Neural Blockade for Orthopedic Surgery
Xavier Capdevila
Paul Zetlaoui
Stephen Mannion
Anesthesia for orthopedic surgery is a significant anesthetic subspecialty. The concurrent use of antithrombotic therapy, risk of significant blood loss, increased difficulties in airway management, and the common use of neural blockade require specialized anesthesiologists. Furthermore, the ability to perform safe and effective regional anesthesia/analgesia is a prerequisite skill for an anesthesiologist working in the field of orthopedic surgery.
Risks and contraindications of Neural Blockade in Orthopedic Surgery
For every patient and orthopedic procedure, there is invariably a neural block that can be performed, even if general anesthesia is also indicated. The advantages of neural blockade, especially for postoperative analgesia, indicate that most patients presenting for orthopedic surgery should receive neural blockade unless specific contraindications exist.
Sepsis and Neural Blockade
Performing Regional Anesthesia in Septic Patients
Perioperative infection or septic complications are not unusual in orthopedic patients and may result in revision surgical procedures. It is still a matter of debate whether neuraxial blockade can be performed safely in septic patients. Recent recommendations state that (1):
Even if the risk of central neuraxial infection is very low after spinal or epidural anesthesia or analgesia, the decision to perform a central blockade must be established on an individual basis, whenever a patent risk of infection is present.
Central neural blockade should not be performed in patients with an untreated or uncontrolled septic state.
Conversely, a controlled infection is not a contraindication for regional anesthesia, if appropriate antibiotic therapy has been initiated before the block and there is evidence of clinical improvement.
Recommendations are less evident for plexus or peripheral anesthesia. Overall, it appears that, when the puncture is performed distant from the site of infection (axillary block for hand infection), a peripheral block can be performed safely in cases of local infection, after verifying that no infective lymphadenopathy is present at the puncture site. However, case reports suggest that local anesthesia is less efficient if local infection, such as paronychia or acute infection of the fingers or toes, is present. The causes for this are not clearly understood, but the addition of clonidine to local anesthetics can shorten the onset time and enhance the quality of both anesthesia and analgesia (2).
Infectious Complications of Regional Anesthesia and Analgesia
Infective complications may be catastrophic events in patients undergoing orthopedic surgery, especially following arthroplasty, and antibiotic prophylaxis guidelines and aseptic techniques must be respected to prevent these from occurring (3).
The infectious risk of regional anesthesia is very low, particularly after single-injection plexus or peripheral blocks. There are few case reports of infection after single-injection neural techniques in chronic pain patients despite the concurrent use of steroids or nonsteroidal anti-inflammatory drugs (NSAIDs). The use of neuraxial or peripheral catheters does raise concerns regarding infective complications. Several studies have confirmed a risk of bacterial colonization of the catheter (4,5,6,7). A large survey by Capdevila and co-workers, involving nearly 1,500 patients, reported that the incidence of bacterial colonization of catheters was about 30% (4). However, only 3% of patients had signs of local inflammation. Risk factors for local inflammation or infection were postoperative monitoring in an intensive care setting, catheter duration greater than 48 hours, male gender, and the absence of antibiotic prophylaxis. Despite these findings, clinical infection is very rare and there are no reports of septic prothesis complications related to a peripheral neural catheter.
The use of an epidural catheter for postoperative analgesia is controversial because of the potential for rare but serious complications from neuraxial infection (6). The incidence of bacterial colonization is also nearly 30%. However, similarly, clinical infection is very rare; the incidence of epidural abscess has been reported as 0.12% in a controlled study involving 800 patients (6). As the bacterial species most frequently found were coagulase-negative staphylococcus (in two-third of cases) proper skin preparation, dressing, and asepsis are required for catheter placement (4,6,7).
Regional Anesthesia and Disorders of Coagulation
Coagulation Disorders
In most cases, inherited coagulation disorders such as hemophilia or von Willebrand disease are traditionally considered
absolute contraindications for regional anesthesia. Only intravenous (IV) regional anesthesia is usually recommended for these patients. However, a recent study by Marcou and Zetlaoui reported the safe placement and use of continuous femoral nerve block for total knee arthroplasty in hemophiliac patients (8). After appropriate factor substitution, the use of peripheral neural blockade is possible in these patients if performed by an experienced anesthesiologist using a nerve stimulation or ultrasonographic technique. Neuraxial blockade is contraindicated because of the risk of blind, uncontrolled, and late bleeding.
absolute contraindications for regional anesthesia. Only intravenous (IV) regional anesthesia is usually recommended for these patients. However, a recent study by Marcou and Zetlaoui reported the safe placement and use of continuous femoral nerve block for total knee arthroplasty in hemophiliac patients (8). After appropriate factor substitution, the use of peripheral neural blockade is possible in these patients if performed by an experienced anesthesiologist using a nerve stimulation or ultrasonographic technique. Neuraxial blockade is contraindicated because of the risk of blind, uncontrolled, and late bleeding.
Table 25-1 Neuraxial anesthesia in the patient receiving thromboprophylaxis | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||
Antithrombotic Agents
Patients receiving regional anesthesia, especially neuraxial blocks, are at risk of serious hemorrhagic complications if they are treated with thrombolytic or fibrinolytic agents, as a result of the profound effects of these drugs on hemostasis and the risk of bleeding related to regional anesthesia. Furthermore, it is likely that the clinical risk of bleeding is increased when several agents, such as heparin or its derivatives (low-molecular-weight heparin; LMWH), pentasaccharide, warfarin, aspirin, NSAIDs, or other antiplatelet medications (clopidogrel or ticlopidine) are used concurrently in the perioperative period. According to the American Society of Regional Anesthesia and Pain Medicine (ASRAPM) recommendations, regional techniques can be performed in patients treated with antithrombotic agents. The recommendations of the ASRAPM are reported in Table 25-1 (9). The timing of the initial LMWH dose, as well as that of subsequent doses, relative to the neuraxial block is especially challenging if a catheter is placed. According to local practice, each clinical team must propose and respect written guidelines to ensure patient safety (10).
Preexisting Central Nervous System Disorders
The presence of a preexisting central nervous system (CNS) disorder is typically considered a contraindication for neuraxial blockade. The postulated risk of worsening neurologic outcome following a mechanical trauma, a drug-induced toxicity, or neural ischemia is commonly reported as contraindication to neuraxial blockade in patients suffering from these conditions. A retrospective study from the Mayo Clinic involving 139 patients with a CNS disorder who underwent spinal anesthesia or epidural anesthesia/analgesia showed no new postoperative worsening of the preexisting CNS disorder (11). These results suggest that a preexisting CNS disorder is not an absolute contraindication for neuraxial blockade, but support an
individualized discussion with the patient regarding the risk–benefit profile. However, two subgroups of patients appear to be at higher risk of neurologic complication after neuraxial blockade: (a) patients presenting with uncontrolled or unstable CNS disorders such as Guillain-Barré syndrome and (b) patients suffering from chronic, stable, neurologic sensorimotor or diabetic polyneuropathies. These patients are at increased risk of new or progressive postoperative neurologic deficits after neuraxial blockade (12). In a retrospective study including 567 stable patients, the risk of worsening or developing a new neurologic dysfunction after neuraxial blockade has been found to be 0.4% (13).
individualized discussion with the patient regarding the risk–benefit profile. However, two subgroups of patients appear to be at higher risk of neurologic complication after neuraxial blockade: (a) patients presenting with uncontrolled or unstable CNS disorders such as Guillain-Barré syndrome and (b) patients suffering from chronic, stable, neurologic sensorimotor or diabetic polyneuropathies. These patients are at increased risk of new or progressive postoperative neurologic deficits after neuraxial blockade (12). In a retrospective study including 567 stable patients, the risk of worsening or developing a new neurologic dysfunction after neuraxial blockade has been found to be 0.4% (13).
Amputees
Although it has been suggested that in scheduled limb amputation perioperative neuraxial blockade could prevent severe phantom limb pain, the use of spinal anesthesia in amputees has a low (5%) but real risk of phantom pain recurrence (14,15). Rare cases have also been reported after peripheral plexus blocks (16). Accordingly, spinal anesthesia or plexus blocks are relatively contraindicated for patients with previous lower limb amputation, and their use should be made on an individual basis considering the anesthetic alternatives.
