Neural Blockade for Cardiovascular Surgery
Mark A. Chaney
Adequate postoperative analgesia prevents unnecessary patient discomfort, may decrease morbidity, may decrease postoperative hospital length of stay, and may thus decrease cost. Because postoperative pain management has been deemed important, the American Society of Anesthesiologists has published practice guidelines regarding this topic (1). Furthermore, in recognition of the need for improved pain management, the Joint Commission on Accreditation of Healthcare Organizations has recently developed standards for the assessment and management of pain in accredited hospitals and other health care settings (2).
Surgical or traumatic injury initiates changes in the peripheral and central nervous system that must be addressed therapeutically to promote postoperative analgesia and, potentially, improve clinical outcome. The physical processes of incision, traction, and cutting of tissues stimulate free nerve endings and a wide variety of specific nociceptors. Receptor activation and activity is further modified by the local release of chemical mediators of inflammation and sympathetic amines released via the perioperative surgical stress response. The perioperative surgical stress response peaks during the immediate postoperative period following cardiovascular surgery (intraoperative period during cardiac surgery associated with cardiopulmonary bypass) and exerts major effects on many physiologic processes (many detrimental). The potential clinical benefits of attenuating the perioperative surgical stress response has received much attention during the last decade and remains controversial (3). However, it seems clear that inadequate postoperative analgesia and/or an uninhibited perioperative surgical stress response following cardiovascular surgery has the potential to initiate pathophysiologic changes in all major organ systems, including the cardiovascular, pulmonary, gastrointestinal, renal, endocrine, immunologic, and/or central nervous system, all of which may lead to substantial postoperative morbidity.
Achieving optimal pain relief following cardiovascular surgery is often difficult. Furthermore, inadequate analgesia and/or an uninhibited stress response during the immediate postoperative period may increase morbidity by causing adverse hemodynamic, metabolic, immunologic, and hemostatic alterations (4,5,6). Aggressive control of postoperative pain, associated with an attenuated stress response, may decrease morbidity and mortality not only in high-risk patients following noncardiac surgery (7,8) and may also decrease morbidity and mortality in patients following cardiac surgery (9,10). Adequate postoperative analgesia following cardiovascular surgery may be attained via a wide variety of techniques (Table 22-1). Choice of technique is substantially influenced by type of surgery performed (i.e., cardiac surgery, thoracoabdominal aortic reconstruction, lower extremity revascularization). Traditionally, analgesia following cardiovascular surgery has been obtained mainly with IV (IV) opioids (specifically morphine), and this technique remains quite popular. However, IV opioid use is associated with definite detrimental side effects (nausea/vomiting, pruritus, urinary retention, respiratory depression), and longer-acting opioids such as morphine may delay tracheal extubation during the immediate postoperative period because of excessive sedation and/or respiratory depression. Thus, in the current era of early extubation (“fast-tracking”) following all types of surgeries, cardiovascular anesthesiologists are exploring unique options other than traditional IV opioids for control of postoperative pain in patients following all types of cardiovascular surgery (11,12). No single analgesic technique is clearly superior; each possesses distinct advantages and disadvantages. It is becoming increasingly clear that a multimodal approach/combined analgesic regimen (utilizing a variety of techniques) is likely the best way to approach postoperative pain to maximize analgesia and minimize side effects. When addressing postoperative analgesia and appropriateness of neural blockade techniques in cardiovascular surgical patients, choice of technique(s) is made only after a thorough analysis of the risk-benefit ratio of each technique in each specific patient in whom analgesia is desired. This chapter focuses on the clinical applications (advantages and disadvantages) of neural blockade techniques in patients undergoing cardiovascular surgery.
Clinical Applications for Cardiac Surgery
Pain following cardiac surgery may be intense and originates from many sources, including the incision (sternotomy, thoracotomy, etc.), intraoperative tissue retraction and dissection, vascular cannulation sites, vein harvesting sites, and chest tubes, among others (13,14). Patients in whom an internal mammary artery is surgically exposed and used as a bypass graft may have substantially more postoperative pain (15). A recently published prospective clinical investigation involving 200 consecutive patients undergoing cardiac surgery via median sternotomy assessed the location, distribution, and intensity of postoperative pain (13). All patients received 25 to 50 μg/kg of intraoperative IV fentanyl, were subjected to routine cardiopulmonary bypass, had their arms positioned along their body on the operating table, had their sternum closed with five peristernal wires, and received mediastinal and thoracic drains passed through the rectus abdominis muscle just below the xiphoid. A subgroup (127 patients) also underwent long
saphenous vein harvesting either from the calf (men) or thigh (women). All patients were extubated before the first postoperative morning. Postoperative analgesic management was standardized and included IV morphine, oral paracetamol, oral tramadol, and subcutaneous morphine. The investigators found that maximal pain intensity was highest on the first postoperative day and lowest on the third postoperative day. However, maximal pain intensity was only graded as “moderate” (mean pain score was approximately 3.8 on a 0-10 scale), did not diminish during the first two postoperative days, then started to decline between postoperative day 2 and 3. Pain distribution did not appear to vary throughout the postoperative period, yet location did (more shoulder pain observed on the seventh postoperative day). As time from operation increased, pain usually moved from primarily incisional/epigastric to osteoarticular. Another source of postoperative pain in patients following cardiac surgery is thoracic cage rib fractures, which may be common (16,17). Furthermore, sternal retraction, causing posterior rib fracture, may lead to brachial plexus injury. In these patients, routine chest radiographs may be normal despite the presence of fracture. Thus, bone scans (superior to chest radiographs in detecting rib fractures) are recommended whenever unexplained postoperative nonincisional pain occurs in a patient who has undergone sternal retraction (17). Other studies have indicated that the most common source of pain in patients following cardiac surgery is the chest wall. Age also appears to impact pain intensity; patients younger than 60 often have higher pain intensity than patients older than 60. Although maximal pain intensity following cardiac surgery is usually only moderate, improvement in analgesic control to minimize pain intensity, especially during the first few postoperative days, is warranted.
