6 Musculoskeletal causes and the contribution of sport to the evolution of chronic lumbopelvic pain
Assessment of the movement system
Lumbopelvic cylinder and chronic pelvic pain
Assessment and rehabilitation of muscles of the lumbopelvic cylinder
Assessment and rehabilitation of muscles of the lumbopelvic cylinder
The neural system and chronic pelvic pain
Sporting activities and chronic pelvic pain
The effect of aerobic exercise on chronic pelvic pain
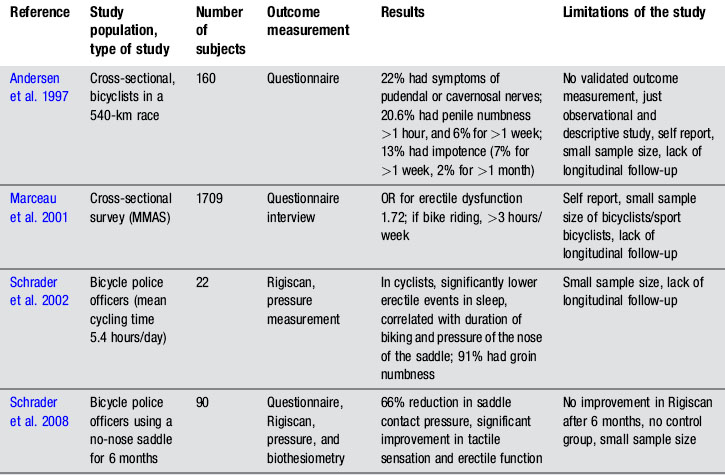
Cycling and genitourinary symptoms in men and women
Sports involving repetitive flexion of the hip
Introduction
Although it is generally accepted that movement changes with pain, there is little agreement regarding the processes that underlie movement changes and their relevance to rehabilitation of musculoskeletal pain (Hodges & Moseley 2003, Tsao et al. 2010). Additionally, one of the main difficulties in the diagnosis of pain in the pelvis is the overlap of signs and symptoms in various conditions, including medical conditions not directly related to musculoskeletal injuries (Nam & Brody 2008). As discussed in Chapters 1, 2, 3, 8 and 12, these can include urinary tract infection, prostatitis and other urinary, bowel and sexual dysfunctions. The urological, neurological, muscular, skeletal and fascial systems may all have a role to play to varying degrees, and consideration of each is necessary to provide a more accurate diagnosis, and a more valid paradigm on which to base treatment. Furthermore, as discussed in Chapter 2, pain perceived to be within the pelvis can be referred from the thoracolumbar spine, sacroiliac joint and the hip (Lee 2004), and since the body operates as a complete movement system, each component of the system is capable of influencing distal and proximal regions.
In this chapter, the authors consider the concept of movement as a physiological system, and describe a method of assessment based on analysis of a patient’s movement (dys)function, combined with an assessment of their injury history and pain presentation (Sahrmann 2002). Rehabilitation is then focused upon restoring efficient movement patterns, improving function, and less on treating the pain per se. Manual therapists have traditionally used the client’s pain patterns and physical findings, such as pain provocation tests, to identify structures contributing to mechanical pain. However, in the presence of central sensitization and neurogenic pain mechanisms, the reliability of such a pathoanatomical assessment to identify the sources of pain can be limited, particularly as the relationship between pain and the state of the tissues becomes weaker as pain persists (Moseley 2007). Classification of movement patterns, used to identify the mechanical causes of pain, may be similarly limited in the presence of central sensitization, where any mechanical stimulus may be sufficient to generate a painful response. At all times then, current pain physiology, and other contributing factors to chronic pelvic pain (CPP), as discussed in Chapters 1, 2 and 3, need to be considered when assessing the movement system. The role of clinical reasoning is further described in Chapter 7.