Performance of Regional Anesthesia in Anesthetized Patients
In orthopedic surgery, association of general anesthesia with regional anesthesia (or analgesia) is common practice, but the timing of regional anesthesia in relation to general anesthesia remains controversial. Benumof, on the basis of four cases, stated that interscalene block should not be performed in anesthetized patients because of the risk of spinal cord injury (17). Prospective studies do not demonstrate an increased risk of neurologic complications associated with regional anesthesia performed under general anesthesia (18,19). Two studies report that the risk of neural damage after epidural or subdural catheter placement in anesthetized patients is very low and probably not different from the relative risk of neuraxial catheter placement in awake patients (20,21). However, according to Benumof, it should be recommended in current practice to perform regional anesthesia in awake or lightly sedated patients. Regional anesthesia performed under general anesthesia is not contraindicated, but should only be considered as an alternative technique in suitable cases.
Advantages of Regional Anesthesia in Orthopedic Surgery
Emergencies
The use of regional anesthesia in the management of a patient undergoing emergency surgery is a reasonable choice because of the nonfasted state and often preoperative pain. Plexus or peripheral blocks are suitable for limb surgery in emergency conditions, as they assure preoperative and postoperative analgesia, and intraoperative anesthesia. Depending on the technique and the administered drugs, extensive or long-duration surgery such as finger replantation is possible. The placement of a perineural catheter should be considered early in these patients as the duration of surgery may be unpredictable (operating room time, staff availability), and continuous techniques provide reliable pain relief, especially if repeated procedures are necessary (22).
In civilian or war casualties, large series or cases reports describe the use of regional anesthesia for pain control in femoral shaft fracture, and hand or foot trauma. If regional anesthesia is suitable for a trauma patient, techniques are selected on the basis of surgical site, presence of fractures and associated injuries, and need for prolonged analgesia. For example, for elbow, forearm, and hand surgery, infraclavicular block is perhaps a good choice, as it does not need upper limb mobilization (23). Furthermore, ultrasound-guided infraclavicular block without nerve stimulation may be a better choice, as movement of the limb and hence fracture is avoided. Although often sufficient, IV regional anesthesia (Bier block) may be unsuitable for a Colles fractures, because wrapping the fracture with an Esmarch bandage is a painful procedure and IV regional anesthesia does not provide postoperative pain control after open surgical repair. In case of confirmed or suspected traumatic pneumothorax, interscalene and supraclavicular block should be replaced with distal approaches to the brachial plexus.
For lower limb traumatic emergencies, anterior or lateral thigh or lateral popliteal approaches of the sciatic nerve are preferred, as they do not require moving the trauma patient. After hip fracture, early fascia iliaca block provides efficient preoperative analgesia and allows pain-free patient positioning for spinal anesthesia if indicated (24,25). The main disadvantage of spinal and epidural anesthesia in trauma patients is hypovolemia related to hemorrhage, dehydration, and the affects of chronic medication such as angiotensin antagonists on vascular tone.
Finally, although the risk of compartment syndrome must be considered in all limb injuries, high-impact traumatic fractures of the forearm and leg are at highest risk. It is important that the orthopedic and anesthetic teams discuss patient management concerning the use of regional anesthesia and the risk–benefit profile (26). If regional anesthesia is performed, the use of short-acting local anesthetics, compartment pressure monitoring, and increased clinical vigilance are sensible precautions. The use of IV regional anesthesia is best avoided because of tourniquet placement, with subsequent local anesthetic volume injection (27).
Ambulatory Surgery
Regional anesthesia techniques such as spinal anesthesia and peripheral nerve blocks (PNBs) are ideal techniques for ambulatory surgery. There is excellent evidence that these techniques provide effective and rapid-onset anesthesia and, compared with general anesthesia, reduce adverse effects and unanticipated hospital admission and provide improved postoperative analgesia, especially if continuous PNBs are performed.
Spinal anesthesia provides fast, reliable, and profound surgical block with a single injection of small amounts of local anesthetics. Disadvantages of using spinal anesthesia in the outpatient setting relate to the effect of spinal block on the recovery of motor and bladder function after the block and the risk of postdural puncture headaches. A recent study compared clinical markers of motor block resolution (Bromage scale) and objective data of functional balance (ability to safely ambulate). The results of the study suggest that the standard markers of motor function are poor predictors of functional balance following ambulatory spinal anesthesia, and the actual
ability to walk was more important for safe patient discharge (28). Mulroy and co-workers recently evaluated the efficacy and safety of applying an accelerated discharge pathway after spinal block by not requiring the patient to void (29). This study suggested that waiting for voiding after short-duration spinal anesthesia for surgical procedures with a low-risk of urinary problems might be not necessary, and could result in prolonged discharge time. Accordingly, the dose and drug used for spinal anesthesia must be balanced to achieve the fastest recovery of unassisted ambulation after the procedure while maintaining adequate efficacy of intraoperative anesthesia. Lidocaine provides intense and short-lasting spinal block. However, in the last 10 years, the occurrence of transient neurologic symptoms (TNS) after spinal lidocaine has increased concerns about its use. Freedman and colleagues, evaluating the epidemiology and risk factors for TNS after spinal anesthesia in more than 1,800 patients, clearly demonstrated that TNS was associated with lidocaine spinal anesthesia (30). Other authors have recommended the use of very low doses of local anesthetics (lidocaine or bupivacaine) that have an incidence of side effects lower than that previously reported with 50 to 60 mg lidocaine and a time to discharge of 145 minutes (31,32). However, this reduction in doses of local anesthetics requires the addition of intrathecal opioids (20–25 μg fentanyl) to improve analgesia. Very good results have been reported with small doses of long-acting agents such as bupivacaine (8 mg of iso- and hyperbaric solutions) and using the concept of unilateral spinal block for orthopedic lower limb surgery (33,34). It has been recently reported that small doses of ropivacaine (10–12 mg) could be an acceptable option for ambulatory surgery, allowing fast recovery of ambulation after the procedure, with discharge times similar to those for small-dose lidocaine anesthesia (35). In some patients, epidural anesthesia may be used with or without general anesthesia. Williams and colleagues demonstrated that combined general and regional anesthesia care is better than general anesthesia alone (36). Patients with the combined technique showed improved recovery profiles, had fewer unanticipated hospital admissions, and required fewer nursing interventions for common postoperative symptoms. Patients receiving epidural anesthesia had discharge outcomes similar to those patients receiving general anesthesia with femoral nerve block. Postanesthesia care unit (PACU) bypass (fast-tracking) was more likely in patients in the regional anesthesia (peripheral or spinal) clinical pathway when compared to the general anesthesia clinical pathway (see also Chapter 26).
ability to walk was more important for safe patient discharge (28). Mulroy and co-workers recently evaluated the efficacy and safety of applying an accelerated discharge pathway after spinal block by not requiring the patient to void (29). This study suggested that waiting for voiding after short-duration spinal anesthesia for surgical procedures with a low-risk of urinary problems might be not necessary, and could result in prolonged discharge time. Accordingly, the dose and drug used for spinal anesthesia must be balanced to achieve the fastest recovery of unassisted ambulation after the procedure while maintaining adequate efficacy of intraoperative anesthesia. Lidocaine provides intense and short-lasting spinal block. However, in the last 10 years, the occurrence of transient neurologic symptoms (TNS) after spinal lidocaine has increased concerns about its use. Freedman and colleagues, evaluating the epidemiology and risk factors for TNS after spinal anesthesia in more than 1,800 patients, clearly demonstrated that TNS was associated with lidocaine spinal anesthesia (30). Other authors have recommended the use of very low doses of local anesthetics (lidocaine or bupivacaine) that have an incidence of side effects lower than that previously reported with 50 to 60 mg lidocaine and a time to discharge of 145 minutes (31,32). However, this reduction in doses of local anesthetics requires the addition of intrathecal opioids (20–25 μg fentanyl) to improve analgesia. Very good results have been reported with small doses of long-acting agents such as bupivacaine (8 mg of iso- and hyperbaric solutions) and using the concept of unilateral spinal block for orthopedic lower limb surgery (33,34). It has been recently reported that small doses of ropivacaine (10–12 mg) could be an acceptable option for ambulatory surgery, allowing fast recovery of ambulation after the procedure, with discharge times similar to those for small-dose lidocaine anesthesia (35). In some patients, epidural anesthesia may be used with or without general anesthesia. Williams and colleagues demonstrated that combined general and regional anesthesia care is better than general anesthesia alone (36). Patients with the combined technique showed improved recovery profiles, had fewer unanticipated hospital admissions, and required fewer nursing interventions for common postoperative symptoms. Patients receiving epidural anesthesia had discharge outcomes similar to those patients receiving general anesthesia with femoral nerve block. Postanesthesia care unit (PACU) bypass (fast-tracking) was more likely in patients in the regional anesthesia (peripheral or spinal) clinical pathway when compared to the general anesthesia clinical pathway (see also Chapter 26).