saphenous vein harvesting either from the calf (men) or thigh (women). All patients were extubated before the first postoperative morning. Postoperative analgesic management was standardized and included IV morphine, oral paracetamol, oral tramadol, and subcutaneous morphine. The investigators found that maximal pain intensity was highest on the first postoperative day and lowest on the third postoperative day. However, maximal pain intensity was only graded as “moderate” (mean pain score was approximately 3.8 on a 0-10 scale), did not diminish during the first two postoperative days, then started to decline between postoperative day 2 and 3. Pain distribution did not appear to vary throughout the postoperative period, yet location did (more shoulder pain observed on the seventh postoperative day). As time from operation increased, pain usually moved from primarily incisional/epigastric to osteoarticular. Another source of postoperative pain in patients following cardiac surgery is thoracic cage rib fractures, which may be common (16,17). Furthermore, sternal retraction, causing posterior rib fracture, may lead to brachial plexus injury. In these patients, routine chest radiographs may be normal despite the presence of fracture. Thus, bone scans (superior to chest radiographs in detecting rib fractures) are recommended whenever unexplained postoperative nonincisional pain occurs in a patient who has undergone sternal retraction (17). Other studies have indicated that the most common source of pain in patients following cardiac surgery is the chest wall. Age also appears to impact pain intensity; patients younger than 60 often have higher pain intensity than patients older than 60. Although maximal pain intensity following cardiac surgery is usually only moderate, improvement in analgesic control to minimize pain intensity, especially during the first few postoperative days, is warranted.
Table 22-1 Techniques available for postoperative analgesia | ||||||||
|---|---|---|---|---|---|---|---|---|
|
Persistent pain following cardiac surgery, while rare, can be problematic (18,19,20). The cause of persistent pain following sternotomy is multifactorial; tissue destruction, intercostal nerve trauma, scar formation, rib fractures, sternal infection, stainless-steel wire sutures, and/or costochondral separation may all play roles. Chronic pain is often localized to the arms, shoulders, or legs. Postoperative brachial plexopathies may also occur and have been attributed to rib fracture fragments, internal mammary artery dissection, suboptimal positioning of patients during surgery, and/or central venous catheter placement. Postoperative neuralgias of the saphenous nerve have also been reported following harvesting of saphenous veins for coronary artery bypass grafts (CABG). Younger patients appear to be at higher risk for developing chronic pain. The correlation of severity of acute postoperative pain and development of chronic pain syndromes has been suggested (patients requiring more postoperative analgesics may be more likely to develop chronic pain), yet the causative relationship is still vague. Ho and associates assessed via survey 244 patients following cardiac surgery and median sternotomy and found that persistent pain (defined as pain still present 2 or more months following surgery) was reported in almost 30% of patients (18). The incidence of persistent pain at any site was 29% (71 patients) and for sternotomy was 25% (61 patients). Other common locations of persistent pain reported to these investigators were the shoulders (17.4%), back (15.9%), and neck (5.8%). However, such persistent pain was usually reported as mild, with only 7% of patients reporting interference with daily living. The most common words used to describe the persistent pain were “annoying” (57%), “nagging” (33%), “dull” (30%), “sharp” (25%), “tiring” (22%), “tender” (22%), and “tight” (22%). The temporal nature of this pain was mostly reported as being brief/transient and periodic/intermittent. Twenty patients (8%) also described symptoms of numbness, burning pain, and tenderness over the internal mammary artery harvesting site, symptoms suggestive of internal mammary artery syndrome. Thus, Ho and associates conclude that mild persistent pain following cardiac surgery and median sternotomy is common, but infrequently interferes substantially with daily life.
Although the most common source of pain in patients following cardiac surgery remains the chest wall, leg pain from vein graft harvesting can be problematic as well. Such pain may not become apparent until the late postoperative period, which may be related to the progression of patient mobilization as well as the decreasing impact of sternotomy pain (unmasking leg incisional pain). The recent utilization of minimally invasive vein graft harvesting techniques (endoscopic vein graft harvesting) decreases postoperative leg pain intensity and duration compared to conventional open techniques (21). Furthermore, leg morbidity (infection, dehiscence, etc.) may be less in patients undergoing endoscopic vein harvest when compared to patients undergoing conventional open techniques, because of different incisional lengths.
Patient satisfaction with quality of postoperative analgesia (following any surgical procedure) is as much related to the comparison between anticipated pain and experienced pain as it is to the actual level of pain experienced. Patients undergoing cardiac surgery remain concerned regarding the adequacy of postoperative pain relief and tend to preoperatively expect a greater amount of postoperative pain than that which is actually experienced (14). Because of these unique preoperative expectations, patients following cardiac surgery who receive only moderate analgesia postoperatively will likely still be satisfied with their pain control. Thus, patients may experience pain of moderate intensity after cardiac surgery yet still express very high satisfaction levels (14,15).
Inadequate analgesia (coupled with an uninhibited stress response) during the postoperative period following cardiac surgery may lead to many adverse hemodynamic (tachycardia, hypertension, vasoconstriction), metabolic (increased catabolism), immunologic (impaired immune response), and hemostatic (platelet activation) alterations. In patients undergoing cardiac surgery, perioperative myocardial ischemia (diagnosed by electrocardiography [ECG] and/or transesophageal echocardiography [TEE]) is most commonly observed during the immediate postoperative period and appears to be related to outcome (22,23). Intraoperatively, initiation of cardiopulmonary bypass causes substantial increases in stress response hormones (norepinephrine, epinephrine, etc.) that persist into the immediate postoperative period and may also contribute to myocardial ischemia observed during this time (24,25,26). Furthermore, postoperative myocardial ischemia may be aggravated by cardiac sympathetic nerve activation, which disrupts
the balance between coronary blood flow and myocardial oxygen demand (27). Thus, during the pivotal immediate postoperative period after cardiac surgery, adequate analgesia (coupled with stress response attenuation) may potentially decrease morbidity and enhance health-related quality of life (27,28).
the balance between coronary blood flow and myocardial oxygen demand (27). Thus, during the pivotal immediate postoperative period after cardiac surgery, adequate analgesia (coupled with stress response attenuation) may potentially decrease morbidity and enhance health-related quality of life (27,28).
Evidence exists that aggressive control of postoperative pain in patients following cardiac surgery may beneficially affect outcome (9,10,29). Unfortunately, aggressive control of postoperative pain in patients following cardiac surgery through the use of relatively large amounts of IV opioids does not allow tracheal extubation to occur in the immediate postoperative period (a goal of current practice). Regional techniques may perhaps allow one to obtain intense postoperative analgesia while allowing early postoperative tracheal extubation.
Local Anesthetic Infiltration
Pain following cardiac surgery is often related to median sternotomy (peaking during the first 2 postoperative days). Because of problems associated with traditional IV opioid analgesia (nausea and vomiting, pruritus, urinary retention, respiratory depression) and the more recently introduced nonsteroidal antiinflammatory drugs (NSAIDs) and cyclooxygenase (COX) inhibitors (gastrointestinal bleeding, renal dysfunction), alternative methods of achieving postoperative analgesia in cardiac surgical patients have been sought. One alternative method is continuous infusion of local anesthetic in the sternotomy incision. In a prospective, randomized, placebo-controlled, double-blind clinical trial, White and associates studied 36 patients undergoing cardiac surgery (30). Intraoperative management was standardized. All patients had two indwelling infusion catheters placed at the median sternotomy incision site at the end of surgery (one in the subfascial plane above the sternum, one above the fascia in the subcutaneous tissue). Patients received either 0.25% bupivacaine (n = 12), 0.5% bupivacaine (n = 12), or normal saline (n = 12) via a constant rate infusion through the catheter (4 mL/hr) for 48 hours following surgery. Average times to tracheal extubation were similar in the three groups (approximately 5–6 hours). Compared with the control group (normal saline), there was a statistically significant reduction in verbal rating scale pain scores and IV patient-controlled morphine analgesia use in the 0.5% bupivacaine group. Patient satisfaction with their pain management was also improved in the 0.5% bupivacaine group versus saline control. However, there were no significant differences in patient-controlled morphine analgesia use between the 0.25% bupivacaine and control groups. Although tracheal extubation time and the duration of the intensive care unit stay (30 hours versus 34 hours, respectively) were not significantly altered, time to ambulation (1 day versus 2 days, respectively) and duration of hospital stay (4.2 days versus 5.7 days, respectively) were lower in the 0.5% bupivacaine group than in the control group. Serum bupivacaine concentrations in patients were reasonable. One complication related to the local anesthetic delivery system was encountered when a catheter tip was inadvertently broken off during its removal from the incision site, which required surgical reexploration of the wound under local anesthesia. The authors conclude that continuous infusion of 0.5% bupivacaine at 4 mL/hour is effective for decreasing postoperative pain and the need for postoperative supplemental opioid analgesic medication, as well as for improving patient satisfaction (earlier ambulation, reduced length of hospital stay) with pain management after cardiac surgery.
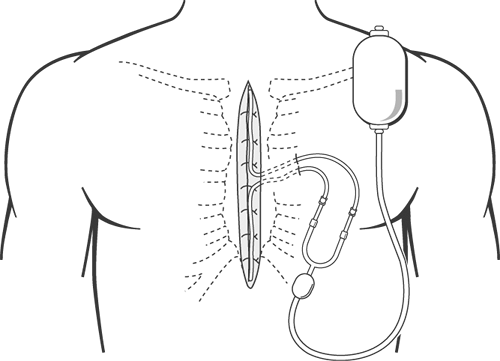
Another published clinical investigation reveals the potential benefits of using a continuous infusion of local anesthetic combined with intercostal nerve blocks in patients following cardiac surgery (31). In this prospective, randomized, placebo-controlled, double-blind clinical trial, Dowling and associates studied 35 healthy patients undergoing cardiac surgery (31). Patients undergoing elective CABG via median sternotomy were randomized to either ropivacaine or placebo groups. At the end of the operation, prior to wound closure, bilateral intercostal nerve injections from T1 to T12 were performed using 20 mL of either 0.2% ropivacaine or normal saline. After sternal reapproximation with wires, two catheters with multiple side openings were placed anterior to the sternum (Fig. 22-1). Infusions of 0.2% ropivacaine or normal saline at approximately 4 mL/hour for 48 hours were delivered through these catheters. Both groups exhibited similar postoperative extubation times (approximately 8 hours). Total mean patient-controlled morphine analgesia consumption during the immediate postoperative period (72 hours) was significantly decreased in the ropivacaine group when compared with the placebo group (47.3 mg versus 78.7 mg, respectively, p = 0.038). Mean overall pain scores (0–10 scale) were also significantly decreased in the ropivacaine group when compared with the placebo group (1.6 versus 2.6, respectively, p = 0.005). Most interestingly, patients receiving ropivacaine had a significantly shorter length of stay of 5.2 days ± 1.3 days compared with 8.2 days ± 7.9 days for patients receiving normal saline (p = 0.001). One patient in the placebo group had an extremely long postoperative hospitalization (39 days). However, the difference between the two groups regarding length of hospital stay remained statistically significant even if this outlier was removed (5.2 days ± 1.3 days versus 6.3 days ± 2.8 days, respectively, p <0.01). Despite differences in postoperative analgesia, postoperative pulmonary function (assessed via forced expiratory volume in 1 second and peak expiratory flow) was similar between the two groups. There was no difference in wound infections or wound healing between the two groups during hospitalization or after hospital discharge. No complications related to placement of the sternal wound catheters or performance of the intercostal nerve blocks were encountered. The significant decrease in hospital length of stay observed by the investigators is intriguing, may result in substantial cost reductions, and deserves further study.
The management of postoperative pain with continuous direct infusion of local anesthetic into the surgical wound has
been described following a wide variety of surgeries other than cardiac (inguinal hernia repair, upper abdominal surgery, laparoscopic nephrectomy, cholecystectomy, knee arthroplasty, shoulder surgery, and gynecologic operative laparoscopy) (32). The infusion pump systems used for anesthetic wound perfusion are regulated by the U.S. Food and Drug Administration (FDA) as medical devices. Thus, adverse events reported to the FDA include tissue necrosis, surgical wound infection, and cellulitis following orthopedic, gastrointestinal, podiatric, and other surgeries. None of these reported adverse events as of yet have involved patients undergoing cardiac surgery. The most commonly reported complication is tissue necrosis, an adverse event almost never seen following normal surgical procedures. Furthermore, consequences of these reported adverse events were typically severe and required intervention and additional medical and/or surgical treatment. Although these initial reports may be isolated incidents, they may also represent an early warning that is representative of a widespread problem. Nevertheless, these reports provide a potentially important signal, suggesting the need for further investigation into the relationship between use of these infusion pumps for direct continuous infusion of local anesthetics and other drugs into surgical wounds and the effect on tissue necrosis, serious infections, or cellulitis. Neither of the two clinical investigations involving local anesthetic infusion in patients following cardiac surgery with median sternotomy report such wound complications (30,31). Regardless, these safety issues merit careful consideration because of the importance of sternal wound complications in this setting.