Assessment of the movement system
As discussed in Chapters 1 and 2, the movement system is modulated by many factors from across somatic, psychological and social domains (Moseley 2007). It is recognized that the nervous system is likely to coordinate muscle activity to meet the demands for stable movement, so it will not only be affected by the task, posture or movement direction, but potentially the real or perceived risk of injury (Hodges & Cholewicki 2007). Motor changes have been documented to occur throughout the movement system, at the motoneuron level and coordination of muscle behaviour, to changes in organization of the motor cortex (for a review see Tsao et al. 2010). Strategies adopted during pain and injury can increase protection of injured or painful parts, but can have mechanical consequences that may prolong pain states, or result in a higher incidence of recurrence (Hodges & Moseley 2003, van Dieen et al. 2003). In controlled clinical trials, rehabilitation of these motor changes has been linked to clinical improvement, resulting in improvements in pain and dysfunction (Cowan et al. 2003, Ferreira et al. 2006). More recently such improvements have also been shown to be associated with recovery of plastic changes at the motor cortex (Tsao et al. 2010).
Various classifications for the analysis of movement and the sub-classification of movement dysfunction have been proposed (McGill 2002, Sahrmann 2002, McKenzie & May 2003, O’Sullivan 2005) and in some instances are gaining good evidence of validity and reliability (Van Dillen et al. 1998, 2003, Dankaerts et al. 2006, Harris Hayes et al. 2009, 2010). It is beyond the scope of this chapter to describe the benefits and limitations of each classification system; however it is reasonable to suggest that the multidimensional problem of chronic low back and pelvic pain should also encompass biopsychosocial principles (Linton 2000, Waddell 2004, Woby et al. 2004, 2007) which are discussed in Chapter 7. The following section describes the evaluation, classification, and subsequent rehabilitation of lumbopelvic movement disorders based upon the work of Sahrmann (2002).
Sahrmann (2002) suggested a classification system for the analysis of lumbopelvic movement and the subsequent prescription of treatment based on clinically assessed movement system dysfunction. A central tenant of the system is that ‘faulty movement can induce pathology, not just be a result of it, and musculoskeletal pain syndromes are seldom caused by isolated events but are the consequence of habitual imbalances in the movement system’ (Sahrmann 1993). Therefore, specific postures and movements that produce pain need to be identified and corrected, as misalignment and aberrant movement patterns might result in further pain and future recurrences (Van Dillen et al. 2003).
The objective examination has two major components:
1. The patient reports the response of symptoms to the movement pattern tested, i.e. whether there is an increase or decrease in symptoms;
2. Assessment of bony and/or joint alignment, in various positions, as outlined in Table 6.1.
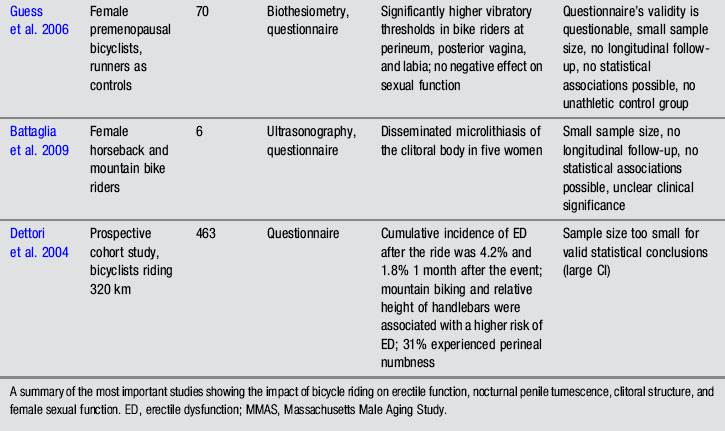
Table 6.1 Items from original examination (Van Dillen et al. 1998) proposed as important for classification of mechanical low back pain organized by test position, symptom behaviour with variations of the test position or movements within the test position, and clinical judgements of quality of alignment or movement ![]()
| Test position | Symptom behaviour with | Judgement of alignment or movement |
|---|---|---|
| Standing | ||
| Sitting | ||
| Supine | ||
| Hook (crook) lying | ||
| Prone | ||
| Quadruped |
* A judgement of relative flexibility refers to a judgement made by the examiner about the relative timing of movement of the lumbar region and the proximal joints when the patient performs a trunk or a limb movement. In general, a patient exhibits a relative flexibility impairment if the lumbar region moves in the first 50% of the range of the overall movement or excessively during the overall movement.
† Corrected test items are follow-up items in which the lumbar region is repositioned to achieve a neutral alignment, or movement of the lumbar region is restricted relative to what was observed with the previous symptomatic test item. The effect of the changes in alignment and movement on symptoms is assessed.
‡ Because rotation and side-bending are coupled motions in the lumbar region, items that refer to judgements of alignment and movement of lumbar region rotation or pelvic rotation include side-bending alignment or movement.
There are several unique components to this examination system:
1. The effect of active limb movements on spinal movements and symptoms;
2. The relative timing of movements of the spine and proximal joints during limb and trunk movements;
3. The effect on symptoms of modifying lumbar alignment or movement during repetition of a previously symptomatic test (Van Dillen et al. 2003).
The information obtained from this assessment allows the patient to be categorized into one of five different categories, named after the type of mechanical factors hypothesized to be factors in the contribution of mechanical low back pain (MLBP) (Van Dillen et al. 2003):
Although the classifications are termed lumbar movement impairments, the analysis is technically of the lumbopelvic region. Additionally as discussed in Chapters 1, 2 and 3, not only do proximal regions of dysfunction affect distal segments of the movement system, the lumbar spine refers pain to the pelvis and hip and CPP definitions involve the pelvis, anterior abdominal wall, lower back and/or buttocks (ACOG 2004, Fall et al. 2010).
The musculoskeletal factors that need to be considered include the passive and active stiffness of the lumbopelvic spine and hips which will be influenced by muscle and fascial systems, all under neuronal control. Assessment of the neural system is therefore also critical, as irritability of, and the ability of the nerve trunk to glide along its neural canal, will affect the perceived length of the muscle (Hall et al. 1998; Walsh et al. 2009). Structural differences such as bony variation of the pelvis and femur, imbalances of strength, length, timing and magnitude of recruitment of the trunk and hip muscles will also need to be assessed during test movements, as well as specific functional activities.
1. Lumbar flexion syndrome: the primary dysfunction in this syndrome is that the lumbar spine range of motion into flexion is more flexible than the hip range of motion into flexion. The habitual movement of the individual is towards flexion with spinal movements and movements of the extremities. The spinal alignment tends to be relatively flexed in different postures (Figure 6.1) and symptoms are elicited and/or aggravated when the patient moves towards the flexed position. When movement into flexion is restricted the symptoms are abolished or diminished. The syndrome is more common in individuals between the ages of 18 and 45 and is more common in males. Habitually flexed work postures or repeated forward bending are often reported, and there is increased relative stiffness in the hip extensors (particularly the hamstrings) relative to the erector spinae (Sahrmann 2002).
2. Lumbar extension syndrome: the primary dysfunction in this syndrome is that the lumbar spine range of motion into extension is more flexible than the hip range of motion into extension. Functionally this means that the lumbar spine can extend more readily than the hip extensors can extend the hip (Sahrmann 2002). The hip flexor muscles therefore exert an anterior shear force on the lumbar spine, as well as a forward rotation moment on the innominates bilaterally. The patient’s habitual movement is towards extension with spinal movements and movements of the extremities (Figure 6.2). When movement into extension is restricted the symptoms are abolished or diminished (Sahrmann 2002). The patients are usually over 55 years of age, and there is no reported gender bias. This pattern is often found in patients with acute recurrent low back pain or chronic ongoing low back pain (Sahrmann 2002).
3. Lumbar rotation syndrome: this syndrome describes a three-dimensional dysfunction of a spinal segment. The primary dysfunction is increased lumbar segmental rotation, side-flexion and translation, relative to other spinal segments (Sahrmann 2002) (Figure 6.3). These three motions occur together, due to the complex interaction of the shape of the Z-joint articular surface, the control of the ligamentous restraint systems, and the flexibility of segmental and global muscle system (White & Punjabi 1990). Clinical spinal instabilities usually involve increased arthrokinematic glides, and fit into this group. The rotational stress on the lumbar spine can be produced directly via lumbar spinal rotation/side-flexion/translation or, indirectly, rotation of the pelvis can produce a relative rotation of the lumbar spine segments (White & Punjabi 1990). In certain patients there is an observable rotation of the lumbar spine whilst in others there is no obvious dysfunction (Sahrmann 2002.) The signs and symptoms are similar to those described for lumbar flexion syndrome; however, they are elicited with spinal rotation, and diminished when lumbar rotation is restricted (Van Dillen et al. 2003).
4. Lumbar rotation with flexion: in response to spinal or extremity movement, the patient moves the lumbar spine in the direction of rotation and flexion. The lumbar spine tends to assume a flexed and rotated position in habitual postures. Symptoms are often unilateral, are aggravated by postures involving flexion and rotation and are eased by limitation of flexion and rotation. Symptoms are often aggravated when sitting to standing and functional movements that involve more than one plane (Sahrmann 2002).
5. Lumbar rotation with extension: in response to spinal or extremity movement, the patient moves the spine in the direction of rotation with extension. The lumbar spine tends to assume an extended and rotated position with habitual postures. Symptoms are often unilateral and elicited by extension rotation movements of the lumbar spine (Sahrmann 2002). This syndrome is more common in patients over the age of 55 and with a history of chronic low back and pelvic pain. It is also more common in those individuals who participate in sports that involve significant amounts of torsion in the lumbar spine, e.g. golf, squash, tennis and racquetball (Harris-Hayes et al. 2009).
Common postural types (see Kendall et al. 2005, Sahrmann 2002)
Ideal standing posture (Figure 6.4) can be described as a position where:
• A marker on the lateral tip of the acromion, the midpoint of the greater trochanter, the tip of the lateral malleolus, all line up to form an angle of approximately 180°
• The lumbar lordosis, thoracic kyphosis, and pelvic tilt are in neutral
• Lumbar neutral: the spinal curve should be 20–30°, there should be less than 1.5 cm (1/2″) difference in prominence of the (L) and (R) region 5 cm (2″) lateral from the spinous process
• Pelvis neutral: the line between anterior superior iliac spine (ASIS) and posterior superior iliac spine (PSIS) is within 15° of horizontal line (may vary in women). No lateral tilt or rotation
• Hip neutral: no angle between peak of iliac crest, to greater trochanter to line along thigh
Kyphotic lordotic standing posture (see Figure 6.2B) can be described as a position where:
• A marker on the lateral tip of the acromion, the midpoint of the greater trochanter, the tip of the lateral malleolus, all line up to form an angle greater than 195°, the back is swayed back, the hips swayed forward
• Lumbar lordosis: inward curve increased in depth, greater than 30°
• Thoracic kyphosis: often increased in depth
• Pelvis anterior pelvic tilt: ASIS is 20° lower than PSIS
• Hips flexed: Hip angle of flexion, between peak of iliac crest to greater trochanter, to line along thigh is more than 10°
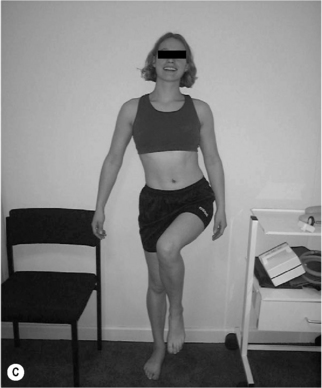
Sway standing posture (Figure 6.5) can be described as a position where:
• A marker on the lateral tip of the acromion, the midpoint of the greater trochanter, the tip of the lateral malleolus, all line up to form an angle less than 165°; the back is swayed back or the hips swayed forward
• Lumbar lordosis: often decreased in length.