Peripheral nerve blocks with long-acting local anesthetics are an attractive alternative for ambulatory surgery (37). These techniques are site-specific, have few side effects, and provide excellent surgical conditions, as well as superior analgesia compared to systemic opioids. Furthermore, despite analgesia with oral and intra-articular drugs, postdischarge pain with systemic opioids is often evaluated as moderate to severe. Mulroy and co-workers evaluated femoral nerve block for postoperative analgesia following outpatient arthroscopic anterior cruciate ligament repair (38). The authors reported that femoral nerve block with 25 mL of 0.25% bupivacaine provided good analgesia for the first 24 hours after surgery. Jankowski and co-workers compared psoas compartment block with low-dose spinal and general anesthesia for outpatient knee arthroscopy (39). Patients undergoing psoas compartment block received 40 mL of 1.5% mepivacaine with epinephrine. For patients receiving spinal anesthesia, 6 mg of isobaric bupivacaine with 15 μg of fentanyl were injected. General anesthesia was induced with propofol and fentanyl, and maintained with propofol and nitrous oxide. All patients received 20 mL of 0.25% bupivacaine intra-articularly at the end of the procedure. All patients receiving spinal anesthesia and all except one (inadvertent bilateral psoas compartment blocks performed with subsequent epidural anesthesia) receiving a psoas compartment block bypassed the PACU, whereas only 35% of general anesthesia patients were able to bypass. Discharge time did not differ among the three groups. There was no difference among groups regarding opioid consumption. However, pain scores were highest in general anesthesia patients until 2 hours postoperatively. The authors concluded that spinal anesthesia or psoas compartment block is superior to general anesthesia when considering hospital resource utilization. The advantages of single-injection PNBs may be limited because of the duration of long-acting local anesthetics (10–24 hours) (40). After resolution of PNBs, postoperative pain management is often difficult to manage and inadequate in the ambulatory setting. Continuous PNBs allow prolonged site-specific local anesthetic delivery in the outpatient setting, resulting in profound analgesia, minimal side effects, and avoidance of premature regression of an analgesic block. Klein and colleagues investigated 40 patients undergoing major shoulder surgery who received an interscalene block and perineural catheter preoperatively, and were randomized to receive either perineural ropivacaine 0.2% or normal saline postoperatively (10 mL/h) (41). Patients receiving perineural ropivacaine averaged 10 on a visual analog score (VAS) pain scale of 0–100 mm, compared with a 30 mm for subjects receiving placebo. Recent randomized double-blinded, placebo-controlled studies involving patients discharged at home with a patient-controlled never block (PCNB) provided interesting results (42,43,44). All of these studies involved patients scheduled for orthopedic surgery procedures who underwent placement of an infraclavicular (42), posterior popliteal (43), or interscalene (44) perineural catheter. Patients receiving perineural local anesthetics achieved both clinically and statistically significant lower resting and breakthrough pain scores compared with those using oral opioids for analgesia. Patients who received perineural local anesthetics experienced additional benefits related to improved analgesia. Zero to 30% of patients receiving perineural ropivacaine reported insomnia due to pain, compared with 60% to 70% of patients using only oral opioids. Patients receiving perineural ropivacaine awoke from sleep because of pain an average of zero times on the first postoperative night, compared with two times for patients receiving perineural saline. Lower opioid consumption in patients receiving perineural local anesthetics also resulted in fewer opioid-related side effects. Patients receiving perineural local anesthetics reported satisfaction ratings for their postoperative analgesia of 8.8 to 9.8 compared with 5.5 to 7.7 for patients receiving placebo. Recent prospective studies focusing on outcome benefits concluded that these techniques are not technically challenging and optimized the patient’s quality of life and postoperative rehabilitation at home (45,46,47) (see Chapter 26).
Anticipated Difficult Intubation
Performance of a regional anesthetic in a patient with an anticipated difficult intubation remains controversial (48). For lower limb, forearm, and hand surgery, regional anesthesia is often recommended in the case of anticipated difficult intubation, such as in patients with arthritic conditions. This recommendation is also suitable in the trauma patient. In the case of respiratory risk associated with regional anesthesia, such with the interscalene block, planned fiberoptic intubation is perhaps the better choice, rather than an emergency intubation in a
hypoxic patient with a difficult airway, such as in Still disease, ankylosing spondylitis, or rheumatoid arthritis.
hypoxic patient with a difficult airway, such as in Still disease, ankylosing spondylitis, or rheumatoid arthritis.
Difficult Neuraxial Regional Anesthesia
Rheumatologic patients suffering from spine deformity often require orthopedic lower limb or hip surgery. In some cases, especially in patients with ankylosing spondylitis or severe scoliosis, midline approach for spinal anesthesia may be impossible. Paramedian or lateral approaches may permit neuraxial blockade in these patients, and anesthesiologists working in orthopedic surgery must be familiar with these alternatives (49).
Rehabilitation
As general anesthesia is becoming increasingly safer, it will be more difficult to demonstrate that regional anesthesia and analgesia decreases postoperative mortality. However, evidence suggests that regional anesthesia and analgesia can improve patient rehabilitation after orthopedic surgery (19). In this area, better analgesic control can shorten duration of hospitalization and rehabilitation, improving the global result of surgery (50). In major knee surgery, postoperative analgesia with a continuous femoral nerve catheter increases maximum range of motion of the operated knee, shortens duration of physiotherapy, reduces pain and systemic analgesics, and improves surgical results (50,51).
Economical Aspects
Regional anesthesia is overall less expensive than general anesthesia for orthopedic surgery. Direct and indirect costs of surgery are often reduced with regional anesthesia. For example, Williams and colleagues showed that benchmarking the perioperative processes after having actively incorporated regional anesthesia led to reduced pharmacy and materials cost variability, slightly increased turnover time, improved intraoperative anesthesia and surgical efficiency, improved recovery times, decreased unanticipated admission rates, and a reduction in the number of nursing interventions required for common postoperative symptoms (52). Spinal anesthesia is less expensive than general anesthesia for hip or knee arthroplasty (53). Moreover, spinal anesthesia is often associated with lower postoperative pain in the PACU, leading to reduced administration of analgesics and antiemetics and reduction in PACU length of stay. Intravenous regional anesthesia has been reported as the more cost-effective technique for outpatient hand surgery (54). However, brachial plexus block is more expensive than general anesthesia for upper limb procedures of short duration (55). Shortening postoperative hospital stay and reducing the costs of rehabilitation are other potential economic advantages of regional anesthesia.
Regional Anesthesia for Spine Surgery
Minor Spine Surgery
Minor spine surgery is usually performed under general anesthesia; neuraxial anesthesia is infrequently used for spinal procedures (56). Although complications associated with neuraxial anesthesia are rare, spinal or epidural anesthesias have been avoided for spinal surgery as some authors have suggested that neuraxial anesthesia may exacerbate preexisting neurologic disease. However, in selected patients scheduled for intervertebral disk herniation surgery, spinal or epidural anesthesia are efficient alternatives (57). Patient acceptance is higher, and hypotension is less common when surgery is performed with the patient in the lateral position, compared to the standard knee-to-chest position. In the same way, epidural or spinal anesthesia have been compared to general anesthesia for one-level laminectomy (58). A study including 400 patients reported that neuraxial blockade is an intraoperative technique for lumbar laminectomy, and is also associated with several advantages such as a reduction in total operative time and PACU stay, less postoperative nausea and vomiting (PONV), less postoperative pain, and an overall reduction in the postoperative complication rate. Furthermore, bladder dysfunction was less frequent after spinal anesthesia as the total amount of morphine for postoperative pain was reduced.
Postoperative epidural analgesia for lumbar laminectomy results in superior pain control and fewer analgesic requirements than patient-controlled morphine analgesia (59). However, patients poorly accept procedures of long duration, and general anesthesia remains the better choice for spinal surgery of long or uncertain duration. In summary, spinal or epidural anesthesia and analgesia are efficient alternative techniques for nonextensive spine surgery and offer better postoperative pain control than conventional treatments, including patient-controlled morphine analgesia.
Major Spine and Pelvic Surgery
Major spine or pelvic surgery requires general anesthesia. However, evidence suggests that the association of general anesthesia combined with regional anesthesia improves intraoperative conditions and patient outcome.
Spinal Analgesia
Several studies reviewed by Tobias report the intraoperative use of spinal analgesia for extensive anterior or posterior spinal fusion in children (60). Although low doses of intrathecal morphine (2 and 5 μg/kg) are administered (61), most studies report the use of high-dose morphine, ranging from 10 to 20 μg/kg (62,63,64). These studies have reported better postoperative pain control in the treated groups and a significant decrease in intraoperative blood loss. The decrease in blood loss is postulated to be a result of intraoperative mild and stable hypotension and less hemodynamic reactivity to intraoperative painful stimulation. Furthermore, volatile anesthetic agents, unlike intraoperative spinal opioids (morphine or sufentanil), do not disturb spinal function monitoring (i.e., somatosensory-evoked potentials). No study reports the use of continuous intrathecal analgesia in spinal procedures. Patients receiving high-dose intrathecal opioids required admission to a more intensely monitored unit at least for the first 24 postoperative hours because of the risk of respiratory depression.
Local anesthetics are typically avoided for intraoperative spinal analgesia because of the increased risk of arterial hypotension, the impossibility of monitoring spinal function, and because of the risk of prolonged postoperative motor blockade, which may delay the early diagnosis of neurologic complications.
Epidural Analgesia
Unlike spinal analgesia, the use of perioperative epidural analgesia is more complex, as different options are available (intraoperative versus postoperative use, single-versus double-catheter, continuous infusion versus intermittent dosing, lipophilic versus hydrophilic opioids, additives). Epidural analgesia in extensive spinal surgery provides perioperative analgesia, mild intraoperative hypotension resulting in blood loss reduction, and, potentially, a reduction in postoperative venous thrombosis (65,66,67). The epidural catheter is usually placed before induction of general anesthesia. If nitrous oxide is used during surgery, the loss-of-resistance technique with air should be carefully considered because of the risk of patchy anesthesia or root compression by neuraxial gas bubbles when their volume is increased by nitrous oxide diffusion (68).
Alternatively, the epidural catheter may be placed under direct vision, by the surgeon at the end of the surgery. This technique allows the placement of two catheters, one directed caudally and the second directed cephalad, to ensure the quality of pain control. The placement of the catheter at the level of surgery results in a significant leak of analgesic solution from the epidural space (69).
Upper Limb
Orthopedic surgery of the upper limb may be performed under a large variety of regional anesthetic techniques including brachial plexus block, a combination of individual nerve blocks, or IV regional anesthesia. The choice of a particular technique depends on the need for a tourniquet, the site of surgery, and the anticipated duration of the procedure. Basically, for regional anesthesia, the upper extremity can be divided in four regions: (a) the shoulder and humeral head, (b) the arm and elbow, (c) the forearm, and (d) the wrist and hand. This anatomic division corresponds approximately to the different regional anesthetic techniques described (Table 25-2).
Table 25-2 Suggestions for block type and need for catheter placement for upper limb surgery | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Shoulder and Humeral Head
Shoulder and humeral head surgery can be performed under regional anesthesia alone, but sedation (70) or general anesthesia should be considered for patient comfort, especially for extensive procedures or when surgery is performed in the prone position.
From an anatomic point of view, interscalene block is the paradigm for shoulder surgery as it anesthetizes the roots of the brachial plexus (C5, C6, C7). However, additional blocks may be necessary according to the site of the surgical incision. For example, the superficial nerves of the cervical plexus innervate the anterosuperior aspect of the shoulder. The deltopectoral groove and the axilla are not blocked by an interscalene approach, as extension of the block to the lower roots (C8–T1) is infrequent or unpredictable. Thus, local infiltration for
cutaneous nerves or paravertebral nerves blocks (T2–T3) may be required.
cutaneous nerves or paravertebral nerves blocks (T2–T3) may be required.
Several studies have investigated the clinical efficacy of the interscalene block in shoulder surgery. Nearly all report the superiority of this technique for intraoperative and postoperative anesthesia and analgesia compared with other methods (71,72,73). In a randomized controlled study enrolling patients scheduled for an arthroscopic acromioplasty under general anesthesia, Singelyn and co-workers reported the superiority of the interscalene block for postoperative analgesia when compared with patient-controlled morphine analgesia, suprascapular nerve block, or intra-articular analgesia (74).
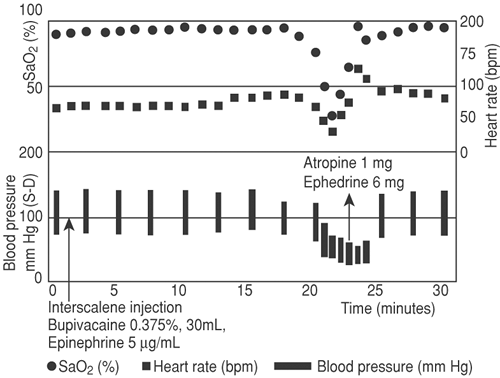 Figure 25-1. Record of a hemodynamic event after interscalene block for shoulder surgery in the beach-chair position. Redrawn from the automatic record. From P.J. Zetlaoui, personal data. |
The beach-chair position, used to avoid excessive traction on the shoulder (and hence plexus roots), is often required for open or arthroscopic shoulder surgery. The beach-chair position and interscalene block are associated with a high incidence (4%–20%) of significant hemodynamic events involving hypotension and/or bradycardia, sometimes leading to cardiac arrest (75) (Fig. 25-1). This reaction seldom occurs under general anesthesia alone or when interscalene block is combined with general anesthesia. It is more frequent when epinephrine is added in the irrigation solution or to the anesthetic mixture (76). Epinephrine-induced tachycardia and relative hypovolemia due to the beach-chair position are postulated to be major determinants of this hemodynamic compromise. This reaction has been misinterpreted as an activation of the Bezold-Jarisch reflex (75), but the review of Campagna and Carter stated that “the hemodynamic embarrassment seen in shoulder surgery during interscalene block appears not to be related with the Bezold-Jarisch reflex activation” (77), as this reflex is activated by an overfilled left ventricle and never by hypovolemia. Consequently, β-blockers are not required as prophylactic or therapeutic agents, and management of these vasovagal reactions includes fluid loading, ephedrine, atropine, and finally epinephrine use if necessary (78,79).
In emergency cases, such as shoulder dislocation, interscalene block is an effective technique for closed reduction. However, the performance of an interscalene block in such situations should be considered on an individual basis, considering that the nonfasted patient is a relative contraindication for interscalene block because of the risk of recurrent laryngeal nerve paresis with this block (80).
In a review of neurologic complications after shoulder surgery, Boardman and Cofield reported an incidence of 1% to 8%, depending on the specific procedure performed (81). Although traditionally interscalene block was often held responsible for a significant part of these complications, this review reported that surgery and intraoperative position are the major determinants for postoperative neurologic complications, and that the contribution of regional anesthesia is very low. The study of Borgeat and colleagues reports that the incidence of interscalene block–related early or late neurologic complications is about 0.4% (82). These findings are supported by the study of Horlocker and colleagues, who report that the incidence of surgery-related neurologic complications is eight times more frequent than anesthetic-related injuries (83). However, the description by Benumof of four cases of spinal cord damage after interscalene block (17) should be considered and suggests that another approach for the interscalene block, such as that proposed by Borgeat using a lateral modified approach, is considered (84). This approach allows easy catheter placement, less catheter dislodgement, high patient satisfaction, and probably less neurologic risk.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