been described following a wide variety of surgeries other than cardiac (inguinal hernia repair, upper abdominal surgery, laparoscopic nephrectomy, cholecystectomy, knee arthroplasty, shoulder surgery, and gynecologic operative laparoscopy) (32). The infusion pump systems used for anesthetic wound perfusion are regulated by the U.S. Food and Drug Administration (FDA) as medical devices. Thus, adverse events reported to the FDA include tissue necrosis, surgical wound infection, and cellulitis following orthopedic, gastrointestinal, podiatric, and other surgeries. None of these reported adverse events as of yet have involved patients undergoing cardiac surgery. The most commonly reported complication is tissue necrosis, an adverse event almost never seen following normal surgical procedures. Furthermore, consequences of these reported adverse events were typically severe and required intervention and additional medical and/or surgical treatment. Although these initial reports may be isolated incidents, they may also represent an early warning that is representative of a widespread problem. Nevertheless, these reports provide a potentially important signal, suggesting the need for further investigation into the relationship between use of these infusion pumps for direct continuous infusion of local anesthetics and other drugs into surgical wounds and the effect on tissue necrosis, serious infections, or cellulitis. Neither of the two clinical investigations involving local anesthetic infusion in patients following cardiac surgery with median sternotomy report such wound complications (30,31). Regardless, these safety issues merit careful consideration because of the importance of sternal wound complications in this setting.
Nerve Blocks
With the increasing popularity of minimally invasive cardiac surgery, which utilizes non sternotomy incisions (minithoracotomy), the use of nerve blocks in cardiac surgical patients has increased as well (33,34,35,36,37,38). Thoracotomy incisions (transverse anterolateral minithoracotomy, vertical anterolateral minithoracotomy), owing to trauma of the costal cartilage tissue, damage to ribs, tissue damage to muscles, and tissue damage to peripheral nerves, may induce more intense postoperative pain than median sternotomy. Adequate analgesia following thoracotomy is important because pain is a key component in alteration of lung function following thoracic surgery. Uncontrolled pain causes a reduction in respiratory mechanics, reduced mobility, and increases in hormonal and metabolic activity. Perioperative deterioration in respiratory mechanics may lead to pulmonary complications and hypoxemia, which may in turn lead to myocardial ischemia/infarction, cerebrovascular accidents, thromboembolism, and/or delayed wound healing, further leading to increased morbidity and prolonged hospital stay. Various analgesic techniques have been developed to treat postoperative thoracotomy pain. The most commonly utilized techniques include intercostal nerve blocks, intrapleural administration of local anesthetics, and thoracic paravertebral blocks.
Intercostal nerve block has been used extensively for analgesia following thoracic surgery (33,35). Intercostal nerve blocks can be performed either intraoperatively or postoperatively and usually provide sufficient analgesia lasting approximately 6 to 12 hours (depending on amount and type of local anesthetic utilized); these blocks may need to be repeated if additional analgesia is required. Local anesthetics may be administered as a single treatment under direction vision, before chest closure; as a single preoperative percutaneous injection; as multiple percutaneous serial injections; or via an indwelling intercostal catheter. Blockade of intercostal nerves interrupts C-fiber afferent transmission of impulses to the spinal cord. A single intercostal injection of a long-acting local anesthetic can provide pain relief and improve pulmonary function in patients following thoracic surgery for up to 6 hours. To achieve longer duration of analgesia, a continuous extrapleural intercostal nerve block technique may be used in which a catheter is placed percutaneously into an extrapleural pocket by the surgeon. A continuous intercostal catheter allows frequent dosing or infusions of local anesthetic agents and avoids multiple needle injections. Various clinical studies have confirmed the analgesic efficacy of this technique, and the technique compares favorably with thoracic epidural analgesic techniques (33). A major concern associated with intercostal nerve block is the potentially high amount of local anesthetic systemic absorption, yet multiple clinical studies involving patients undergoing thoracic surgery have documented safe blood levels with standard techniques. Clinical investigations involving patients undergoing thoracic surgery indicate that intercostal nerve blockade by intermittent or continuous infusion of 0.25% to 0.5% bupivacaine with epinephrine is an effective method for supplementing systemic IV opioid analgesia for postthoracotomy pain. The value of single preclosure injections remains doubtful.
Intrapleural administration of local anesthetics initiates analgesia via mechanisms that remain incompletely understood (33,35). However, the mechanism of action of extrapleural regional anesthesia seems to depend primarily on diffusion of the local anesthetic into the paravertebral region. Local anesthetic agents then affect not only the ventral nerve root but also afferent fibers of the posterior primary ramus. Posterior ligaments of the posterior primary ramus innervate posterior spinal muscles and skin and are traumatized during posterolateral thoracotomy. Intrapleural administration of local anesthetic agent to this region through a catheter inserted in the extrapleural space thus creates an anesthetic region in the skin. The depth and width of the anesthetic region depends on diffusion of the local anesthetic agent in the extrapleural space. With this technique, local anesthetics may be administered via an indwelling intrapleural catheter placed between the parietal and visceral pleura by intermittent or continuous infusion regimens. Systemic absorption of local anesthetic and toxicity are always a concern with this technique, but have not been substantiated in clinical studies that assayed plasma levels (33,35). A handful of clinical investigations involving patients undergoing thoracic surgery via thoracotomy incision suggest that 0.25% to 0.5% bupivacaine may improve analgesia in patients following thoracic surgery, yet its true efficacy as a postoperative analgesic in this patient population remains somewhat controversial (36). The analgesic benefits are of short duration, and there does not appear to be a significant overall opioid-sparing effect. Furthermore, the optimum concentration and duration remains to be defined. However, a recently published prospective, randomized clinical study involving 50 patients undergoing minimally invasive direct CABG (via minithoracotomy) reported that an intrapleural analgesic technique (using 0.25% bupivacaine) is safe and effective and compares favorably to a conventional thoracic epidural technique (37). However, careful catheter positioning, chest tube clamping, and anchoring of the catheter are mandatory for postoperative intrapleural analgesia to be effective. A major factor implicated in lack of efficacy regarding intrapleural techniques is loss of local anesthetic solution through intercostal chest drainage tubes. Although clamping the chest tubes during the postoperative period will increase analgesic efficacy, it may not be safe to clamp chest tubes, as they provide important drainage of hemorrhage and air and allow for enhanced lung patency and expansion.
Apart from proper catheter positioning (insertion of catheter under direct vision and anchoring catheter to skin is essential), effective analgesia with this technique also appears to depend on whether surgery to the lung was performed or whether the pleural anatomy and physiology are relatively intact.
Apart from proper catheter positioning (insertion of catheter under direct vision and anchoring catheter to skin is essential), effective analgesia with this technique also appears to depend on whether surgery to the lung was performed or whether the pleural anatomy and physiology are relatively intact.
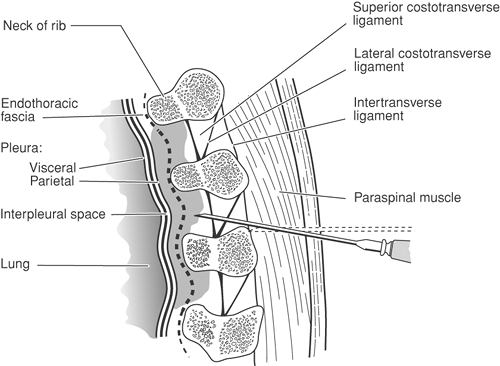 Figure 22-2. Sagittal section through the thoracic paravertebral space showing a needle that has been advanced above the transverse process. |
Thoracic paravertebral block involves injection of local anesthetic adjacent to the thoracic vertebrae, close to where the spinal nerves emerge from the intervertebral foramina (Fig. 22-2 and see Figs. 16-4, and 16-15,16-16,16-17). Thoracic paravertebral block, when compared to thoracic epidural analgesic techniques, provides equivalent analgesia, is technically easier, and may harbor less risk. Several different techniques exist for successful thoracic paravertebral block, and have recently been extensively reviewed (34) (Chapter 16). These blocks may be effective in alleviating acute and chronic pain of unilateral origin from the chest and/or abdomen. Unilateral paravertebral block is useful for attaining postthoracotomy analgesia, because pain following lateral thoracotomy is essentially always unilateral. The benefits of unilateral paravertebral blockade are a lesser incidence of adverse events (hypotension, urinary retention) and a decreased risk of systemic local anesthetic toxicity because less local anesthetic is used. The clinical investigations involving unilateral paravertebral block in patients undergoing thoracic surgery are few (33,35). Therefore, it is not possible to determine from the available literature whether the technique of paravertebral blockade (single injection) is truly useful in the postoperative analgesic management of patients following thoracotomy. Continuous thoracic paravertebral infusion of local anesthetic, placed under direct vision at thoracotomy or using a loss-of-resistance technique, is an effective method of providing analgesia following thoracotomy. Indeed, continuous thoracic paravertebral block, as part of a balanced analgesic regimen, may provide effective pain relief with very few side effects following thoracotomy and appears to be comparable to thoracic epidural analgesia (34). Bilateral use of thoracic paravertebral block has been described.
In summary, intercostal nerve blocks, intrapleural administration of local anesthetics, and thoracic paravertebral block offer the advantages of simplicity and efficacy in controlling postoperative pain in patients undergoing thoracic incisions for cardiac surgery. However, although the analgesic efficacy of these techniques sometimes is comparable to intrathecal techniques and epidural techniques, these techniques appear to work best as a part of a multimodal analgesic regimen. The patient must be observed for complications associated with infiltrations of large quantities of local anesthetic when utilizing these analgesic techniques.
Intrathecal and Epidural Techniques
Intrathecal and/or epidural techniques, utilizing opioids and/or local anesthetics, initiate reliable postoperative analgesia in patients following cardiac surgery (39). Additional potential advantages of using intrathecal and/or epidural techniques in patients undergoing cardiac surgery include stress response attenuation and thoracic cardiac sympathectomy. Intrathecal or epidural anesthesia and analgesia (with local anesthetics or opioids) can effectively inhibit the stress response associated with surgical procedures (27). Local anesthetics appear to possess greater efficacy than opioids in perioperative stress response attenuation, perhaps because of their unique mechanism of action. Although still a matter of some debate, perioperative stress response attenuation with epidural local anesthetics and/or opioids in high-risk patients after major noncardiac surgery may potentially decrease morbidity and mortality (7,8,27). Unfortunately, to achieve perioperative stress response attenuation in patients undergoing cardiac surgery using IV opioids in this manner does not allow tracheal extubation to occur in the immediate postoperative period. Intrathecal or epidural anesthesia and analgesia techniques (particularly with local anesthetics) are attractive alternatives because of their potential to attenuate the perioperative stress response yet still allow tracheal extubation to occur in the immediate postoperative period.
The myocardium and coronary vasculature are densely innervated by sympathetic nerve fibers that arise from T1 to T5 and profoundly influence total coronary blood flow and distribution (40). Cardiac sympathetic nerve activation initiates coronary artery vasoconstriction (41) and paradoxical coronary vasoconstriction in response to intrinsic vasodilators (42). In patients with coronary artery disease, cardiac sympathetic
nerve activation disrupts the normal matching of coronary blood flow and myocardial oxygen demand (43,44). Animal models have revealed an intense poststenotic coronary vasoconstrictive mechanism mediated by cardiac sympathetic nerve activation that attenuates local metabolic coronary vasodilation in response to myocardial ischemia (45,46). Furthermore, myocardial ischemia initiates a cardiocardiac reflex mediated by sympathetic nerve fibers, which augments the ischemic process (47). Cardiac sympathetic nerve activation likely plays a central role in initiating postoperative myocardial ischemia by decreasing myocardial oxygen supply via these mechanisms (27,48).
nerve activation disrupts the normal matching of coronary blood flow and myocardial oxygen demand (43,44). Animal models have revealed an intense poststenotic coronary vasoconstrictive mechanism mediated by cardiac sympathetic nerve activation that attenuates local metabolic coronary vasodilation in response to myocardial ischemia (45,46). Furthermore, myocardial ischemia initiates a cardiocardiac reflex mediated by sympathetic nerve fibers, which augments the ischemic process (47). Cardiac sympathetic nerve activation likely plays a central role in initiating postoperative myocardial ischemia by decreasing myocardial oxygen supply via these mechanisms (27,48).
Thoracic epidural anesthesia with local anesthetics effectively blocks cardiac sympathetic nerve afferent and efferent fibers, whereas epidural opioids are unable to effectively block such cardiac sympathetic nerve activity (27). Patients with symptomatic coronary artery disease benefit clinically from cardiac sympathectomy; the application of thoracic sympathetic blockade in the management of angina pectoris was described as early as 1965 (49). Thoracic epidural anesthesia with local anesthetics increases the diameter of stenotic epicardial coronary artery segments without causing dilation of coronary arterioles (43), decreases determinants of myocardial oxygen demand (44), improves left ventricular function (50), and decreases anginal symptoms (44,51). Furthermore, cardiac sympathectomy increases the endocardial-to-epicardial blood flow ratio (52,53), beneficially affects collateral blood flow during myocardial ischemia (53), decreases poststenotic coronary vasoconstriction (46), and attenuates the myocardial ischemia-induced cardiocardiac reflex (46). In an animal model, thoracic epidural anesthesia with local anesthetics actually decreased myocardial infarct size following coronary artery occlusion (52). Of note, these beneficial effects are not caused by systemic absorption of the local anesthetic (52). In short, thoracic epidural anesthesia with local anesthetics may benefit patients undergoing cardiac surgery by effectively blocking cardiac sympathetic nerve activity and improving the myocardial oxygen supply-demand balance.
Intrathecal Techniques
Application of intrathecal analgesia to patients undergoing cardiac surgery was initially reported by Mathews and Abrams in 1980 (54). They described the administration of intrathecal morphine (1.5–4.0 mg) to 40 adults after the induction of general anesthesia for cardiac surgery. Somewhat remarkably, all 40 patients awakened pain-free at the end of surgery (prior to leaving the operating room) and 36 patients were tracheally extubated prior to transfer to the intensive are unit. Postoperatively, all 40 patients were entirely pain-free for the first 27.5 postoperative hours, and 17 did not require any supplemental analgesics prior to discharge from the hospital. Mathews and Abrams summarize: “The benefits of recovering from surgery free from pain have been impressive. This has been particularly appreciated by patients who have had previous operations with conventional anaesthesia and postoperative analgesic drugs. The patients have been remarkably comfortable, able to move more easily in bed, and more cooperative, thus greatly helping their nursing care” (54). After this impressive clinical display, other investigators have subsequently applied intrathecal anesthesia and analgesia techniques to patients undergoing cardiac surgery (55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83). Most clinical investigators have used intrathecal morphine to provide prolonged postoperative analgesia, although some clinical investigators have used intrathecal fentanyl, sufentanil, and/or local anesthetics. A recently published anonymous survey of members of the Society of Cardiovascular Anesthesiologists indicates that almost 8% of practicing anesthesiologists incorporate intrathecal techniques into their anesthetic management of adults undergoing cardiac surgery (83). Of these anesthesiologists, 75% practice in the United States, 72% perform the intrathecal injection prior to induction of anesthesia, 97% utilize morphine, 13% utilize fentanyl, 2% utilize sufentanil, 10% utilize lidocaine, and 3% utilize tetracaine (83).
Intrathecal Analgesia and Tracheal Extubation
Two randomized, blinded, placebo-controlled clinical studies revealed the ability of intrathecal morphine to induce significant postoperative analgesia following cardiac surgery (69,76). In 1988, Vanstrum and associates prospectively randomized 30 patients to receive either intrathecal morphine (0.5 mg) or intrathecal placebo prior to induction of anesthesia (76). Intraoperative anesthetic management was standardized, and all patients postoperatively received exclusively IV morphine administered by a nurse who attempted to keep the linear analog pain score at less than four (1–10 scale). Although pain scores between groups were not significantly different at any postoperative time interval tested, patients who received intrathecal morphine required significantly less IV morphine than placebo controls (2.4 mg versus 8.3 mg, respectively, p <0.02) during the initial 30 hours following intrathecal injection. Associated with this enhanced analgesia in patients receiving intrathecal morphine was a substantially decreased need for antihypertensive medications (sodium nitroprusside, nitroglycerine, hydralazine) during the immediate postoperative period. Time to tracheal extubation (approximately 20 hours) and postoperative arterial blood gas tensions following anesthesia were not significantly affected by the use of intrathecal morphine. In 1996, Chaney and associates prospectively randomized 60 patients to receive either intrathecal morphine (4.0 mg) or intrathecal placebo prior to induction of anesthesia for elective CABG (69). Intraoperative anesthetic management was standardized and, after tracheal extubation, all patients received exclusively IV morphine via patient-controlled analgesia (PCA). The mean time from intensive care unit arrival to tracheal extubation was similar in all patients (approximately 20 hours). However, patients who received intrathecal morphine required significantly less IV morphine than placebo controls (33.2 mg versus 51.1 mg, respectively, p <0.05) during the initial postoperative period. Despite enhanced analgesia, no clinical differences between groups existed regarding postoperative morbidity (pruritus, nausea, vomiting, urinary retention, prolonged somnolence, atrial fibrillation, ventricular tachycardia, myocardial infarction, cerebral infarction), mortality, nor duration of postoperative hospital stay (approximately 9 days in each group).
The mid 1990s saw the emergence of fast-track cardiac surgery, with the goal being tracheal extubation in the immediate postoperative period. Chaney and associates, in 1997, were the first to study the potential clinical benefits of intrathecal morphine when used in patients undergoing cardiac surgery and early tracheal extubation (68). They prospectively randomized 40 patients to receive either intrathecal morphine (10 μg/kg) or intrathecal placebo prior to induction of anesthesia for elective CABG. Intraoperative anesthetic management was standardized (IV fentanyl, 20 μg/kg, and IV midazolam, 10 mg) and all patients postoperatively received exclusively IV morphine via PCA. Of the patients who were tracheally extubated during the immediate postoperative period, the mean
time from intensive care unit arrival to tracheal extubation was significantly prolonged in those who received intrathecal morphine (10.9 hours ± 4.4 hours; p = 0.02) when compared to placebo controls (7.6 hours ± 2.5 hours). Three patients who received intrathecal morphine had tracheal extubation substantially delayed (12–24 hours) because of prolonged ventilatory depression, likely secondary to intrathecal morphine. No clinical differences existed between groups regarding IV morphine use for 48 hours, postoperative morbidity, mortality, nor duration of postoperative hospital stay (approximately 9 days in each group).
time from intensive care unit arrival to tracheal extubation was significantly prolonged in those who received intrathecal morphine (10.9 hours ± 4.4 hours; p = 0.02) when compared to placebo controls (7.6 hours ± 2.5 hours). Three patients who received intrathecal morphine had tracheal extubation substantially delayed (12–24 hours) because of prolonged ventilatory depression, likely secondary to intrathecal morphine. No clinical differences existed between groups regarding IV morphine use for 48 hours, postoperative morbidity, mortality, nor duration of postoperative hospital stay (approximately 9 days in each group).