• Thoracic kyphosis: often increased in length, shoulders more than 5 cm posterior to greater trochanter
• Pelvis neutral to posterior pelvic tilt: for posterior pelvic tilt, ASIS is 20° higher than PSIS
• Hips extended: hip angle of extension, between peak of iliac crest, to greater trochanter to line along thigh is more than 10°
• Knees hyperextended: backward bowing of knee joint; tibia may be posterior to femur
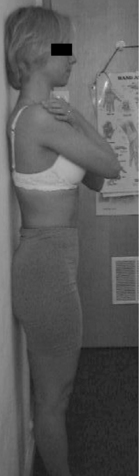
Flat back standing posture (Figure 6.6) can be described as a position where:
• A marker on the lateral tip of the acromion, the midpoint of the greater trochanter, the tip of the lateral malleolus, all line up to form an angle of approximately 180°
• Lumbar lordosis: flat, absent inward curve (may be normal in men)
• Thoracic kyphosis: flat, absent outward curve
• Pelvis neutral to posterior pelvic tilt: for posterior pelvic tilt, ASIS is 20° higher than PSIS
• Hips neutral to extended: hip angle of extension, between peak of iliac crest, to greater trochanter to line along thigh is more than 10°
• Knees neutral to hyperextended: Backward bowing of knee joint, tibia may be posterior to femur
Asymmetry (Figure 6.7): any of the postural shapes above with:
• Paraspinal asymmetry: (L) and (R) paraspinal regions from lumbar spinous processes to 5 cm lateral are greater than 1.5 cm difference in prominence
• Scoliosis/rib hump: ribs more prominent on one side
• Lateral tilt: one iliac crest is more than 1.5 cm higher than other iliac crest (Figure 6.7A,B)
• Rotation: ASIS on one side is anterior to ASIS on other side
• Lateral shift: the pelvis is shifted away from the midline (Figure 6.7C)
Table 6.2 shows the proposed MLBP categories with the associated signs, symptoms and general treatment guidelines. Although it should be stressed that this movement assessment system has not yet been fully validated, the construct validity of the movement impairment-based classification system provided support for three out of the five categories (Van Dillen et al. 2003) and recently the inter-tester reliability based on this classification system has been shown to be substantial (Harris-Hayes & Van Dillen 2009).
Table 6.2 Proposed mechanical low back pain categories with associated signs and symptoms and general treatment guidelines (taken from Van Dillen et al. 2003)![]()
The aim of the assessment is to identify the postural alignment strategies and the habitual movement patterns which may contribute to the individual’s presenting condition. Each syndrome has specific key tests, which help identify the alignment strategies assumed by the individual and confirm the direction of the movement patterns. The patient is then observed during performance of symptom-provoking functional activities, to determine if the same strategies are repeated. Functional instruction is then directed toward modifying the patient’s preferred strategies. Exercise prescription is directed toward correcting the patient-preferred movement and alignment strategies identified on examination. Emphasis is on modifying the strategies that (1) are symptom-provoking and (2) can be modified to decrease the patient’s symptoms during the examination (Van Dillen et al. 2003). This systematic approach is repeated in order to classify movement impairment syndromes of the hip and is described later in this chapter (Table 6.3). It should also be emphasized that, in the authors’ opinion, if the client holds negative beliefs and attitudes associated with pain, such as exhibiting fear-avoidance behaviours without an understanding of current pain biology, the way in which these corrective exercises are explained could contribute to their fear of movement and potentially make their pain problem worse. In this instance, addressing the patients’ attitudes, beliefs and understanding needs to be the therapists’ main priority (O’Sullivan 2005).
Lumbopelvic cylinder and chronic pelvic pain
In the presence of postural changes, respiratory demands, lumbopelvic pain (LPP) and stress incontinence, muscles of the lumbopelvic cylinder (LPC) are altered (Hemborg et al. 1985, Hodges & Richardson 1996, 1998, Hides et al. 1996, Moseley et al. 2002, Hodges & Gandevia 2000, O’Sullivan et al. 2002, Jones et al. 2006, Hodges et al. 2007, Dickx et al. 2008). However, it appears that skilled voluntary activation of muscles with altered motor recruitment can reduce pain, disability and recurrence rate for musculoskeletal conditions (Hides et al. 2001, Cowan et al. 2003, Ferreira et al. 2006), restore motor co-ordination including automatic postural adjustments (Cowan et al. 2003, Tsao & Hodges 2007, 2008), reversing cortical reorganization in people with recurrent pain (Tsao et al. 2010). These findings suggest then, that in addition to the five categories of movement dysfunction described above, muscles of the LPC should be evaluated and rehabilitated, when appropriate, in patients with CPP, although to date there is no scientific trial that has evaluated this clinical approach in this sub-group of chronic pain patients.
The pelvic floor muscles (PFM) form the bottom of the LPC, with the respiratory diaphragm its top, and transversus abdominis (TrA) the sides. The spinal column is part of this cylinder and runs through the middle, supported posteriorly by segmental attachments of lumbar multifidus and anteriorly by segmental attachments of psoas (posterior fasciculii) to the abdominal muscles (Jones 2001). Intra-abdominal pressure (IAP) is generated by co-activation of the PFM, the diaphragm and the abdominal muscles (Hemborg et al. 1985, Hodges & Gandevia 2000), implying that co-ordinated co-activation of the muscles of the LPC is necessary in order to balance the functional demands of continence, respiration and lumbopelvic stability (Hemborg et al. 1985, Hodges & Gandevia 2000, Pool-Goudzwaard et al. 2004, Hodges et al. 2007). Muscles of the LPC work at low levels at all times and increase their activity when the central nervous system can predict timing of increased load, such as occurs in coughing, lifting or limb movements (Constantinou & Govan 1982, Moseley et al. 2002, Barbic et al. 2003). Further details regarding the diaphragm (Chapter 9) and the PFM (Chapter 13) will be found in the appropriate chapters, while the next section describes the assessment and rehabilitation of muscles of the LPC.
Assessment and rehabilitation of muscles of the lumbopelvic cylinder
Voluntary activation of TrA independently from other trunk muscles (Richardson et al. 1999)
• Palpate approximately two fingers’ breadth down from the anterior superior iliac spine (ASIS) along the inguinal ligament, and one finger’s breadth medially
• Ask the patient to breathe in, then on the out-breath to relax and let go of the stomach. Ask the patient to then draw in the low lateral abdominal wall (below the umbilicus) as if to pull the stomach away from the pant (knicker) elastic and breathe normally (Figure 6.8)
• Palpate for a symmetrical tensioning, without excessive bulging, underneath the palpating fingertips, or verify with real-time ultrasound imaging to observe thickening and shortening of the abdominal muscle (Hodges et al. 2003)
• Once the patient can activate TrA with minimal activity of the abdominal muscles, they should hold the contraction, whilst breathing normally, for up to 10 seconds
• Three sets of ten repetitions, twice a day, has been shown to be effective (Tsao & Hodges 2008)
Common substitution patterns or faults
• Movement of the trunk or pelvis out of a neutral position
• Breath holding, apical breathing
• Drawing in of the upper abdominal wall
• Rib cage depression with a decrease of the infrasternal angle
• Lateral flaring or bulging of the waist
• Excessive superior, inferior or lateral movement of the umbilicus
Facilitation techniques for TrA
• Alternative starting positions such as crook lying, 4-point kneeling, side lying, standing, sitting forward lean, prone
• Visualize the lower abdomen as an old-fashioned corset, and as the stays are drawn in, the waist narrows and flattens, into an hourglass shape
• Ensure that the abdomen is relaxed to start with, often easier in sitting or standing forward lean, 4-point kneeling, prone
• Tactile feedback: ask the patient to put one hand above the umbilicus and one hand below, as soon as movement is felt above the umbilicus, drawing in should cease. Tactile feedback: ask patient to palpate you, noting the difference between bulging and tensioning, then to self-palpate
• Facilitation using the PFM which can be particularly useful for asymmetry of contraction (Chapter 13) as can psoas activation (described later)
Assessment and rehabilitation of muscles of the lumbopelvic cylinder
Voluntary activation of pelvic floor muscles (Laycock & Jerwood 2001, Messelink et al. 2005)
Activation and facilitation of PFM
• In a supine, crook lying position with a pillow under the head and legs supported, the International Continence Society (ICS) guidelines to facilitate a PFM contraction are ‘squeeze the muscles of the pelvic floor as if attempting to stop the flow of urine or prevent wind or flatus escaping’ (Messelink et al. 2005)
• Recent research and clinical experience have suggested that the addition of ‘squeeze around the back passage, as if you were trying to prevent breaking wind (flatus), bring that feeling forward towards the urethra/pubic bone and then lift, as if you were elevating the PFM, whilst breathing normally’ elicits a consistent PFM contraction, resulting in a cranioventral lift of the PFM and pelvic organs (Lovegrove Jones 2010)
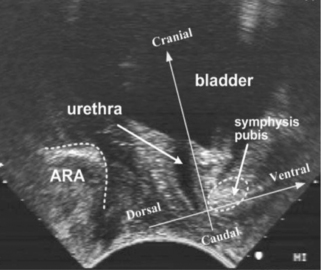
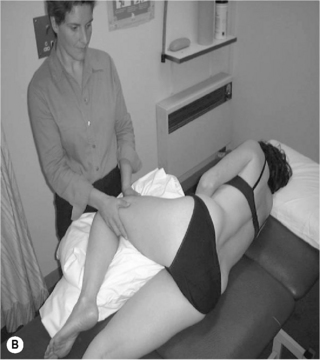
• With consent, confirm the ability of the volunteer to perform an elevating, sustained PFM contraction by vaginal or rectal palpation, real-time perineal (Figure 6.9) or transabdominal ultrasound (Figure 6.10). The patient should have a sensation of a ‘lifting’ rather than ‘bearing down’ contraction, which can also be verified by observation of the perineum ‘lifting’. If verification is not possible in any of the ways described, palpating abdominally, approximately two fingers’ breadth down from the ASIS along the inguinal ligament and one finger’s breadth medially, as in the evaluation of a TrA contraction above, will give an indication of whether co-activation of TrA and the PFM has occurred. Recent evidence has indicated the presence of co-activation in healthy continent and incontinent women (Sapsford et al. 2001, Urquhart et al. 2005, Jones et al. 2006)
• Once the patient can activate the PFM they should hold the contraction whilst breathing normally for up to 10 seconds. The co-ordination of a pelvic floor contraction and normal relaxed breathing seems to be very difficult for some subjects. If this is the case then repeated practice is advised, using low effort. The ability to voluntarily relax the PFM after contraction (Messelink et al. 2005), particularly with PFM overactivity, is essential and the presence of pain on voluntary contraction should be noted (see Chapter 13)


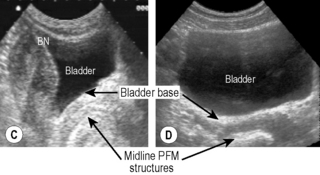
Figure 6.10 • Transabdominal ultrasound transducer placement for (A) sagittal and (B) transverse ultrasound imaging of the bladder. Reproduced from Whittaker (2007) Ultrasound Imaging for Rehabilitation of the Lumbopelvic Region: A Clinical Approach. Typical sagittal (C) and transverse (D) plane transabdominal view of the bladder, bladder base and midline pelvic floor (PF) structures. BN, bladder neck
Voluntary activation of deep segmental lumbar multifidus (Richardson et al. 1999)
• In prone lying (often over a pillow is helpful), palpate the medial paraspinal muscles at each segmental level in turn, just to the side of the lumbar vertebrae and let them sink firmly into the muscle
• Instruct the patient to take a breath in, then on the breath out to relax and let go of the stomach. Slowly and gently hollow and pull up the lower stomach towards the spine, and gently swell the muscles into the palpating fingertips
• Palpate for a symmetrical tensioning, underneath the palpating fingertips or verify with real-time ultrasound imaging to observe thickening of the muscle (Hides et al. 1992)
• Once the patient can activate multifidus they should hold the contraction whilst breathing normally for up to 10 seconds
Facilitation techniques for multifidus
• Visualization of the muscle as deep triangles that extend down and out from each of the spinous processes
• Instruct the patient to feel the contraction on you first, to understand the concept of an isometric swelling contraction
• Other starting positions such as side lying, standing or sitting
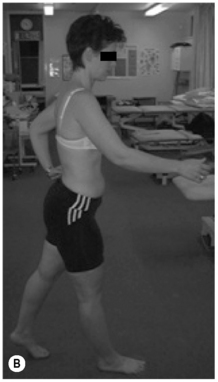
• In standing, move from a position of upright standing to sway, palpating the differences in tension of the medial paraspinals
• In standing, palpate the dysfunctional multifidus with one hand and lift the opposite arm forward and away from the body from 0° to 90°, palpating the superficial fibres changes in tension. Sustain the contraction when multifidus activity decreases. Maintain active muscle tension during slow, repetitive arm flexion. Maintain this multifidus contraction and keep tension in the muscle during slow arm movements with relaxed breathing (Figure 6.11A)
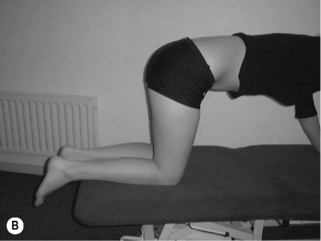
• In walk stance, with full weight on the rear foot, palpate the tension in the dysfunctional multifidus muscle on the rear foot side, and move the body weight forward onto the front foot. Multifidus should activate just after heel lift. Try to sustain the contraction during slow weight transfer with relaxed breathing (Figure 6.11B)
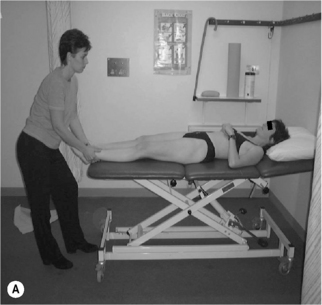
Voluntary activation of the posterior fasciculii of psoas (Gibbons et al. 2002)
Activation and facilitation of the posterior fasciculii of psoas
• With both the lumbar spine and hip in neutral, gently distract the femur in supine or side lying (Figure 6.12). Maintain the distraction and instruct the patient to take a breath in, then on the out-breath to relax and let go of the stomach, whilst slowly and gently drawing in or shortening the hip into the acetabulum without moving the pelvis or lumbar spine. It may be helpful to push the femur into the acetabulum several times to give the sensation of the action required
• Then palpate both the anterior superior iliac spine (ASIS) and the soft tissue below in the anterolateral groin (5 cm below the ASIS). The upper finger assesses for control of movement of the pelvis and maintenance of the lumbopelvic neutral position while the lower finger checks for excessive activity in rectus femoris and sartorius
• Once the therapist is confident that the patient is able to activate the muscle, the patient lies in prone on the plinth with one leg firmly extended to help maintain balance, and the other leg hanging freely over the edge with the foot on the floor. The side with the leg hanging freely is the side to be assessed. In pelvis and lumbar neutral with the trunk muscles relaxed, each lumbar vertebral level is manually palpated to assess the relaxed joint play displacement in the transverse and anterior directions. When the patient then facilitates the psoas contraction, each vertebral level is repalpated to assess the contracted joint play in the transverse and anterior directions. Ideally, there should be a significant palpable increase in resistance to manual displacement (stiffness) at each level
Common substitution patterns or faults
• Movement of the trunk or pelvis out of a neutral position
• Pushing down with the contralateral leg to provide stability for the trunk
• Dominant or excessive activation of rectus femoris, tensor fascia lata or trunk muscles indicated by a resistance to passive rotation of the hip or pelvis. Suggest that the patient uses less effort
Integration of voluntary activation of the lumbopelvic cylinder into function
When muscles of the LPC are working efficiently, voluntary and involuntary activation of any one muscle, should elicit a co-contraction with the others. Although this has been shown with TrA, multifidus and the PFM (Sapsford et al. 2001, Richardson et al. 2002
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree