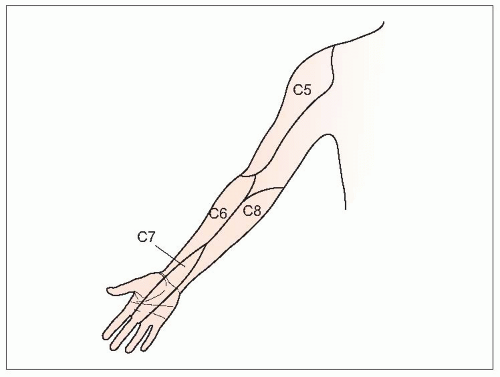
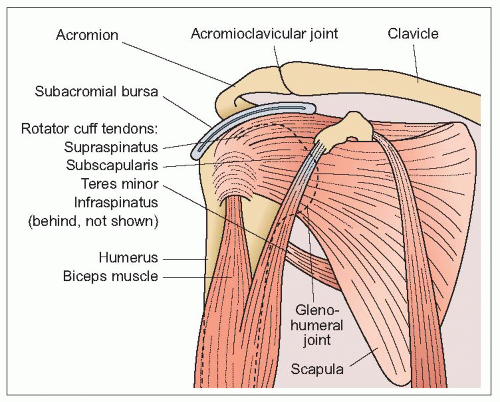
The shoulder is a complex structure (
4.6). Shoulder pain can be caused by overuse in older adults or trauma in young patients (
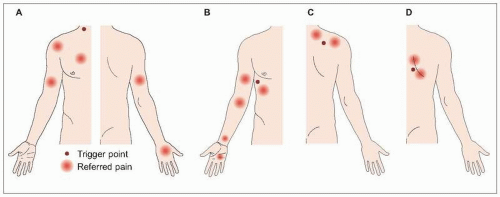
Table 4.3). Pain in the anterior shoulder often results from osteoarthritis of the true shoulder joint (glenohumeral joint) or more commonly acromioclavicular joint or biceps tendonitis. Anterior and lateral pain occur with subacromial bursitis and rotator cuff tendonitis.
History of trauma or overuse, pain features, and physical examination can help distinguish among common causes of shoulder pain (
Table 4.4). Although these features can assist in determining a diagnosis, the clinical evaluation of shoulder pain can be difficult. Several studies have compared results among clinicians when evaluating patients with shoulder pain complaints. In general, diagnostic agreement is poor to moderate. In one study, 44 patients
with shoulder pain were evaluated by three rheumatologists
6. Agreement among clinicians was only 46%. When the three rheumatologists evaluated the patients together and discussed diagnostic signs and symptoms, agreement improved to 78%. In another study, diagnostic agreement between two experienced physical therapists for 201 patients with shoulder pain was only moderate (60%)
7. Agreement was worse among patients with bilateral, chronic, or severe pain. Clinical tests assessing shoulder function and range of motion are also notoriously unreliable in shoulder pain patients
8,
9,
10. For this reason, most patients with chronic shoulder pain will require radiographic studies in addition to history and physical examination (
Table 4.5). Partial rotator cuff tears are best assessed with
MRI or ultrasound. A comparison of both techniques against arthroscopic findings in 71 patients with rotator cuff tears showed similar good identification and size measurement for both full and partial tears
11.
Rotator cuff tendonitis
Rotator cuff tendonitis is a common cause of shoulder pain. A prospective, 1-year survey of 131 patients presenting to their primary care physicians for shoulder pain identified rotator cuff tendonopathy in 85%
12. Inflammation within the rotator cuff is often combined with subacromial bursitis and termed impingement syndrome. Pain is generally
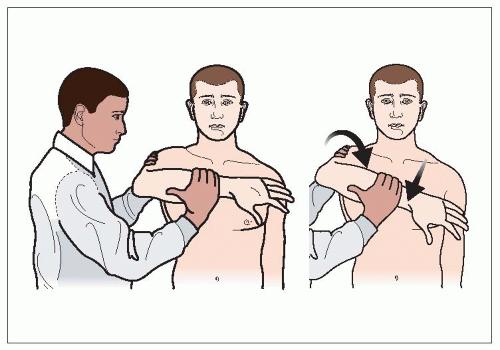
located over the anterior and lateral shoulder. Impingement syndrome can be confirmed with the Hawkins test (
4.8). Rotator cuff tendonitis pain is aggravated with overhead activities and is worse at night. Clicking or popping may occur in the affected shoulder.