These somewhat discouraging findings (absence of enhanced analgesia, prolongation of tracheal extubation time) stimulated the same group of investigators, in 1999, to repeat the study, but decrease intraoperative IV fentanyl administration to 10 μg/kg (66). Of the patients tracheally extubated during the immediate postoperative period, mean time to tracheal extubation was similar in patients who received intrathecal morphine (6.8 hours ± 2.8 hours) when compared to intrathecal placebo patients (6.5 hours ± 3.2 hours). However, once again, four (10%) patients who received intrathecal morphine had tracheal extubation substantially delayed (14 hours, 14 hours, 18 hours, 19 hours) because of prolonged respiratory depression (likely secondary to intrathecal morphine). No clinical differences existed between groups regarding postoperative morbidity, mortality, nor duration of postoperative hospital stay (approximately 6 days in each group). Based on these three prospective, randomized, double-blind, placebo-controlled clinical investigations, the authors concluded that, although intrathecal morphine certainly can initiate reliable postoperative analgesia, its use in the setting of fast-track cardiac surgery and early tracheal extubation may be detrimental by potentially delaying tracheal extubation in the immediate postoperative period.
Since this time, however, other clinical investigators have revealed that certain combinations of intraoperative anesthetic technique, coupled with appropriate doses of intrathecal morphine, will allow both tracheal extubation following cardiac surgery within the immediate postoperative period along with enhanced analgesia (58). Importantly, limiting the amounts of intraoperative IV opioids and IV sedatives and the application of a postoperative tracheal extubation protocol may be more important in achieving the goal of early tracheal extubation following cardiac surgery than adequate pain control during the immediate postoperative period.
Many other suboptimally designed clinical investigations attest to the ability of intrathecal morphine to induce substantial postoperative analgesia in patients following cardiac surgery (Table 22-2). Intrathecal doses of 0.5 to 10.0 mg administered prior to cardiopulmonary bypass initiate reliable postoperative analgesia, the quality of which depends not only on the intrathecal dose administered but also on the type and amount of IV analgesics and sedatives used for the intraoperative baseline anesthetic. The optimal dose of intrathecal morphine for achieving the maximum postoperative analgesia with minimum undesirable drug effects is uncertain. Naturally, when larger doses of intrathecal morphine are used, more intense and prolonged postoperative analgesia is purchased at the expense of more undesirable side effects, including nausea and vomiting, pruritus, urinary retention, and respiratory depression.
Attenuation of Stress Response
Because of morphine’s low lipid solubility, analgesic effects following intrathecal injection are delayed. Thus, even large doses of intrathecal morphine administered to patients prior to cardiac surgery will not initiate reliable intraoperative analgesia (76,77,78,81) and therefore would not be expected to potentially attenuate the intraoperative stress response associated with cardiopulmonary bypass. Only an extremely large dose of intrathecal morphine (10.0 mg) may initiate reliable intraoperative analgesia (80). A single clinical investigation has examined the ability of intrathecal morphine to potentially attenuate the intraoperative stress response associated with cardiopulmonary bypass as measured by blood catecholamine levels (69). In this clinical investigation by Chaney and associates, patients were prospectively randomized to receive either intrathecal morphine (4.0 mg) or intrathecal placebo prior to induction of anesthesia for elective CABG with cardiopulmonary bypass. Intraoperative anesthetic management was standardized, and multiple arterial blood samples were obtained perioperatively to ascertain norepinephrine and epinephrine levels. Patients who were administered intrathecal morphine experienced similar perioperative increases in blood catecholamine levels when compared with placebo controls. Thus, it appears that intrathecal morphine (even in relatively large doses) is unable to reliably attenuate the perioperative stress response associated with cardiac surgery and cardiopulmonary bypass.
However, although unable to reliably attenuate the perioperative stress response associated with cardiopulmonary bypass, intrathecal morphine (by initiating postoperative analgesia) may potentially attenuate the stress response during the immediate postoperative period (76). Vanstrum and associates revealed that patients who were administered 0.5 mg of intrathecal morphine prior to the induction of anesthesia not only required significantly less IV morphine postoperatively when compared to placebo controls but also required significantly less IV nitroprusside (58.1 mg versus 89.1 mg, respectively, p <0.05) during the initial 24 postoperative hours to control hypertension, suggesting partial postoperative stress response attenuation.
Intrathecal fentanyl, sufentanil, and/or local anesthetics have been used in patients undergoing cardiac surgery, hoping to provide intraoperative anesthesia and analgesia (and stress response attenuation), with mixed results (Table 22-2). Intrathecal sufentanil (50 μg), administered prior to the induction of anesthesia for cardiac surgery can reduce volatile anesthetic requirements during mediastinal dissection but is unable to reliably block intraoperative hemodynamic responses to laryngoscopy and intubation (73).
Hemodynamic Effects of Intrathecal Local Anesthetics
Administration of intrathecal local anesthetics to patients after the induction of anesthesia for cardiac surgery may help promote intraoperative hemodynamic stability (70,72).
In 1994, in a retrospective review, 18 adult patients were administered lumbar intrathecal hyperbaric bupivacaine (23–30 mg) and/or hyperbaric lidocaine (150 mg) mixed with morphine (0.5–1.0 mg) following the induction of anesthesia (72). In an attempt to produce a “total spinal” and, thus, thoracic cardiac sympathectomy, the Trendelenburg position was maintained for at least 10 minutes following intrathecal injection. Heart rate decreased significantly (baseline mean 67 bpm to postinjection mean 52 bpm) after the intrathecal injection (indicating cardiac sympathectomy was obtained) and not a single patient exhibited ECG evidence of myocardial ischemia prior to cardiopulmonary bypass. Although these authors report that
the technique provided stable perioperative hemodynamics, 17 of 18 patients required IV phenylephrine at some time intraoperatively to increase blood pressure. In 1996, the same group of investigators reported similar hemodynamic changes in a case report involving a 10-year-old child with Kawasaki disease who underwent CABG and receiving intrathecal hyperbaric bupivacaine mixed with morphine via a lumbar puncture following induction of anesthesia (70).
the technique provided stable perioperative hemodynamics, 17 of 18 patients required IV phenylephrine at some time intraoperatively to increase blood pressure. In 1996, the same group of investigators reported similar hemodynamic changes in a case report involving a 10-year-old child with Kawasaki disease who underwent CABG and receiving intrathecal hyperbaric bupivacaine mixed with morphine via a lumbar puncture following induction of anesthesia (70).
Table 22-2 Reports of intrathecal anesthesia and analgesia for cardiac surgery | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
A recently published, small (n = 38 patients), prospective, randomized, blinded clinical investigation reveals that large doses of intrathecal bupivacaine (37.5 mg) administered to patients immediately prior to induction of general anesthesia (19 patients received intrathecal bupivacaine, 19 patients served as controls) for elective CABG may potentially initiate intraoperative stress response attenuation (assessed via serum mediator levels, hemodynamics, and qualitative/quantitative alterations in myocardial β-receptors) (84). However, no effect on real clinical outcome parameters (i.e., tracheal extubation times, respiratory function, perioperative spirometry) was observed. Mean tracheal extubation times (measured from the time of sternotomy dressing application) were extremely short in both groups (11–19 minutes). Postoperative pain scores and morphine use via PCA did not differ between the two groups. Not surprisingly, phenylephrine use was more common in patients who received intrathecal bupivacaine when compared to control patients.
In summary, the many clinical investigations involving the use of intrathecal analgesic techniques in patients undergoing cardiac surgery indicate that the administration of intrathecal morphine to patients prior to cardiopulmonary bypass initiates reliable postoperative analgesia following cardiac surgery. Intrathecal opioids or local anesthetics cannot reliably attenuate the perioperative stress response associated with cardiopulmonary bypass that persists during the immediate postoperative period. Although intrathecal local anesthetics (not opioids) may induce perioperative thoracic cardiac sympathectomy, the hemodynamic changes associated with a “total spinal” makes the technique unsuitable for patients with cardiac disease.
Epidural Techniques
Thoracic epidural anesthesia and analgesia with local anesthetics and/or opioids induces significant postoperative analgesia in patients undergoing cardiac procedures. A recently published anonymous survey of members of the Society of Cardiovascular Anesthesiologists indicates that 7% of practicing anesthesiologists incorporate thoracic epidural techniques into their anesthetic management of adults undergoing cardiac surgery (83). Of these anesthesiologists, 58% practice in the United States. Regarding the timing of epidural instrumentation, 40% perform instrumentation before induction of general anesthesia, 12% perform instrumentation following induction of general anesthesia, 33% perform instrumentation at the end of surgery, and 15% perform instrumentation on the first postoperative day (83).
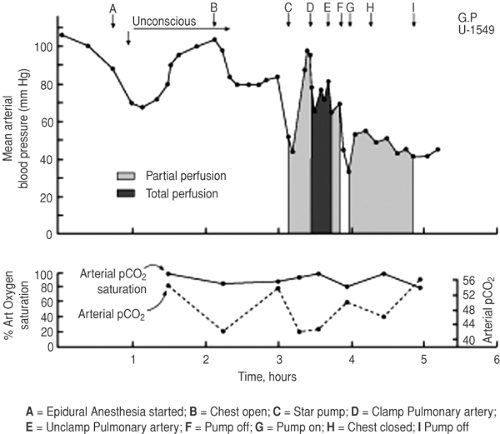 Figure 22-3. Graph of clinical course of initial cardiac patient receiving presurgical epidural anesthesia in 1954. From Clowes et al. (85). |
The initial description of thoracic epidural anesthesia and analgesia applied to a cardiac surgical patient occurred in 1954 (85). Clowes and associates describe their presurgical anesthetic technique in a 55-year-old man with severe cardiac failure: “An endotracheal tube was passed with topical anesthesia. Under extradural block of the upper thorax, hypotension developed but responded to the administration of a vasopressor drug. At this time the patient became comatose” (Fig. 22-3) (85). The patient eventually expired. Application of thoracic epidural anesthesia and analgesia to patients undergoing cardiac surgery during the modern surgical era was initially reported by Hoar and associates in 1976 (86). They described the intraoperative insertion of thoracic epidural catheters in 12 patients following CABG (after IV protamine, prior to transfer to intensive care unit). The epidural catheters were injected with lidocaine and bupivacaine during the immediate postoperative period to promote analgesia and effectively control hypertension. Administration of epidural local anesthetics to these patients significantly decreased postoperative blood pressure in hypertensive and normotensive patients; not a single patient required cardiac or peripheral vascular stimulants during the immediate postoperative study period.
The 1987 report by El-Baz and Goldin was the first to describe the insertion of thoracic epidural catheters in patients prior to cardiac surgery and also involved epidural opioids, rather than local anesthetics (87). In prospective, randomized fashion, patients undergoing elective CABG received either routine treatment for postoperative pain (n = 30 patients, IV morphine) or a continuous infusion of morphine (0.1 mg/hr) via a thoracic epidural catheter (n = 30 patients). Thoracic epidural catheters were inserted at T3–T4 immediately prior to induction of anesthesia on the day of surgery. Intraoperative anesthetic technique was standardized; mean postoperative tracheal extubation time was significantly shorter in patients receiving thoracic epidural anesthesia when compared to control patients (9 ± 3 hours versus 18 ± 5 hours, respectively, p <0.01). Continuous thoracic epidural infusion of morphine also achieved better postoperative pain relief in patients than IV morphine (significantly better pain scores, significantly less supplemental IV morphine). Furthermore, in a subgroup of 20 patients (10 per group), postoperative “stress” was assessed via serum cortisol and β-endorphin levels. Patients receiving thoracic epidural anesthesia had significantly lower postoperative levels of these mediators when compared to control patients, indicating potential postoperative stress response attenuation. Continuous thoracic epidural infusion of morphine (when compared to controls) was also associated with a lower incidence of opioid-related side effects during the immediate postoperative period. The insertion of the thoracic epidural catheter immediately prior to systemic heparin administration was not associated with any neurologic problems.
Since this initial report of potential benefits (reliable postoperative analgesia, stress response attenuation, facilitation of early tracheal extubation), others clinical investigators have subsequently applied thoracic epidural anesthesia and analgesia to patients undergoing cardiac surgery (88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123) (Table 22-3). For example, patients randomized to receive intermittent boluses of thoracic epidural infusion intraoperatively, followed by continuous infusion postoperatively, exhibited significantly decreased blood levels of norepinephrine and epinephrine (98,101) and cortisol (98) perioperatively when compared with patients managed similarly without thoracic epidural catheters (101). Furthermore, increased blood catecholamine levels in these patients were associated with increased systemic vascular resistance (101). Continuous thoracic epidural bupivacaine and sufentanil infusion administered perioperatively significantly decreased blood levels of norepinephrine following sternotomy when compared to conventional analgesic methods (104). Other clinical studies further attest to the ability of thoracic epidural anesthesia with
local anesthetics to promote perioperative hemodynamic stability in patients undergoing cardiac surgery, which suggests perioperative stress response attenuation (86,100,101,104).
local anesthetics to promote perioperative hemodynamic stability in patients undergoing cardiac surgery, which suggests perioperative stress response attenuation (86,100,101,104).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree