Fig. 30.1
Gasserian ganglion block. Three-dimensional CT-view constructed after the needle (yellow) tip was advanced through the foramen ovale (Image reprinted with permission from Springer. The image was originally published in Koizuka et al. (2009), Figure 3)
Sphenopalatine Ganglion Block
Anatomy: The sphenopalatine ganglion that is also known as the pterygopalatine ganglion resides in the pterygopalatine fossa, along with the maxillary artery and its branches (Erdine 2008; Moore et al. 2010). It is just behind the middle turbinate and below a depth of 1–1.5 mm mucosa/soft tissue (Windsor and Jahnke 2004). It contains both sensory and autonomic neuronal components (Erdine 2008; Moore et al. 2010; Windsor and Jahnke 2004). The sensory nerves, that innervate the nasal membranes, the soft palate, and parts of the pharynx, pass through the ganglion and join the maxillary nerve just above the ganglion. Postganglionic sympathetic fibers pass through the ganglion and innervate the lacrimal gland and the nasal and palatine mucosa. Preganglionic parasympathtic fibers originate from the superior salivatory nucleus, travel with the facial nerve, the greater petrosal nerve and the vidian nerve, and synapse on their postganglionic cells in the ganglion. The postganglionic parasympathetic fibers innervate the nasal, paranasal sinus mucosa, and lacrimal gland.
Indications: Sphenopalatine neuralgia, trigeminal neuralgia, cluster headache, migraine, and atypical facial pain (Erdine 2008).
Block technique: There are three approaches namely transnasal, transoral, and lateral to block the sphenopalatine ganglion using local anesthetic (Tsui et al. 2009). Among these, the transnasal approach produces least patient discomfort. The patient is placed supine with monitors for vital signs and cardiac rhythm attached (Erdine 2008; Windsor and Jahnke 2004). To facilitate the insertion of a cotton-tip to the pterygopalatine fossa, the nasal mucosa is anesthetized with 2% viscous lidocaine. The cotton-tip that has been soaked with a local anesthetic, such as 4% lidocaine is slowly advanced to the posterior wall of the nasopharynx along the superior border of the middle turbinate. The cotton-tip is left in place for 20–45 min. An intravenous infusion tube can be slid over the cotton stick and attached to a syringe to allow for more precise instillation of local anesthetic (Windsor and Jahnke 2004). Pain reduction is short lived and periodic repetition of the procedure is common in order to maintain a sustained response (Erdine 2008). Longer pain relief for months to years has been reported after either pulsed radiofrequency or thermal radiofrequency treatment of the sphenopalatine ganglion.
Intercostal Nerve Block
Anatomy: There are 11 pairs of intercostal nerves derived from the anterior rami of thoracic spinal nerve T1–T11 (Gundamraj and Richeimer 2010). Each intercostal nerve has four branches, the white and gray sympathetic rami communicates, the lateral cutaneous branches and the anterior cutaneous branches (Brown 2006f). The lateral and anterior cutaneous branches along with posterior cutaneous branch from the posterior rami, collectively, provide innervation to the skin and muscles of the chest wall and abdomen. The intercostal nerves run inferior to the intercostal vein and artery as a neurovascular bundle. The common sites of needle entry for intercostal nerve block are the posterior angle of a rib and the posterior axillary line where the intercostal nerve is between the innermost intercostal muscle and internal intercostal muscle and in the intercostal groove (Brown 2006f; Nachi et al. 2008).
Indications: Relief of chest wall pain associated with surgery (i.e., thoracic and breast surgeries), tumor invasion, rib fracture, and postherpetic neuralgia (Gundamraj and Richeimer 2010; Nachi et al. 2008; Burton et al. 2009).
Block technique (Brown 2006f; Nachi et al. 2008; Waldman 2008): A patient is placed in a prone or seated or lateral position. Needle entry site is either the posterior angle of the rib or posterior or mid-axillary line at the level of the intercostal nerve corresponding to the location of the pain. The skin is prepared and draped according to usual sterile technique. Conscious sedation may be provided especially if blocks are placed in multiple intercostal levels. After infiltration of the skin and subcutaneous tissue with fast-acting local anesthetics such as lidocaine, a 22- or 25-gauge, 1½-in., short-beveled needle is inserted at the inferior edge of the rib until it reaches the bone. The needle is then walked off the rib into the intercostal grove. After negative aspiration for blood and air, 3–5 mL of local anesthetic is injected. The block can be performed under the guidance of fluoroscopy (Waldman 2008) or ultrasound (Harmon and Shorten 2009). To provide a longer duration of pain reduction, a neurolytic solution such as 10% phenol can be injected (Burton et al. 2009).
Lateral Femoral Cutaneous Nerve Block
Anatomy: The lateral femoral cutaneous nerve derives from the L2 and L3 spinal nerves (Enneking et al. 2009). It is a pure sensory nerve supplying the lateral aspect of the thigh from the ilioinguinal ligament to the knee. It emerges from the psoas muscle laterally, advancing between the iliac muscle and fascia, passing below the inguinal ligament and medial to the anterior superior iliac spine into the thigh. It is initially beneath the fascial lata, but pierces it about 7–9 cm from the anterior superior iliac spine and splits into anterior and posterior branches.
Indications: This block is a diagnostic tool for meralgia paresthetica and may also provide therapeutic value (Harney and Patijn 2007). It can also be used for analgesia during biopsy or skin graft harvesting (Enneking et al. 2009).
Block technique (Waldman 2008; Harney and Patijn 2007; Brown 2006g; Hadzic and Vloka 2004): To perform a lateral femoral cutaneous nerve block, one first identifies the anterior superior iliac spine. The needle entry point is approximately 2 cm medial to this landmark and just below the inguinal ligament. This block can be carried out using a 22–25-G 1½-in. needle. It is recommended using a needle with a short bevel to enhance the sensation of a “pop” when the needle passes through the fascia lata. Commonly injected anesthetics are 0.2–0.5% Ropivacaine or 0.25–0.5% bupivacaine or 1% lidocaine. The drug should be injected in a fanlike fashion as well above and below the fascia lata. If the procedure is carried out without a nerve stimulator or ultrasound guidance, an injection volume of around 10 mL is recommended due to the anatomical variation of the nerve as it emerges under the inguinal ligament.
Ilioinguinal/Iliohypogastrick Nerve Block
Anatomy: The iliohypogastric nerve derives from the T12 and L1 spinal nerves. It controls the motor function of the internal and external oblique muscles as well as the transverse abdominis at the anterior inferior abdominal wall (Enneking et al. 2009). It contains sensory innervation for the inferior abdominal wall and the upper lateral quadrant of buttock.
The ilioinguinal nerve derives from the L1 spinal nerve (Enneking et al. 2009). It controls the motor function of the internal oblique muscle and provides sensory innervation for inferior to medial aspect of the inguinal ligament. After leaving the lumbar plexus in the psoas muscle, the iliohypogasstric and ilioinguinal nerves extend laterally along the posterior lateral abdominal wall and in front of quadratus lumborum (Netter 1989). They then pierce the transverse abdominis, internal oblique and external oblique muscles while continuing to extend anteromedially in the anterior abdominal wall. At or near the anterior superior iliac spine, the iliohypogastric nerve lies between the internal and external oblique muscles, whereas the ilioinguinal nerve is between the transverse abdominis and internal oblique muscles. The ilioinguinal nerve pieces the internal oblique muscle at a more medial location in the anterior abdominal wall (Harmon and Shorten 2009).
Indications: Diagnosis and treatment of inguinal and suprapubic pain after inguinal hernia repair or lower abdominal surgery (Molloy and Benzon 2008).
Block technique (Waldman 2008; Harmon and Shorten 2009; Brown 2006h): To perform an ilioinguinal/iliohypogastric nerve block, one identifies the anterior superior iliac crest. According to different text books, the needle entry point is 1 cm (Harmon and Shorten 2009), or 3 cm (Brown 2006h), or 2 in. (Waldman 2008) medial and inferior to this landmark. Local anesthetic is then deposited between the internal oblique and external oblique muscles as well as between the transverse abdominis and internal oblique muscles. To improve block accuracy and success, the procedure can be carried out using ultrasonography that allows direct visualization of the fascia planes and nerves (Peng and Tumber 2008). Ultrasound guidance also helps to decrease complications such as puncturing the bowel.
Genitofemoral Nerve Block
Anatomy: The genitofemoral nerve derives from the L1 and L2 spinal nerves (Enneking et al. 2009). After it emerges from psoas major muscle, it descends behind the ureter and divides into a femoral branch and a genital branch just above the inguinal ligament (Waldman 2008). The femoral branch runs lateral to the external iliac artery in the femoral sheath and innervates the skin of the thigh just below the inguinal ligament. In the male, the genital branch runs inside the inguinal canal, exits the superficial inguinal ring, follows the spermatic cord, and innervates the cremaster muscle and skin of the scrotum. In the female, the genital branch runs with the round ligament and innervates the mons pubis and labia majora on the same side.
Indications: As a diagnostic tool for chronic inguinal pain, pain relief after the block supports a diagnosis of genitofemoral neuralgia (Nachi et al. 2008).
Block technique (Nachi et al. 2008): The landmarks for a genitofemoral nerve block include the pubic tubercle, inguinal ligament, inguinal crease, and femoral artery. To block the femoral branch, one inserts the needle lateral to the femoral artery at the inguinal crease and injects local anesthetic in a fanlike fashion into the subcutaneous tissue. The medication is injected laterally to the pubic tubercle below the inguinal ligament to block the genital branch.
Sacroiliac Joint Block
Anatomy: The sacroiliac joint is a large, synovial joint characterized by irregular contours of the sacrum and ileum that provide interlocking mechanisms (Cohen 2005). The joint has limited movement and its main function is stress-relieving (Bogduk 2005). The joint volume ranges from 0.8 to 2.5 mL with an average of 1.5 mL (Bogduk 2004f). The joint is stabilized by strong ligaments, including interosseous, posterior and anterior sacroiliac ligaments (Bogduk 2005). There have been variable descriptions of the spinal nerves that give rise to branches innervating this joint. The current thinking is that the posterior aspect of the joint is innervated by the lateral branches of the posterior rami of L4–S3 and the anterior aspect of the joint is innervated by nerves derived from the anterior rami of L2–S2. A recent study showed that local anesthetic blockade at L5 dorsal rami and S1–S3 lateral branches can render only insensitivity to painful stimulation applied to the interosseous and posterior sacroiliac ligament but not the sacroiliac joint (Dreyfuss et al. 2009).
Indications: Diagnosis of pain from sacroiliac joint (Bogduk 2004f).
Block technique (Bogduk 2004f): The patient is placed in a prone position and the skin overlying the target sacroiliac joint is prepared following the standard protocol for an aseptic procedure. Using a C-arm, a fluoroscopic view which displays the anterior and posterior margin of the joint is obtained. The goal is to obtain a maximally crisp medial cortical line of the posterior joint margin. A common needle entry point is where anterior and posterior joint margins overlap. A 22- to 25-G 3½-in. spinal needle is used most often to enter the joint (Fig. 30.2). Once the needle is inside the joint, 0.3–0.5 mL contrast medium can be injected to confirm placement. Local anesthetics are then injected. The total volume from contrast and local anesthetic should not exceed 2.5 mL maximally.


Fig. 30.2
Sacroiliac joint injection. Anterior–posterior view of a fluoroscopic image shows the needle (round shadow with a short black line within) is directed to the joint
Medial Branch Nerve Block and Radiofrequency Treatment
Anatomy: Zygapophyseal or facet joints are synovial joints. Between the third cervical and first sacral level, they are formed by the inferior articular process of one vertebra and the superior articular process of the vertebra immediately below it (Cramer 2005; Boorstein and McGraw 2004). Each joint is innervated by two medial branch nerves, one that derives from the posterior ramus of the spinal nerve at the level of the joint and one from the level above.
In the lumbar region, the medial branches from the L1 to L4 dorsal rami run along the junction between the roots of subjacent transverse process and superior articular process, covered partially by the mamillo-accessory ligament (Fig. 30.3). Each medial branch nerve innervates two facet joints, the multifidus muscle, the interspinous muscle and ligaments (Bogduk 2005). The L5 dorsal ramus passes the groove where ala and superior articular process of the sacrum meet. It then gives rise to its medial branch nerve to innervate the L5–S1 facet joint and multifidus muscles.
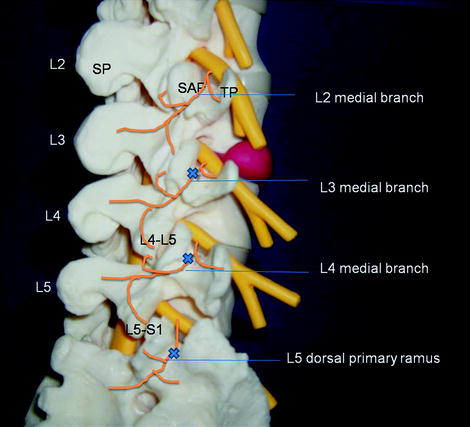
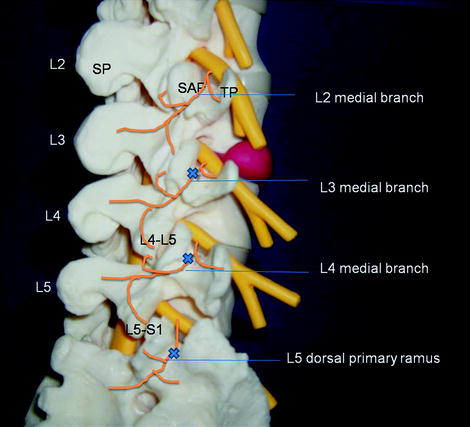
Fig. 30.3
The lumbar medial branch nerves and targets (x) for anesthetic blocks of L4–L5 and L5–S1 zygapophysial joints. L2 the second lumbar vertebra, SAP superior articular process, SP spinous process, TP transverse process, L4–L5, L4–L5 zygapophysial joint, L5–S1, L5–S1 zygapophysial joint
In the cervical region, medial branches from the C4 to C7 dorsal rami run along the waist of its respective articular pillar (Bogduk 1982; Lord et al. 1995) (Fig. 30.4). Each medial branch gives rise rostral and caudal articular branches to innervate the facet joint above and below. For example, medial branch from the C5 dorsal ramus innervates C4–C5 and C5–C6 facet joints. This is different for the C3 dorsal ramus in that it gives rise to two medial branches. A larger one, the third occipital nerve, runs along the C2–C3 facet joint and gives rise to the articular branches to it. A deep one runs around the waist of C3 articular pillar just like the other cervical medial branch nerves below it and provides innervation to the C3–C4 facet joint.
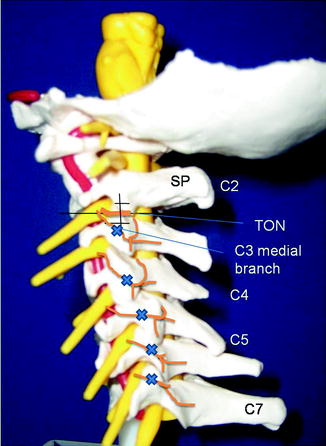
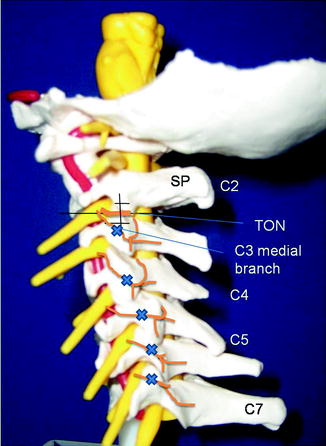
Fig. 30.4
The cervical medial branch nerves and third occipital nerve (TON). Targets (x, +) for anesthetic blocks. C2, the second cervical vertebra; SP, spinous process
In the thoracic region, medial branches from the T1 to T4 and the T9 to T10 derive from the dorsal rami of their respective spinal nerves (Chua and Bogduk 1995) (Fig. 30.5). Each of them then runs posteriorly through the intertransverse space, reaches the superolateral corner of the respective transverse process, and continues caudally along the posterior surface of the tip of the transverse process. The medial branches of T5–T8 dorsal rami do not always come into contact with the transverse process. The medial branches of T11 and T12 dorsal rami runs within the junction of the superior articular process and the base of the transverse process, in a manner similar to that in the lumbar region.
Fig. 30.5
A sketch of the medial branches of the thoracic dorsal rami viewed from behind. On the right side, the multifidus and lateral branches are not shown. TP transverse process; MB medial branch; ZJ zygapophysial joint; SP spinous process; LB lateral branch; MF multifidus; ISL, interspinous ligament; C cervical vertebra; L lumbar vertebra; asterisk atypical medial branch (Reprinted with permission from Springer-Verlag Wien. The image was originally published in Chua and Bogduk (1995))
Indications: Medial branch nerve blocks are used to determine if a facet joint is the pain generator and radiofrequency treatment of the medial branch nerves are used to treat facet joint pain (Bogduk 2004a, c).
Block technique: The skin over the injection site is prepared and draped according to the standard protocol for aseptic procedures.
To block lumbar medial branch nerves, the patient is placed in the prone position with a pillow under the abdomen to decrease lumbar lordosis (Bogduk 2004c). An oblique view of the ipsilateral lumbar spine is obtained using a C-arm fluoroscope (Fig. 30.6). The target point for the L1–L4 medial branch is the junction of the superior articular process and the transverse process (Fig. 30.7a–c). The target point for L5 dorsal ramus is the junction of the superior articular process of the sacrum and ala (Fig. 30.3).

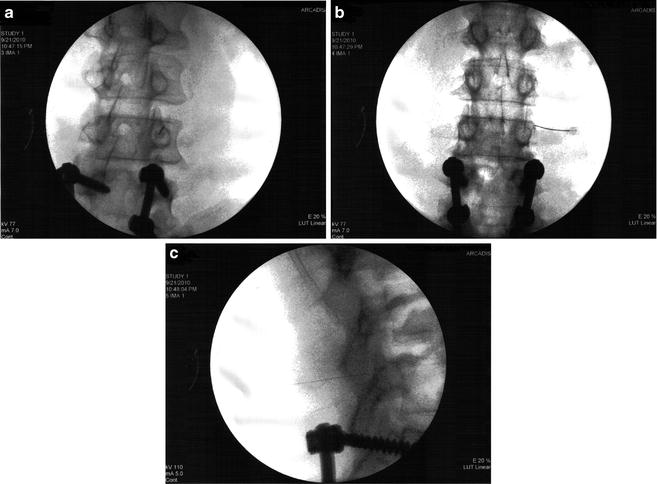

Fig. 30.6
The setting during a medial branch block. Needle placement is guided by fluoroscopic images
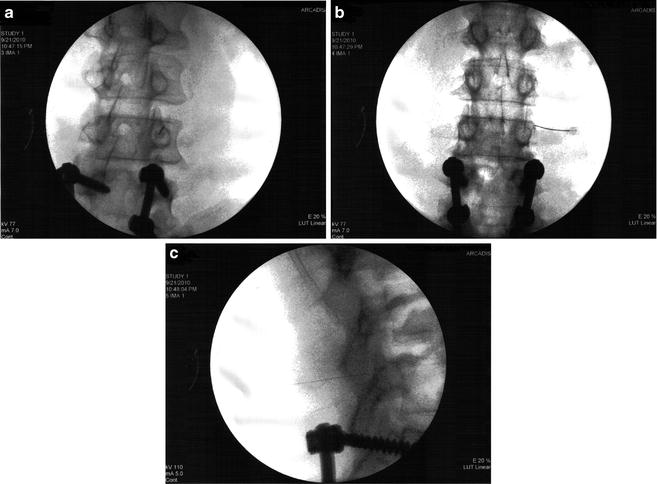
Fig. 30.7
(a) Fluoroscopic images of needle positions during a medial branch block (oblique view); (b) Fluoroscopic images of needle positions during a medial branch block (anterior–posterior view); (c) Fluoroscopic images of needle positions during a medial branch block, (lateral view)
To block cervical medial branch nerves, the patient is placed in either a prone or supine or lateral (affected site up) position. A true lateral view, the right and left articular pillars of cervical spine at the level to be blocked are superimposed, is obtained using a C-arm. To adequately block the third occipital nerve, it is recommended that local anesthetic be placed at three target points over the C2–C3 joint capsule. Precisely, one is to draw an imaginary vertical line bisecting the C2–C3 joint (Fig. 30.4). On this line, the highest target point is at the level of the tip of the C3 superior articular process, the middle line is at the level of the joint and the lowest point is at the level of the bottom of the C2–C3 intervertebral foramen. To block C3–C6 medial branch, the target point is at the middle of the centroid of the articular pillar of the appropriate cervical vertebra (Fig. 30.8). To block the C7 medial branch nerve, the target point is at the apex of the C7 superior articular process.


Fig. 30.8
Fluoroscopic images of needle positions during cervical medial branch blocks (oblique view). The highest needle in this picture shows one of the positions for blocking TON. The next three needles are in positions to block C3, C4, and C5 medial branches
To block the thoracic medial branch nerve, the patient is placed in a prone position. An oblique view of the ipsilateral thoracic spine is obtained using a C-arm. The target point for blocking a medial branch nerve derived from the T1 to T4 and T9 and T10 nerves is the superior lateral corner of the transverse process of the level to be blocked (Chua and Bogduk 1995; Nelson 2008). The target point for the T11 or 12 medial branch nerve is the junction of the superior articular process and transverse process. This is similar to that at the L1–L4 level. The target point for a medial branch block at the T5–T8 level is below the rib at the depth of the transverse process.
Local anesthetic is delivered to the target site using a 22- or 25-G spinal needle. In a retrospective evaluation of 500 consecutive patients with chronic neck, thoracic or low back pain, Manchukonda et al. (2007) reported that the false-positive rates after a single medial branch block at the cervical, thoracic, and lumbar spine were 45, 42, and 45% respectively. In order to reduce this false-positive response, comparative local anesthetic blocks have been advocated (Bogduk 2004a, c). This is accomplished by two injections separated by weeks. On one occasion the patient receives a local anesthetic such as lidocaine with a short duration of action. On another occasion, the patient receives a local anesthetic such as bupivacaine with a long duration of action. In general, a positive response constitutes 80% pain reduction with the ability to perform previously painful movements on both occasions (Manchukonda et al. 2007). Patients with positive responses can then be treated with radiofrequency therapy.
Continuous radiofrequency medial branch neurotomy (Bogduk 2004e): To perform a continuous radiofrequency medial branch neurotomy at either the cervical, thoracic, or lumbar spine, the patient is usually placed in a prone position. An appropriate size radiofrequency cannula depending on the anatomical characteristics (5–15 cm length, 18–22 G with a 5–10 mm active tip) is placed parallel to the target nerve under fluoroscopy guidance. The proximity of the electrode to the nerve can be estimated by sensory stimulation at 50 Hz and less than 0.5 V. Motor testing to ensure the electrode is placed sufficiently away from a motor nerve is conducted at 2 Hz and no less than three times the sensory threshold or 3 V (Rathmell 2006a). Once the position of the cannula is satisfactory, target site is anesthetized with local anesthetic and a thermal probe is placed into the cannula. Thermal lesioning is carried out at no less than 80°C and no more than 85°C for 60–90 s.
Pulsed radiofrequency of medial branch (Rathmell 2006a): To perform pulsed radiofrequency of medial branch at the various level of the spine, the radiofrequency cannula is placed perpendicular to the target nerve, in the same way as the needle placement for medial branch block. After sensory and motor testing, pulsed radiofrequency treatment is performed at 42°C with a voltage between 40 and 45 V for 120 s.
Stellate Ganglion Block
Anatomy: The stellate ganglion is the fusion of the inferior cervical ganglion and the first thoracic ganglion in most individuals (Erdine 2008). It is located at the vertebral level between C7 and T1. The surrounding structures include the longus colli muscle medially, scalene muscles laterally, subclavian and vertebral arteries anteriorly, transverse processes and prevertebral fascia posteriorly and posterior aspect of the pleura anterior and inferiorly. It is also near the phrenic nerve, recurrent laryngeal nerve, and brachial plexus (Molloy and Benzon 2008). As part of the sympathetic nervous system for the head and neck, all preganglionic fibers originate from the anterolateral horn of the first and second thoracic spinal cord segments (Erdine 2008). They either synapse or pass the inferior cervical ganglion. On the other hand, not all preganlionic fibers of the upper extremity sympathetic nerve system relay through the stellate ganglion. The upper extremity sympathetic preganglionic fibers originate from the T2 to T8 and sometimes the T9 anterolateral horn cells. These fibers synapse at the second thoracic ganglion, stellate ganglion, and sometimes the middle cervical ganglion. Postganglionic fibers from the stellate ganglion join gray rami communicates to enter C7, C8, and T1 spinal nerves to the upper extremity. Other postganglionic fibers from the stellate ganglion form a cardiac branch, ansa subclavius, and vertebral plexus (Darby 2005).
Indications: Relief sympathetically mediated pain in the upper extremities, head, and neck. The most common application is complex regional syndrome I and II of the upper extremity. Stellate ganglion block is also used to treat vascular insufficiency from occlusion and embolism, vasospasm, phantom limb pain, pain due to Paget disease, herpes zoster, postherpetic neuralgia, postradiation neuritis, intractable angina pectoris, frostbite, and hyperhidrosis (Erdine 2008; Rathmell 2006b; Breivik and Cousins 2009).
Block technique: Stellate ganglion block has been done for many years using anatomical landmarks without image guidance. The patient is placed in a supine position without a pillow and often with a towel roll under the shoulders to keep the neck in extension (Erdine 2008; Brown 2006i). The patient’s head should be turned slightly to the contralateral site of the procedure. After skin preparation according to procedures for aseptic technique, the C6 vertebral tubercle (Chassaignac’s), trachea and the carotid artery are identified. While keeping the carotid artery retracted laterally and the trachea medially, a 22- or 25-gauge needle is inserted through the skin until contacting the C6 transverse process. The needle is then pulled back 1–2 mm to have the needle tip outside of the longus coli muscle. After negative aspiration for blood and CSF, 0.5 mL of the anesthetic solution (such as 0.25% bupivacaine or 0.2% ropivacaine) is injected first. The patient should be told beforehand that he or she should avoid cough and speaking during the procedure. The patient is instructed to raise his/her thumb to request the procedure to be stopped. If no adverse reactions noted during the testing dose, additional anesthetics can be injected slowly in 3–4 mL interval. The total volume of anesthetic is usually 5–10 mL. Some use 1:200,000 epinephrine with local anesthetic as a test dose. Once the block is completed, the needle is removed, the patient should be observed for at least 30 min. To increase block accuracy and decrease complications, the use of fluoroscopic guidance (Abdi et al. 2004) or ultrasound guidance (Narouze et al. 2007; Gofeld et al. 2009) has been strongly advocated. When image guidance is available, the block can be done at the C7 level. This allows the needle to be placed at the location of the ganglion and decreases the volume of local anesthetic injection. However, this is associated with increased risk of pneumothorax and puncture of the vertebral artery (Erdine 2008; Abdi et al. 2004).
Celiac Plexus, Splanchnic Nerve Block, and Neurolysis
Anatomy: The celiac plexus is a network of nerve fibers and ganglia that are located anterior to the abdominal aorta and between the origin of the celiac and superior mesenteric arteries at the T12–L2 vertebral level (Darby 2005; Loukas et al. 2010). Sympathetic preganglionic fibers from the greater splanchnic nerves synapse on neurons in the celiac ganglia. The great splanchnic nerve derives from the T5 to T9 and sometimes the T10 thoracic sympathetic ganglia. The great splanchnic nerve descends obliquely along the lateral vertebral body and pieces the diaphragm to enter the abdominal cavity. Preganglionic sympathetic fibers in the lesser splanchnic nerve from the T9 and T10 or the T10 and T11 thoracic ganglia pierce the diaphragm with the greater splanchnic nerve and synapse at the aorticorenal ganglion, which is the lower, separate part of the celiac ganglia. The least splanchnic nerve that is present in 56% of cases derives from the T12 or the T11 and T12 thoracic ganglia. It synapses at the renal plexus after entering the abdomen. Postganglionic sympathetic fibers from the celiac plexus form downstream secondary plexuses near the target organs. These include hepatic, phrenic, gastric, splenic, testicular, ovarian, superior and inferior mesenteric, renal and abdominal aortic plexuses. Consequently, blockade of the celiac plexus can affect abdominal visceral pain.
Indications: Pain from abdominal viscera including pancreas, liver, gallbladder, omentum, mesentery and gastrointestinal tract from stomach to the transverse colon (Niv and Gofeld 2008; Rathmell 2006c).
Block technique: There are several approaches to perform a celiac plexus block. There are two large categories based on needle entry during the procedure, either posterior or anterior approaches. The classic description by Kappis employs a posterior approach which has been the basis for modern modifications in performing the block under fluoroscopy or CT guidance (Niv and Gofeld 2008; Rathmell 2006c). The patient is usually given intravenous conscious sedation with monitoring of cardiac rhythm, heart rate, blood pressure, and oxygen saturation. If using a fluoroscope to perform the procedure, the patient is placed prone on the procedure table. The scope is rotated to the ipsilateral site of needle entry until the tip of the transverse process of L1 overlies the anterolateral margin o f the L1 vertebral body. Frequently, the procedure is performed on the left side first. The skin and subcutaneous tissue that overlay the upper 1/3 of the lateral margin of the L1 vertebral body are anesthetized with 1% lidocaine, followed by insertion of a 22-gauge, 5–7-in. long spinal needle along the X-ray beam to contact the anterolateral margin of L1 vertebral body. The needle is then advanced 2–3 cm anterior to the anterior aspect of L1 vertebral body with the fluoroscope rotated to provide lateral views. Sometimes, the needle enters the aorta during the process. If this occurs, the needle should be advanced further until it completely penetrates through the aorta (this constitutes the transaortic approach). The needle position is verified on an AP view. One to two ml of radiographic contrast is injected after negative aspiration for blood, CSF, urine, and lymphatic fluid. The contrast may cover the left and right area anterior to the aorta. If this occurs, there is no need to perform a block on the right side. Otherwise, the procedure is repeated on the right side. For a celiac plexus block, 20–40 mL of local anesthetic, such as 0.25% bupivacaine or 0.2% ropivacaine is injected in increments of 5 mL with intermittent aspiration. If the procedure is repeated on the right side, 20–40 mL of local anesthetic is divided in half and distributed on each side. For neurolytic block, replace the local anesthetic with 50–100% alcohol or 6–10% phenol. A higher concentration of alcohol is often diluted with local anesthetics to a lower desired concentration. A higher concentration of phenol is often diluted with radiographic contrast. If a splanchnic nerve block or neurolysis is desired, the fluoroscope is tilted cephalocaudad to clear the 12th rib after lining up the tip of the L1 transverse process with the lateral margin of the L1 vertebra. The needle is then directed towards the anterolateral aspect of the T12 vertebra just below the 12th rib. This is also the end point for needle insertion during the retrocrural approach.
More recently, celiac plexus block/neurolysis has been completed by the guidance of endoscopic ultrasound (Wiersema and Wiersema 1996; Levy and Wiersema 2003). Although the celiac plexus cannot be visualized by ultrasound, its location in relation to celiac trunk is relatively stable. Vascular landmarks can be easily identified by color doppler. Using a transgastric anterior approach, access to the celiac plexus is much more direct than techniques guided by fluoroscopy or CT via either posterior or anterior approach. Because this approach avoids the retrocrural space, it may have lower risk of neurological and pulmonary complications (Levy and Wiersema 2003). The current, limited data suggest the efficacy of this approach is not inferior to other percutaneous methods (Chak 2009).
Lumbar Sympathetic Block
Anatomy: The lumbar sympathetic chain is part of the paravertebral sympathetic system that is situated at the anterolateral vertebral bodies bilaterally. It consists of ganglia, mostly four pairs at the level of the second to fourth lumbar vertebra, and connecting nerve fibers. The ganglia receive preganglionic fibers that originate from neurons in the lateral horn, intermediate nucleus, and paracentral nuclei of the thoracolumbar spinal cord via the white rami communicantes (Niv and Gofeld 2008). Postganglionic fibers join the lumbosacral plexus via the gray rami communicantes and the L1–L5 nerves.
Indications: Sympathetically mediated pain such as complex regional pain syndrome (CRPS) type I and type II, peripheral vascular insufficiency secondary to diffuse microvascular occlusion and other low extremity neuropathic pain may be reduced by this block (Rathmell 2006d).
Block technique (Niv and Gofeld 2008; Rathmell 2006d): Currently, a lumbar sympathetic block is carried out under fluoroscopic guidance. To perform the block, the patient is placed in a prone position. Lumbar vertebrae are identified under fluoroscopic image. The C-arm is oblique to the side to be blocked such that the lateral edge of the transverse process and lateral edge of the vertebral body are overlapped. This permits the needle entering the skin to reach the vertebra without bony structures in the way. For an anesthetic block, it is recommended to place the needle superior to the L3 transverse process in order to avoid the exiting spinal nerve root. Once the block needle touches the vertebra, the C-arm is rotated to a lateral view, the needle is then walked off laterally to reach the first 1/3 portion of the vertebra. The C-arm is then rotated to an anterior–posterior position. The block needle should be medial to the lateral margin of the vertebra. Nonionic contrast is injected to confirm needle position and rule out intravascular needle placement. Fifteen to twenty ml local anesthetic is injected, i.e., 0.25–0.5% bupivacaine. A minimal of 1–2°C rising in skin temperature of the lower extremity on the side of the block signifies a successful sympathetic block. Neurolysis with 10% phenol, or 50–100% ethyl alcohol or radiofrequency have been well described but is not done frequently in routine clinical practice due to post-sympathectomy pain.
Superior Hypogastric Plexus Block
Anatomy: The superior hypogastric plexus, an extension of the aortic plexus, is located anterior to the aorta and inferior to its bifurcation at the vertebra level of L5–S1 (Bosscher 2001). The lower two lumbar splanchnic nerves also send input to this plexus (Brown 2006j). The superior hypogastric plexus descends and divides along the internal iliac arteries to form the hypogastric nerve, which connects with inferior hypogastric plexus (Bosscher 2001). Most subsidiary plexuses to the pelvic organs originate from the inferior hypogastric plexus. Pelvic visceral pain afferent fibers, which have their cell bodies in the dorsal root ganglion, travel along the autonomic system. Therefore, blockade of the superior hypogastric plexus offers relief from pain originating from pelvic organs.
Indications: Pain from gynecological disorders, such as inflammatory pelvic disorders and adhesions, pelvic visceral pain due to nongynecological diseases, such as interstitial cystitis, irritable bowel syndrome and chronic pain after pelvic surgery, tumors of the pelvic organs. (Erdine and Ozyalcin 2008).
Block technique: The superior hypogastric block is performed with the aid of a fluoroscope. The patient is placed prone on the table. The skin overlaying the lumbosacral region is prepared and draped per routine for aseptic procedures (Stevens et al. 2000). After anesthetizing the skin and subcutaneous tissue, under fluoroscope guidance, a 7-in. 22-gauge spinal needle is inserted on one side of the L5 vertebra. The final tip position is just anterior to the L5 vertebra. Similar steps are then repeated on the other side. Radiographic contrast is injected after negative aspiration for blood to confirm the proper placement of the needle. This is followed by 6–8 mL of local anesthetic such as 0.25% bupivacaine or 0.2% ropivacaine on each site in the case of a diagnostic block. If longer-term relief is desired, neurolytic agents, 6–10% of phenol or 50% alcohol can be used instead (Erdine and Ozyalcin 2008).
Ganglion Impar Block
Anatomy: The ganglion impar, also known as the ganglion of Walther, is the union of the two sympathetic chains that located just anterior to the coccyx (Oh et al. 2004). Visceral afferents transmitting pain from the perineum, distal rectum, anus, distal urethra, vulva, and distal third of the vagina converge at this ganglion (de Médicis and de Leon-Casasola 2001).
Indications: Visceral or sympathetically mediated pain in the perineum, rectum, and genitalia (Erdine and Ozyalcin 2008).
Block technique: Several techniques have been described to block the ganglion impar under fluoroscopy guidance. These include the introduction of a bend needle through the anococcygeal ligament (Erdine and Ozyalcin 2008) or paracooccygeally (Foye and Patel 2009). Alternatively, a straight needle can be advanced through sacrococcygeal junction (Erdine and Ozyalcin 2008) or coccygeal joint (Hong and Jang 2006). Accurate needle placement is confirmed by radiographic contrast spreading along the anterior wall of sacrum and coccyx (Fig. 30.9). For diagnosis and temporary relief, 4–6 mL of local anesthetic such as 0.25% bupivacaine or 0.2% ropivacaine or 1% lidocaine can be injected. For longer-term relief, 4–6 mL of 6% phenol can be used (de Médicis and de Leon-Casasola 2001).
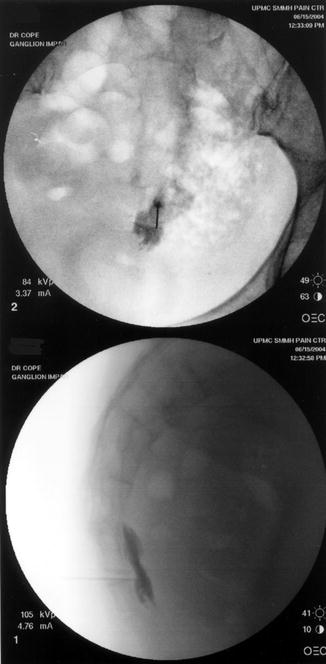
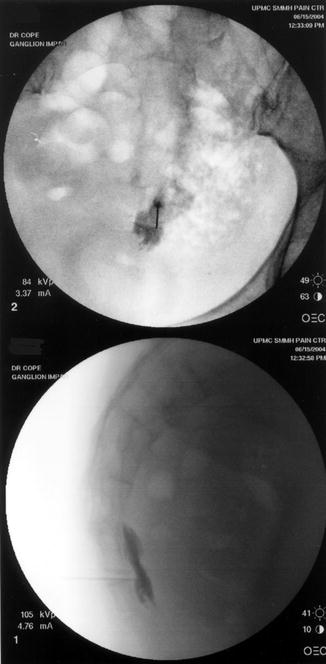
Fig. 30.9
Ganglion impar block. Top image, the anterior–posterior view; lower image, lateral view. Contrast was spreading along the anterior wall of sacrum and coccyx
Epidural Steroid Injection
Anatomy: The epidural space is defined as the space outside the dura mater and within the bony spinal canal (Hogan 2009). The space starts superiorly from foramen magnum and ends inferiorly at sacral hiatus. The anterior boundary is the posterior longitudinal ligament, the vertebral body, and the intervertebral disc. Posteriorally, it is limited by the lamina, zygapophyseal joint, and ligament flavum. Laterally, the neural foramens allow the passage of nerves, vessels, and lymphatics, whereas pedicles protect the space. The epidural space is filled by areolar fat. It is largest in the mid-lumbar region and decreases progressively cephalad that it becomes a potential space above the C7 level. The internal vertebral venus plexus, the spinal branches of the segmental arteries, lymphatics and dura arachnoid projections that surround the spinal nerve are also found in the epidural space (Botwin et al. 2004).
Indications: Radicular pain in cervical, thoracic, and lumbar regions due to disc pathology or spinal stenosis (Bogduk 2010; Obray and Huntoon 2008).
Block technique: The epidural space can be accessed via the interlaminar, transforaminal, and caudal route (Fig. 30.10). Although blind technique has been used for many years to place medication into the epidural space via the interlaminar or caudal route, fluoroscopy guidance is highly recommended because needle placements are not always in the epidural space even in experienced hands (Price et al. 2000; Bartynski et al. 2005).
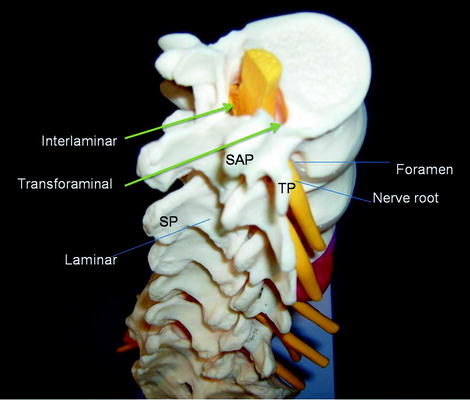
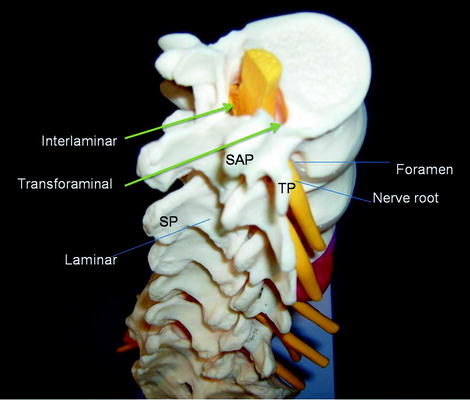
Fig. 30.10
Access the epidural space via the interlaminar or transforaminal route. SAP superior articular process; SP spinous process; TP transverse process
Interlaminar approach: The principles of interlaminar epidural steroid injection at the cervical, thoracic, and lumbar spine are the same. Technically, there are specifics for each level to accommodate regional anatomy. In general, to perform an epidural steroid injection under fluoroscopic guidance in the cervical, thoracic, or lumbar spine, the patient is placed in a prone position. Skin overlaying the injection site is cleaned and draped according to standard practice for an aseptic procedure. An anterior–posterior fluoroscopic image is obtained and the C-arm is adjusted to maximize the target interlaminar space for needle access. Skin and subcutaneous tissue is anesthetized with 1% lidocaine. A 20-gauge 3½-in. or 18-gauge 5-in. Tuohy needle is inserted through the skin and gently pushed towards the epidural space with the guidance of intermittent anterior–posterior and lateral fluoroscopy. Loss of resistance to saline or air adds the identification of epidural space. The needle position is confirmed by 1–2 mL nonionic radiographic contrast medium (Fig. 30.11a, b). This also serves to rule out intrathecal or intravascular needle placement. Steroid diluted in preservative free saline is injected followed by removal of the needle and placement of a bandaid (Rathmell 2006e).
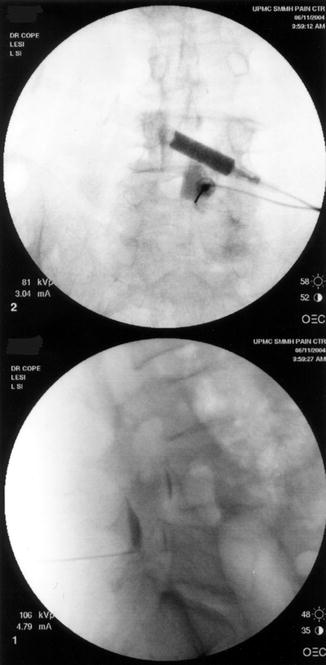
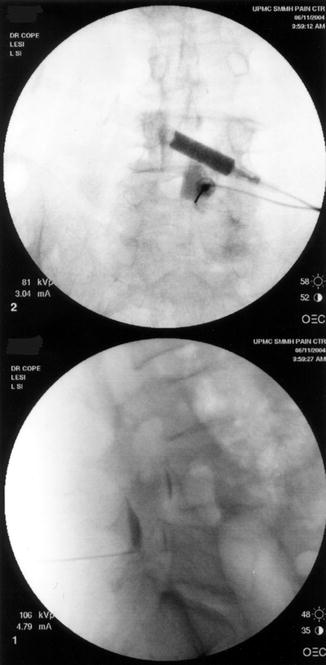
Fig. 30.11
Interlaminar epidural steroid injection. Contrast pattern demonstrated epidural spread
Transforaminal approach: The use of a fluoroscope is essential when this approach is utilized. In the lumbar region, the procedure is carried out with the patient in the prone position. After the skin is cleaned and draped according to protocol for aseptic procedure, an anterior–posterior fluoroscopic image is obtained. The C-arm is adjusted so that the anterior and posterior edges of the inferior vertebral end plate of the upper of the two vertebrae of the target segment are superimposed. The C-arm is then obliqued towards the site to be injected until the superior articular process of the lower vertebra is under the pedicle of the upper vertebra. There are two techniques, subpedicular and retroneural. In the subpedicular approach, the final position of the needle tip is above the nerve root and below the pedicle near the posterior vertebral surface (Fig. 30.12). In the retroneural technique, the needle entry point is slightly lateral to the tip of superior articular process of the lower vertebra. The final position of the needle tip is right behind the exiting nerve root (Fig. 30.12). Once the needle placement is in a satisfactory position as judged by fluoroscopy, a small amount of contrast is injected to ensure neither intrathecal nor intravascular injection occurs (Figs. 30.13). This is followed by the injection of a mixture of steroid and local anesthetic (Bogduk 2004d). To inject the S1 nerve root, the subpedicular technique is used.
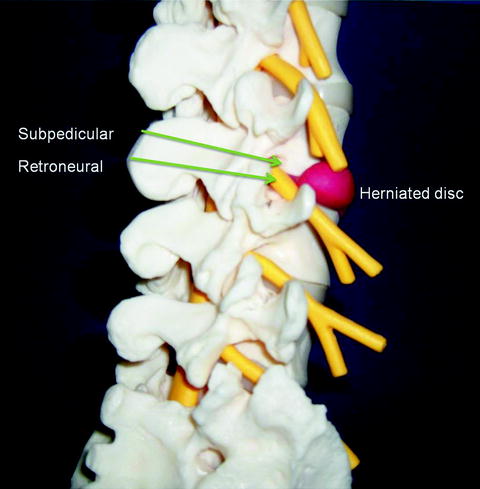

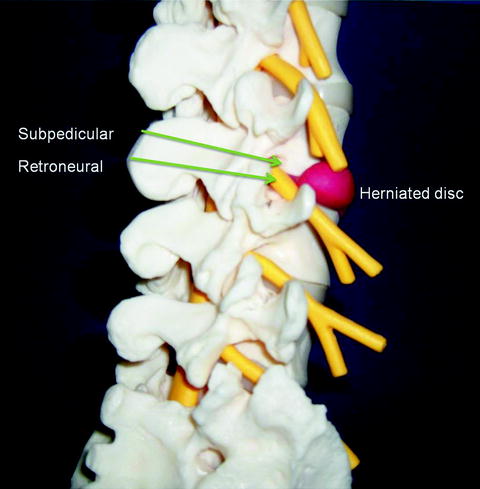
Fig. 30.12
Subpedicular or retroneural approach to perform transforaminal epidural steroid injections

Fig. 30.13
Fluoroscopic images of a transforaminal epidural steroid injection by retroneural approach. This is also termed selective nerve root block because the needle tip is outside the intervertebral foramen. Top image, anterior–posterior view; lower image, lateral view
Cervical transforaminal epidural steroid injection is much more technically demanding. It is performed with the patient in supine, oblique, or lateral position (Bogduk 2004b; Rathmell 2006f). After preparation of the procedure field, the C-arm is obliqued towards the site to be treated, so that the intervertebral foramina are clearly visualized. The needle entry site is over the anterior half of the superior articular process that forms the posterior wall of the target intervertebral foramen. The needle is first placed on this bone and then readjusted to pass tangentialy into the intervertebral foramen by no more than 2–3 mm. Prior to injection of steroid and local anesthetic, the needle position is confirmed by fluoroscopy with contrast. Digital subtraction angiogram increased the sensitivity of detection of intravascular injection.
Thoracic transforaminal epidural steroid injection is also technically demanding and is performed much less frequently. Detailed descriptions can be found in the Practice Guidelines, Spinal Diagnostic and Treatment Procedures published by the International Spine Intervention Society (Bogduk 2004g).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





