Monitoring Anesthetic Brain States
Negin Daneshpayeh
Emery N. Brown
I. GENERAL CONSIDERATIONS
General anesthesia is defined as a drug-induced reversible condition composed of unconsciousness, amnesia, analgesia, immobility and stability of the autonomic, cardiovascular, respiratory and thermoregulatory systems. Monitoring behavioral states during general anesthesia is challenging. During general anesthesia, amnesia is not monitored directly but implicitly by the extent to which unconsciousness is achieved.
A. The physiologic signs of changes in heart rate, arterial blood pressure, and movement are the measures most commonly used to track the anesthetic during maintenance of general anesthesia.
B. The changes in heart rate and arterial blood pressure that anesthetized patients show in response to a nociceptive stimulus can be explained in terms of the nociceptive-medullary-autonomic (NMA) circuit, which is comprised of the spinoreticular tract, the brainstem arousal circuits, and the sympathetic and parasympathetic efferent pathways.
1. The ascending nociceptive (pain) pathway begins with A-delta and C-fibers whose free nerve endings bring nociceptive (painful) information from the periphery to the spinal cord.
2. In the spinal cord, these fibers synapse in the dorsal horn on projection neurons that travel through the anterolateral fasciculus and synapse at multiple sites in the brainstem, including the nucleus of the tractus solitarius in the medulla.
a. The autonomic response to a painful stimulus is initiated within the nucleus of the tractus solitarius, which mediates sympathetic output through the rostral ventral lateral medulla and the caudal ventral lateral medulla to the heart and peripheral blood vessels through projections to the thoracolumbar sympathetic ganglia.
b. The parasympathetic output from the nucleus of the tractus solitarius is mediated through the nucleus ambiguus, which projects through the vagus nerve to the sinoatrial node of the heart.
C. Thus, a potentially nociceptive operative stimulus initiates an increase in sympathetic output and a decrease in parasympathetic output through the NMA circuit that rapidly results in the increase in heart rate and arterial blood pressure.
1. The NMA circuit explains why increases in heart rate and arterial blood pressure are used as a rapid indicator of an inadequate level of analgesia.
D. There are several additional approaches for monitoring unconsciousness and analgesia.
1. Electroencephalogram (EEG)-based indices are among the most commonly used methods for tracking altered levels of consciousness induced by general anesthesia and sedation.
II. ELECTROENCEPHALOGRAM-BASED INDICES OF LEVEL OF CONSCIOUSNESS
A. It is recognized that the EEG changes systematically in relation to the dose of anesthetic drug administered. As a consequence, the unprocessed EEG and various forms of processed EEG have been used to track
the level of consciousness of patients receiving general anesthesia and sedation.
the level of consciousness of patients receiving general anesthesia and sedation.
1. Basic Biophysics of EEG
a. The EEG detects postsynaptic potentials in the cerebral cortex. As neurons synapse in a region of the cortex, they produce macroscopic extracellular currents that can be detected as potential differences by surface electrodes. The cortex is tied to subcortical structures like the thalamus.
b. Therefore with the EEG, inferences can be made about both cortical and subcortical dynamics.
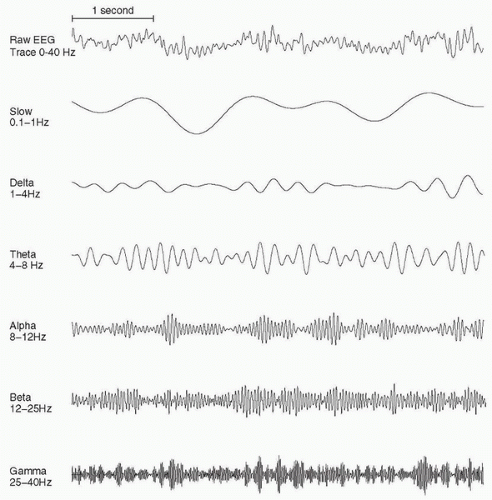
c. The EEG signals are comprised of oscillations or waves with a variety of frequencies.
1. The signal typically consists of many frequencies with different amplitudes (Figs. 11.1 and 11.2).
B. Several EEG-based index systems have been studied and used in clinical practice. These systems process the EEG and provide an index value or set of values in real time or near real time to track the level of consciousness. In general, the indices are designed to decrease with decreasing levels of consciousness and increase as consciousness returns. The anesthesia provider can use these indices along with physiologic signs such as changes in heart rate and blood pressure to track the patient’s state of unconsciousness and to some degree antinociception.
C. Bispectral Index (BIS) is an EEG-based index system. A sensor is placed on the forehead that transmits EEG signals to a digital signal converter, which sends the information to the monitor for processing and analysis.
1. Bispectral Index (BIS)
a. The BIS uses a proprietary algorithm that processes the EEG in near real time and computes an index between 0 and 100 that indicates the patient’s level of consciousness. A value of 100 corresponds to being completely awake, whereas 0 corresponds to a profound state of coma or unconsciousness that is reflected by an isoelectric or flat EEG.
b. Measures specific features of the spectrogram, the bispectrum, and the level of burst suppression and uses a predetermined weighting scheme to convert these features into the index value.
c. Along with the index value, the BIS monitor also displays the unprocessed EEG, the spectrogram, and the level of electromyographic activity.
d. The electromyography indicator displays in decibels the power in the frequency range of 70 to 110 H that is believed to be attributable to muscle activity. The power range is 30 to 55 dB.
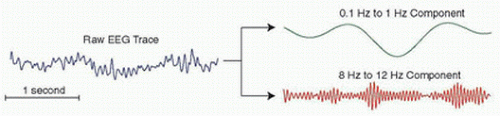 FIGURE 11.1 A typical electroencephalogram trace can be split into a slower oscillatory (0.1 to 1 Hz component [top]) with an overlying higher frequency (8 to 12 Hz component [bottom]). |
e. A patient is considered to be appropriately anesthetized when the BIS value is between 40 and 60.
f. The BAG-RECALL Trial, which focused on patients at high risk for intraoperative awareness, found that patients with BIS-guided general anesthesia experienced a small but statistically significant increase in intraoperative awareness relative to patients receiving general anesthesia guided by an end-tidal anesthetic criterion.
2. Patient Safety Index (PSI)
a. The PSI uses a proprietary algorithm that assesses level of consciousness based on the EEG for patients receiving general anesthesia.
b. Like the BIS, it is also scaled from 0 to 100, but the numeric range to ensure that the patient is unconscious is between 25 and 50.
c. In addition to displaying the numeric value, the PSI monitor also shows the unprocessed EEG in real time with its spectrogram from both the left and right sides of the head, the level of electromyographic
activity, an artifact index, and the suppression ratio which measures the amount of time the EEG is in burst suppression.
activity, an artifact index, and the suppression ratio which measures the amount of time the EEG is in burst suppression.
d. This monitor has been less frequently studied in clinical investigations and has not received the same level of clinical use as the BIS monitor.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree