the vasoconstrictor. Local anesthetic cartridges should never be heat-sterilized as this will cause deterioration of the vasoconstrictive agent. The internal contents of the local anesthetic cartridges are sterile. If the cartridges are to be used in a sterile system, they should be disinfected with an appropriate agent prior to handling. The shelf life of a plain local anesthetic solution (no vasoconstrictor) in a dental cartridge is approximately 48 months. Local anesthetic solutions containing epinephrine and levonordefrin have shelf lives of 18 months and 12 months, respectively.
Problems with Cartridges
Despite quality control in the manufacturing of local anesthetic cartridges, several minor problems may develop:
Bubbles. Small bubbles (1–2 mm) may be visible within the cartridge. These bubbles are usually nitrogen gas, which has been introduced into the cartridge during the manufacturing
process to prevent oxygen from entering the cartridge, the presence of which would cause deterioration of the vasoconstrictor. Although these small bubbles are harmless, large bubbles in cartridges, with or without plungers extruded beyond the end of the cartridge, may be caused by freezing during transit and should be discarded.
Extruded plungers. Extruded plungers in cartridges that contain no bubbles usually indicate that the cartridge has been stored in disinfecting solution and that some of the solution has passed through the rubber stopper or diaphragm and contaminated the anesthetic solution. These should be discarded.
Corrosion of aluminum cap. Corrosion of the cap is usually caused by immersing the cartridge in chemical disinfecting solutions that contain nitrate antirust materials; these cartridges should not be used.
Syringes
The most commonly used syringe in dentistry for intraoral injections is the metal, side-loading metal cartridge aspirating syringe (Fig. 18-4). These syringes are extremely durable, autoclavable, accept a wide variety of cartridge and needles, and can produce negative pressure during the injection process.
To load, the piston is retracted and the cartridge inserted, plunger end first, into the syringe (Fig. 18-5A). Next, the piston is pushed forward with moderate pressure until the harpoon on the plunger (Fig. 18-5B) is firmly engaged into the rubber stopper. This will allow the stopper to be advanced and withdrawn when negative or positive pressure is applied to the piston to facilitate aspiration. The needle is then affixed to the threaded end of the syringe and pierces the diaphragm of the cartridge (Fig. 18-5C). A few drops of solution are expressed to ensure that the unit is properly assembled and ready for use (Fig. 18-5D).
 Figure 18-4. Metal aspirating syringe that can be resterilized. (Courtesy of Cook-Waite Laboratories, Inc., New York.) |
Several other types of cartridge syringe systems may be used for intraoral injections. One of these is the self-aspirating, cartridge-type syringe, which is a variation of the conventional side-loading syringe previously described. This syringe has no barbed or harpoon plunger, but instead allows aspiration to occur by depression of a thumb disk at its base. This action causes distortion of the cartridge diaphragm, which then rebounds as the thumb disk is released, producing negative pressure. Subsequently, during the injection process, any release of forward plunger pressure will result in negative pressure in the syringe, resulting in aspiration.
Needles
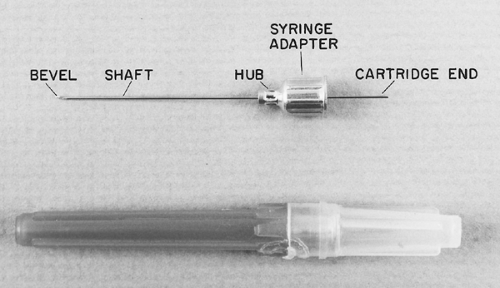
Needles designed for use in the standard dental syringe are divided into five parts: the bevel, shank, hub, syringe adapter, and syringe end of the needle (Fig. 18-6). Needles for intraoral injection range from 30 to 25 gauge and from 1.5 to 5 cm in length and are for one-time use. For deep intraoral injections, the 25-gauge, 5 cm needle is preferred by most practitioners. This needle may be inserted painlessly and directed to the
desired site with minimal deflection, yet is of sufficient gauge to allow reliable aspiration.
desired site with minimal deflection, yet is of sufficient gauge to allow reliable aspiration.
Emergency (Resuscitation) Equipment
Because complications and emergencies can occur during the administration of any local anesthetic, it is imperative that medical emergency equipment and supplies be immediately available and that practitioners who use these drugs be proficient in resuscitation (see Chapter 5).
Although local anesthesia within the oral cavity generally uses relatively small doses and volumes of local anesthetic drugs, the head and neck is a very vascular area, with direct and immediate connection to the central nervous system (CNS). Unintentional intra-arterial or intravenous (IV) injection or the rapid absorption of even relatively small amounts of local anesthetic doses may result in immediate and severe toxic manifestations of local anesthetic toxicity. Indeed, it is estimated that 90% of all medical emergencies occurring in dental offices occur in conjunction with, but are not necessarily directly attributable to, the administration of local anesthesia. Acute medical emergencies such as angina, syncope, hyperventilation
syndrome, acute-onset seizure activity, bronchospasm, and myocardial infarction have all been reported to have been precipitated by anticipatory fear, pain, and accidental intravascular injections (4) (see also Chapter 5).
syndrome, acute-onset seizure activity, bronchospasm, and myocardial infarction have all been reported to have been precipitated by anticipatory fear, pain, and accidental intravascular injections (4) (see also Chapter 5).
Local Anesthetic Solutions
Although any available local anesthetic solution acceptable for neural blockade in other parts of the body may be used for regional anesthesia of the head and neck, only eight agents are currently available in cartridge form for dentistry (Table 18-1). It is important to note that procaine (Novocaine), the first local anesthetic with true dental utility, is no longer available in North America in dental cartridges. Therefore, only amide local anesthetics constitute the dental local anesthetic armamentarium.
As in other types of neural blockade, the choice of anesthetic agent and amount, type, and concentration of vasoconstrictor is based on many factors such as physical status, age, and weight of the patient, duration of the procedure, and the need for hemostasis. Local anesthesia toxicity is a concern whenever large volumes of concentrated local anesthetic are used. Clinicians must to avoid injecting more milligrams per kilogram than is recommended to avoid a toxic response with the potential of leading to CNS, respiratory, and cardiac depression. When a large volume of local anesthetic must be administered, the incidence of toxicity can be avoided by using the lowest concentration of local anesthetic that will produce the required block and calculating the maximum volume of this solution that each patient may receive in advance of starting the injection. This is especially true in pediatric, severely compromised, and geriatric patients, in whom drug toxicity can become a life-threatening complication if maximum doses are not strictly followed (Table 18-2).
Table 18-1 Local anesthetics in cartridge form | |||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||
In the past, dental local anesthetic cartridges also contained methylparaben as a bacteristatic agent. Since the dental anesthetic cartridge is designed for one-time use, methylparaben has been eliminated. On the other hand, sodium (meta) bisulfite as an antioxidant is present in any dental cartridge containing a vasopressor (epinephrine or levonordefrin) to prevent oxidation and a decrease in potency.
Since 1948, lidocaine, the first amino-amide local anesthetic, became the “gold standard” against which all other dental local anesthetics are compared. Lidocaine, mepivacaine, and prilocaine combined with a vasoconstrictor provide reliable and profound pulpal anesthesia for approximately 60 minutes with a duration of soft tissue anesthesia ranging from 3 to 5 hours (5).
The increase in longer and more invasive surgical procedures with significant postoperative pain led to the introduction of longer-acting local anesthetics available in the dental cartridge. Currently, bupivacaine, 0.5% with 1:200,000 epinephrine is the only long-lasting local anesthetic available in dental cartridges in North America. Despite its relatively long onset (6 to 10 minutes), injections of bupivacaine with up to 12 hours of soft tissue anesthesia play an important role in reducing pain in the postoperative period.
Articaine, the newest local anesthetic available in dental cartridges, was introduced in 1976 in Europe and in 2000 in the United States. Articaine with epinephrine appears to have a similar clinical profile as lidocaine, mepivacaine, and prilocaine with vasoconstrictors (6). Despite the anecdotal reports of greater success and efficacy with articaine than with other local anesthetics, at this time, a lack of evidence supports these claims. Controversy also exists concerning reports
that the 4% local anesthetic solutions (articaine and prilocaine) may be implicated in a slightly higher rate of prolonged paresthesia following inferior alveolar block than other agents (7).
that the 4% local anesthetic solutions (articaine and prilocaine) may be implicated in a slightly higher rate of prolonged paresthesia following inferior alveolar block than other agents (7).
Table 18-2 Duration and maximum safe dosage of agents used in dentistry | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Vasoconstrictors
Vasoconstrictors are used to prolong the duration of anesthetic effect, decrease the rate of absorption of local anesthetics, and decrease localized bleeding at the site of administration. The most pronounced effect on duration is achieved by adding a vasoconstrictor to lidocaine and mepivacaine. By contrast, addition of a vasoconstrictor to bupivacaine does little to prolong its duration, as this drug produces prolonged duration of anesthesia following mandibular block, primarily because of bupivacaine’s high degree of lipid solubility. The two most commonly used vasoconstrictors in dentistry are epinephrine and levonordefrin. In dental cartridges, epinephrine is available in three concentrations, 5 μg/mL (1:200,000), 10 μg/mL (1:100,000), and 20 μg/mL (1:50,000). A standard dental cartridge with 1:100,000 epinephrine contains 18 μg of epinephrine. Levonordefrin is found only in dental cartridges containing mepivacaine, in a concentration of 50 μg/mL (1:20,000). A standard dental cartridge with 1:20,000 levonordefrin contains 90 μg of levonordefrin. Although levonordefrin is a relatively weaker adrenergic agonist than epinephrine, consideration should be given to the fact that the 1:20,000 concentration is five times greater than the standard concentration of epinephrine. Therefore, fewer cartridges containing levonordefrin may be safely used in comparison with cartridges containing epinephrine. Table 18-3 gives generally accepted dosages for vasoconstrictors in healthy patients, as well as in those with cardiovascular compromise.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree