1. Understand the anatomy at the location of planned needle entry
2. Review the skin integrity for lesions or local infection
3. Review recent plain films if there is concern about barriers to needle placement
4. Review recent CT or MRI images if significant stenosis is a concern
5. Plan the angle of approach for the needle, including the paramedian angle and needle-to-spine angle (as illustrated in this chapter)
6.2 Technical Overview
After proper patient preparation, the physician should develop a strategy for needle placement. This strategy should include level of entry, angle of entry, side of entry, and method of identifying the epidural space. The physician should also plan the site for the placement of the needle tip at the time of epidural space entry in relation to bony landmarks. Once the route of entry is determined, a local anesthetic injection is given (Fig. 6.1). At this point, a #15 blade is used to make a small stab wound to place the needle. This step allows for an easier entry into the tissues and may reduce the risk of introducing infection into the epidural space from skin pathogens. The needle is then ideally placed at an angle of 30–45° and advanced until it contacts the lamina of the vertebral body caudal to the planed interlaminar space entry. It is then advanced and “walked off” cephalad into the ligament (Fig. 6.2). In some patients, anatomical variants may require modification of the needle angle to increase the ease and safety of access. In addition, the body habitus of the patient must be accommodated: If the patient is obese, a more caudal skin entry site is required to ensure maintenance of the desired needle angle of entry, whereas a more cephalad skin entry site is needed for very thin patients. Once the needle is established in the ligament, the stylet is removed and the needle is advanced carefully, using the loss of resistance or hanging drop technique (Figs. 6.3 and 6.4). Some have described a method of using a wire to identify the entry into the epidural space, but this technique is not well established or uniform and should be used only if the implanter is trained in this approach. In some settings, such as in the upper thoracic spine, the anatomy makes entry into the epidural space at a reasonable angle difficult. In these settings, the use of a curved-tip needle may be helpful. An example of this type of needle is seen in Fig. 6.4.
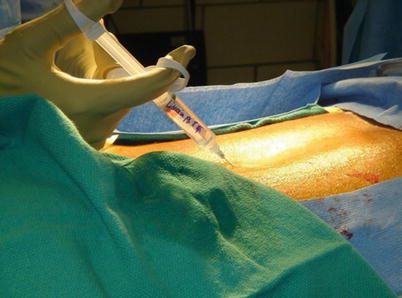


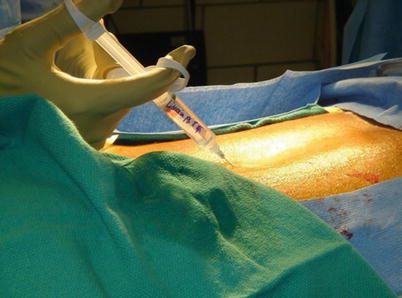
Fig. 6.1
Local anesthetic should be applied in the same plane that is planned for the needle placement. The local anesthetic should be placed in the skin and subsequent tissues to the level of the supraspinous ligament. If the needle is advanced aggressively into the spine, injection of local anesthetic into the spinal fluid can lead to an accidental spinal block

Fig. 6.2
The angle of needle placement should be between 30° and 45° when possible. In some cases, the patient’s anatomy will not lend itself to that angle and adjustments must be made accordingly

Fig. 6.3




Ideal needle placement with stylet removed
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







