CHAPTER 120
Monarticular Arthritis, Acute
Presentation
The patient complains of one joint that has become acutely red, swollen, hot, painful, and stiff, with pain on minimal range of motion. Rapid onset with fever and local warmth suggests the possibility of septic arthritis. A prominent monarticular synovitis with comparatively little pain, but where the joint is warm with a large effusion, especially of the knee, is typical of Lyme disease. A migratory tendonitis or arthritis often precedes gonococcal monarthritis. A history of similar attacks, especially of the first metatarsophalangeal joint, suggests the possibility of gouty arthritis. A history of recurrent knee swelling with minimal erythema and gradual onset after overuse or minor trauma is more likely associated with osteoarthritis and pseudogout.
A child between the ages of 3 and 10 years who presents with a limp or inability to walk may have a transient synovitis of the hip or a more serious septic arthritis.
What To Do:
 Ask about previous, similar episodes in this or other joints, as well as trauma, systemic illness, fever, tick bites (Lyme arthritis), sexual risk factors, IV drug use, skin infections, or rashes, and ask about any history of gout (see Chapter 114). Determine the rapidity of onset and the duration of symptoms. Remember that although a high-grade fever is especially concerning, the elderly or immunocompromised patient may fail to mount a fever in the face of infection. General malaise and rash can be associated with infection.
Ask about previous, similar episodes in this or other joints, as well as trauma, systemic illness, fever, tick bites (Lyme arthritis), sexual risk factors, IV drug use, skin infections, or rashes, and ask about any history of gout (see Chapter 114). Determine the rapidity of onset and the duration of symptoms. Remember that although a high-grade fever is especially concerning, the elderly or immunocompromised patient may fail to mount a fever in the face of infection. General malaise and rash can be associated with infection.
 Perform a thorough physical examination, looking for evidence of the above. Obtain cervical, anal, oral, or urethral swabs for culture and Gram stain or DNA probe when you suspect gonococcal arthritis. Cultures of synovial fluid are positive in no more than 50% of patients. Mucosal cultures are positive in 80% of cases.
Perform a thorough physical examination, looking for evidence of the above. Obtain cervical, anal, oral, or urethral swabs for culture and Gram stain or DNA probe when you suspect gonococcal arthritis. Cultures of synovial fluid are positive in no more than 50% of patients. Mucosal cultures are positive in 80% of cases.
 Examine the affected joint and document the extent of effusion, involvement of adjacent structures, and degree of erythema, tenderness, heat, and limitation of range of motion. True intra-articular problems cause restriction of active and passive range of motion, whereas periarticular problems (e.g., prepatellar bursitis, olecranon bursitis), which may mimic joint inflammation, restricting active range of motion more than passive range of motion. Maximum pain at the limit of joint motion is characteristic of true arthritis.
Examine the affected joint and document the extent of effusion, involvement of adjacent structures, and degree of erythema, tenderness, heat, and limitation of range of motion. True intra-articular problems cause restriction of active and passive range of motion, whereas periarticular problems (e.g., prepatellar bursitis, olecranon bursitis), which may mimic joint inflammation, restricting active range of motion more than passive range of motion. Maximum pain at the limit of joint motion is characteristic of true arthritis.
 Intra-articular fluid accumulation can often be detected by pressing on one side of the affected joint and, at the same time, palpating a wavelike fluctuance on the opposite side of the joint. In the knee, when the medial or lateral compartment is stroked, the fluid moves into the opposite compartment, resulting in a visible bulge. To detect effusion in the elbow joint, the triangular recess in the lateral aspect of the elbow, between the lateral epicondyle, radial head, and the olecranon process, should be palpated. To detect effusion in the ankle, the joint should be palpated anteriorly.
Intra-articular fluid accumulation can often be detected by pressing on one side of the affected joint and, at the same time, palpating a wavelike fluctuance on the opposite side of the joint. In the knee, when the medial or lateral compartment is stroked, the fluid moves into the opposite compartment, resulting in a visible bulge. To detect effusion in the elbow joint, the triangular recess in the lateral aspect of the elbow, between the lateral epicondyle, radial head, and the olecranon process, should be palpated. To detect effusion in the ankle, the joint should be palpated anteriorly.
 Although not always necessary, send a blood sample for complete blood count (CBC) and erythrocyte sedimentation rate (ESR), which may support a suspicion of an inflammatory or infectious process. When sepsis is suspected, obtain blood cultures. Blood cultures are positive in about 50% of nongonococcal infections but are rarely positive (about 10%) in gonococcal infection. Serum uric acid measurement is not always helpful and may be misleading. Lyme antibodies may be appropriate as Lyme disease is becoming more and more prevalent, even in the absence of known tick bites. Most patients with Lyme arthritis have positive two-tier serologic tests for B. burgdorferi infection.
Although not always necessary, send a blood sample for complete blood count (CBC) and erythrocyte sedimentation rate (ESR), which may support a suspicion of an inflammatory or infectious process. When sepsis is suspected, obtain blood cultures. Blood cultures are positive in about 50% of nongonococcal infections but are rarely positive (about 10%) in gonococcal infection. Serum uric acid measurement is not always helpful and may be misleading. Lyme antibodies may be appropriate as Lyme disease is becoming more and more prevalent, even in the absence of known tick bites. Most patients with Lyme arthritis have positive two-tier serologic tests for B. burgdorferi infection.
 Consider obtaining radiographs of the affected joint to detect possible unsuspected fractures or evidence of chronic disease, such as rheumatoid arthritis. The finding of crystal-induced chondrocalcinosis could support but not confirm the diagnosis of pseudogout arthritis or osteoarthritis. Occasionally, osteomyelitis or malignancy may be detected. In most cases, radiographs are not helpful in the diagnosis of the acute, nontraumatic, swollen, and painful joint, and they are not always a requirement during the initial evaluation.
Consider obtaining radiographs of the affected joint to detect possible unsuspected fractures or evidence of chronic disease, such as rheumatoid arthritis. The finding of crystal-induced chondrocalcinosis could support but not confirm the diagnosis of pseudogout arthritis or osteoarthritis. Occasionally, osteomyelitis or malignancy may be detected. In most cases, radiographs are not helpful in the diagnosis of the acute, nontraumatic, swollen, and painful joint, and they are not always a requirement during the initial evaluation.
 Perform arthrocentesis to remove joint fluid for analysis, to relieve pain, and, in the case of septic or crystal-induced arthritis, to reduce the bacterial and crystal load within the joint. Identify the joint line to be entered, make a pressure mark on the overlying skin with the closed end of a retractable pen to serve as a target. Then using sterile technique throughout, cleanse the skin over the most superficial area of the joint effusion with alcohol and povidone-iodine (Betadine), anesthetize the skin with 1% plain buffered lidocaine, and aspirate as much joint fluid as possible through a 16- to 18-gauge needle (smaller in small joints). The joint space of the knee (Figure 120-1, A) may be entered medially or laterally with the leg fully extended and the patient lying supine. Hold the needle parallel to the bed surface, and direct it just posterior to the patella into the subpatellar space. The elbow joint (Figure 120-1, B) is best entered at about 30 degrees of flexion, with the needle introduced proximal to the olecranon process of the ulna and just below the lateral epicondyle. Advance the needle medially into the joint space. The best site for needle entry of the wrist is on the dorsal radial aspect at the proximal end of the anatomic snuff box and the distal articulation of the radius. Place the wrist in about 20 degrees of flexion and introduce the needle perpendicular to the skin, advancing it toward the ulna into the joint space (Figure 120-1, C). The ankle joint (Figure 120-1, D) may be entered with the patient supine, the knee extended, and the foot plantarflexed. Find the small depression that is just medial to the extensor hallucis longus and tibialis anterior tendons, inferior to the distal tibia, then direct your needle into the tibiotalar articulation. For small joints, enter the midline on the dorsolateral aspect and advance a small needle into the joint space. Joints of the digits may have to be distracted by pulling on the end to enlarge the joint space. Fluoroscopy may be valuable in guiding needle placement for hip or shoulder joint aspiration.
Perform arthrocentesis to remove joint fluid for analysis, to relieve pain, and, in the case of septic or crystal-induced arthritis, to reduce the bacterial and crystal load within the joint. Identify the joint line to be entered, make a pressure mark on the overlying skin with the closed end of a retractable pen to serve as a target. Then using sterile technique throughout, cleanse the skin over the most superficial area of the joint effusion with alcohol and povidone-iodine (Betadine), anesthetize the skin with 1% plain buffered lidocaine, and aspirate as much joint fluid as possible through a 16- to 18-gauge needle (smaller in small joints). The joint space of the knee (Figure 120-1, A) may be entered medially or laterally with the leg fully extended and the patient lying supine. Hold the needle parallel to the bed surface, and direct it just posterior to the patella into the subpatellar space. The elbow joint (Figure 120-1, B) is best entered at about 30 degrees of flexion, with the needle introduced proximal to the olecranon process of the ulna and just below the lateral epicondyle. Advance the needle medially into the joint space. The best site for needle entry of the wrist is on the dorsal radial aspect at the proximal end of the anatomic snuff box and the distal articulation of the radius. Place the wrist in about 20 degrees of flexion and introduce the needle perpendicular to the skin, advancing it toward the ulna into the joint space (Figure 120-1, C). The ankle joint (Figure 120-1, D) may be entered with the patient supine, the knee extended, and the foot plantarflexed. Find the small depression that is just medial to the extensor hallucis longus and tibialis anterior tendons, inferior to the distal tibia, then direct your needle into the tibiotalar articulation. For small joints, enter the midline on the dorsolateral aspect and advance a small needle into the joint space. Joints of the digits may have to be distracted by pulling on the end to enlarge the joint space. Fluoroscopy may be valuable in guiding needle placement for hip or shoulder joint aspiration.
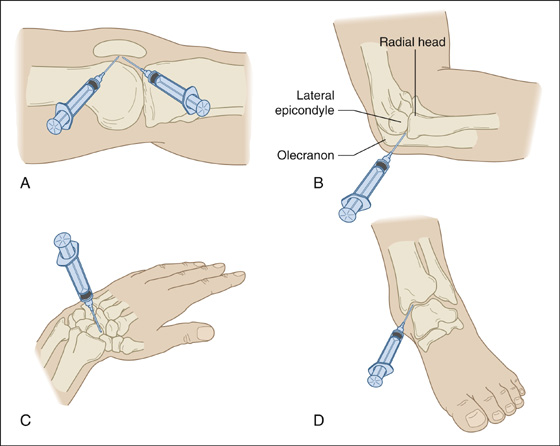
Figure 120-1 Entry sites for arthrocentesis. (A and D, Illustrations provided by Dr. D.H. Neustadt. B and C, Adapted from Akins CM: Aspiration and injection of joints, bursae and tendons. In Vander Salm TJ, Cutler BS, Brownell Wheeler H, editors: Atlas of bedside procedures, ed 2. Boston, 1988, Little Brown & Co.)
 Grossly examine the joint aspirate. Clear, light-yellow fluid is characteristic of osteoarthritis or mild inflammatory or traumatic effusions. Grossly cloudy fluid is characteristic of more severe inflammation or bacterial infection. Blood in the joint is characteristic of trauma (a fracture or tear inside the synovial capsule) or bleeding from hemophilia or anticoagulants. A traumatic tap may cause the serous joint fluid to become bloody during aspiration and is not indicative of a previous hemarthrosis. This procedure can be performed safely in patients who are taking warfarin (Coumadin).
Grossly examine the joint aspirate. Clear, light-yellow fluid is characteristic of osteoarthritis or mild inflammatory or traumatic effusions. Grossly cloudy fluid is characteristic of more severe inflammation or bacterial infection. Blood in the joint is characteristic of trauma (a fracture or tear inside the synovial capsule) or bleeding from hemophilia or anticoagulants. A traumatic tap may cause the serous joint fluid to become bloody during aspiration and is not indicative of a previous hemarthrosis. This procedure can be performed safely in patients who are taking warfarin (Coumadin).
 One drop of joint fluid may be used for a crude string or mucin clot test. Wet the tips of two gloved fingers with joint fluid, repeatedly touch them together, and slowly draw them apart. As this maneuver is repeated 10 or 20 times, and the joint fluid dries, normal synovial fluid will form longer and longer strings, usually to 5 to 10 cm in length. Inflammation inhibits this string formation. This is a nonspecific test but may aid decision making at the bedside.
One drop of joint fluid may be used for a crude string or mucin clot test. Wet the tips of two gloved fingers with joint fluid, repeatedly touch them together, and slowly draw them apart. As this maneuver is repeated 10 or 20 times, and the joint fluid dries, normal synovial fluid will form longer and longer strings, usually to 5 to 10 cm in length. Inflammation inhibits this string formation. This is a nonspecific test but may aid decision making at the bedside.
 If microscopic examinations are delayed, a tube with ethylenediaminetetraacetic acid should be used for anticoagulation, because anticoagulants (e.g., oxalate, lithium heparin) used in other tubes can confound crystal analysis.
If microscopic examinations are delayed, a tube with ethylenediaminetetraacetic acid should be used for anticoagulation, because anticoagulants (e.g., oxalate, lithium heparin) used in other tubes can confound crystal analysis.
 The most important laboratory tests on joint fluid consist of a Gram stain and culture for possible septic arthritis. Gram-positive bacteria can be seen in 80% of culture-positive synovial fluid, but gram-negative bacteria are seen less often; gram-negative diplococci are seen rarely. Polymerase chain reaction techniques can detect gonococcal DNA in the synovial fluid of some culture-negative cases of suspected gonococcal arthritis, but this test is not presently considered a standard evaluation.
The most important laboratory tests on joint fluid consist of a Gram stain and culture for possible septic arthritis. Gram-positive bacteria can be seen in 80% of culture-positive synovial fluid, but gram-negative bacteria are seen less often; gram-negative diplococci are seen rarely. Polymerase chain reaction techniques can detect gonococcal DNA in the synovial fluid of some culture-negative cases of suspected gonococcal arthritis, but this test is not presently considered a standard evaluation.
 A joint fluid total and differential leukocyte count is the next most useful test to order. A count greater than 50,000 white blood cells (WBC)/mm3 is characteristic of bacterial infection (especially when greater than 75% to 90% are polymorphonuclear neutrophils [PMNs]). In osteoarthritis, there are usually fewer than 2000 WBC/mm3, and inflammatory arthritis (such as gout and rheumatoid arthritis) falls in the middle range of 2000 to 50,000 WBC/mm3. One clinical study showed that 36% of patients with septic arthritis had a joint fluid WBC count of less than 50,000/mm3. In a case review of 50 patients with septic arthritis, none had synovial fluid counts of less than 2500 WBC/mm3. Therefore it is reasonable to conclude that when the clinical picture does not suggest infection, and the WBC count is less than 2000 WBC/mm3, empirical antibiotic treatment is not necessary. Also, the presence of greater than 75% PMNs has a good positive predictive value for inflammation/infection and should be treated as infection.
A joint fluid total and differential leukocyte count is the next most useful test to order. A count greater than 50,000 white blood cells (WBC)/mm3 is characteristic of bacterial infection (especially when greater than 75% to 90% are polymorphonuclear neutrophils [PMNs]). In osteoarthritis, there are usually fewer than 2000 WBC/mm3, and inflammatory arthritis (such as gout and rheumatoid arthritis) falls in the middle range of 2000 to 50,000 WBC/mm3. One clinical study showed that 36% of patients with septic arthritis had a joint fluid WBC count of less than 50,000/mm3. In a case review of 50 patients with septic arthritis, none had synovial fluid counts of less than 2500 WBC/mm3. Therefore it is reasonable to conclude that when the clinical picture does not suggest infection, and the WBC count is less than 2000 WBC/mm3, empirical antibiotic treatment is not necessary. Also, the presence of greater than 75% PMNs has a good positive predictive value for inflammation/infection and should be treated as infection.
 There is no clear evidence to guide decision making when the count is between 2000 WBC/mm3 and 50,000 WBC/mm3. Clinical judgment predominates in this range, with an emphasis on presumptive antibiotic treatment until a diagnosis is established. If possible, consult with an orthopedist before antibiotic treatment, because they may want to take the patient to the operating room (OR) prior to starting antibiotics.
There is no clear evidence to guide decision making when the count is between 2000 WBC/mm3 and 50,000 WBC/mm3. Clinical judgment predominates in this range, with an emphasis on presumptive antibiotic treatment until a diagnosis is established. If possible, consult with an orthopedist before antibiotic treatment, because they may want to take the patient to the operating room (OR) prior to starting antibiotics.
 Send a wet preparation to look for crystals. Identification of crystals can establish a diagnosis of gout or pseudogout and avoid unnecessary hospitalization for suspected infectious arthritis.
Send a wet preparation to look for crystals. Identification of crystals can establish a diagnosis of gout or pseudogout and avoid unnecessary hospitalization for suspected infectious arthritis.
 If there is any suspicion of a bacterial infection (based on predisposing factors, fever, elevated ESR, cellulitis, lymphangitis, or the joint fluid results), always treat empirically and start the patient on appropriate intravenous antibiotics based on the results of the Gram stain or the presumptive organism. Adequate treatment should include hospitalization for further IV antibiotics. In older patients, who are not at risk for sexually transmitted diseases (STDs), antibiotic coverage should be aimed at Staphylococcus aureus. Use vancomycin (Vancocin), 1.0 gm IV q12h, along with cefotaxime (Claforan), 1.0 g IV q12h, for uncomplicated infections, or alternatively, use vancomycin with either ceftriaxone (Rocephin), 1.0 or 2.0 g qd IV; ciprofloxacin (Cipro), 400 mg bid IV; or levofloxacin (Levaquin), 500 mg qd IV. For patients with suspected gonococcus, use ceftriaxone (Rocephin), 1.0 g qd IV, or cefotaxime (Claforan), 1.0 g q8h IV. If Gram stain shows gram-positive cocci in clusters, add vancomycin (Vancocin), 1.0 g q12h IV. Provide Chlamydia treatment with azithromycin (Zithromax), 1 g PO × 1, or doxycycline (Doryx), 100 mg bid × 7 days. For children older than 5 years of age, prescribe nafcillin (Unipen) or oxacillin (Prostaphlin), 150 to 200 mg/kg/day divided into 4 to 6 doses, plus ceftriaxone (Rocephin), 50 mg/kg/day (maximum 2 g) divided bid.
If there is any suspicion of a bacterial infection (based on predisposing factors, fever, elevated ESR, cellulitis, lymphangitis, or the joint fluid results), always treat empirically and start the patient on appropriate intravenous antibiotics based on the results of the Gram stain or the presumptive organism. Adequate treatment should include hospitalization for further IV antibiotics. In older patients, who are not at risk for sexually transmitted diseases (STDs), antibiotic coverage should be aimed at Staphylococcus aureus. Use vancomycin (Vancocin), 1.0 gm IV q12h, along with cefotaxime (Claforan), 1.0 g IV q12h, for uncomplicated infections, or alternatively, use vancomycin with either ceftriaxone (Rocephin), 1.0 or 2.0 g qd IV; ciprofloxacin (Cipro), 400 mg bid IV; or levofloxacin (Levaquin), 500 mg qd IV. For patients with suspected gonococcus, use ceftriaxone (Rocephin), 1.0 g qd IV, or cefotaxime (Claforan), 1.0 g q8h IV. If Gram stain shows gram-positive cocci in clusters, add vancomycin (Vancocin), 1.0 g q12h IV. Provide Chlamydia treatment with azithromycin (Zithromax), 1 g PO × 1, or doxycycline (Doryx), 100 mg bid × 7 days. For children older than 5 years of age, prescribe nafcillin (Unipen) or oxacillin (Prostaphlin), 150 to 200 mg/kg/day divided into 4 to 6 doses, plus ceftriaxone (Rocephin), 50 mg/kg/day (maximum 2 g) divided bid.
 Inflammatory arthritis may be treated with nonsteroidal anti-inflammatory drugs (NSAIDs) (unless contraindicated), beginning with a loading dose, such as indomethacin (Indocin), 50 mg, or ibuprofen (Motrin), 800 mg, tapered to usual maintenance doses.
Inflammatory arthritis may be treated with nonsteroidal anti-inflammatory drugs (NSAIDs) (unless contraindicated), beginning with a loading dose, such as indomethacin (Indocin), 50 mg, or ibuprofen (Motrin), 800 mg, tapered to usual maintenance doses.
 If infection can be confidently excluded from the diagnosis, intra-articular injections of corticosteroids can be a useful adjunctive or alternative therapy. Using aseptic technique, prepare the skin with povidone-iodine and alcohol. Using the techniques described above, with a 3- to 5-ml syringe and a 1¼-inch 27-gauge needle, inject 1 to 2 mL of 40 mg/mL methylprednisolone (Depo-Medrol) with 2 to 8 mL of bupivacaine (Marcaine), 0.25% to 0.5%, into the affected joint. For finger or toe joints, use a smaller volume (0.2 to 0.5 mL) of the more concentrated (80 mg/mL) methylprednisolone, along with a lesser volume of bupivacaine. Alternatively, triamcinolone hexacetonide (Aristospan Intra-articular), 20 to 40 mg/injection may be used. Warn patients of the 10% to 15% risk for postinjection flare or recurrent pain for 24 to 48 hours after the local anesthetic wears off.
If infection can be confidently excluded from the diagnosis, intra-articular injections of corticosteroids can be a useful adjunctive or alternative therapy. Using aseptic technique, prepare the skin with povidone-iodine and alcohol. Using the techniques described above, with a 3- to 5-ml syringe and a 1¼-inch 27-gauge needle, inject 1 to 2 mL of 40 mg/mL methylprednisolone (Depo-Medrol) with 2 to 8 mL of bupivacaine (Marcaine), 0.25% to 0.5%, into the affected joint. For finger or toe joints, use a smaller volume (0.2 to 0.5 mL) of the more concentrated (80 mg/mL) methylprednisolone, along with a lesser volume of bupivacaine. Alternatively, triamcinolone hexacetonide (Aristospan Intra-articular), 20 to 40 mg/injection may be used. Warn patients of the 10% to 15% risk for postinjection flare or recurrent pain for 24 to 48 hours after the local anesthetic wears off.
 When joint fluid cannot be obtained to rule out infection, it may be a good tactic to treat simultaneously for infectious and inflammatory arthritis.
When joint fluid cannot be obtained to rule out infection, it may be a good tactic to treat simultaneously for infectious and inflammatory arthritis.
 Splint and elevate the affected joint and arrange for admission or follow-up.
Splint and elevate the affected joint and arrange for admission or follow-up.
 Children complaining of acute hip pain must be evaluated for the possibility of a septic arthritis versus a transient synovitis. Similar symptoms are present in these two diseases at the early stages, and differential diagnosis is difficult. To help differentiate between these two diseases, obtain a CBC, ESR, C-reactive protein (CRP), and hip radiograph.
Children complaining of acute hip pain must be evaluated for the possibility of a septic arthritis versus a transient synovitis. Similar symptoms are present in these two diseases at the early stages, and differential diagnosis is difficult. To help differentiate between these two diseases, obtain a CBC, ESR, C-reactive protein (CRP), and hip radiograph.
 Five reportedly independent predictors of septic arthritis are a temperature greater than 37° C (98.6° F), an ESR greater than 20 mm/h, a CRP greater than 1.0 mg/dL, a WBC greater than 11,000/mm3, and a radiographic joint space difference between the affected and unaffected hips greater than 2 mm. The likelihood of septic arthritis is 0.1% if none of the predictors is present, between 3% and 23% with two variables present, 24% to 77% with three, 82% to 97% with four, and 99.1% if all five predictors are present.
Five reportedly independent predictors of septic arthritis are a temperature greater than 37° C (98.6° F), an ESR greater than 20 mm/h, a CRP greater than 1.0 mg/dL, a WBC greater than 11,000/mm3, and a radiographic joint space difference between the affected and unaffected hips greater than 2 mm. The likelihood of septic arthritis is 0.1% if none of the predictors is present, between 3% and 23% with two variables present, 24% to 77% with three, 82% to 97% with four, and 99.1% if all five predictors are present.
 It may be reasonable to obtain an MRI or fluoroscopically directed joint aspiration in those children with three or four of these predictors.
It may be reasonable to obtain an MRI or fluoroscopically directed joint aspiration in those children with three or four of these predictors.
 When there is a low index of suspicion for a septic hip and there are no contraindications to NSAID use, place the child on ibuprofen (Motrin), 10 mg/kg tid for 5 days. In a small study, this was shown to shorten the duration of symptoms of transient synovitis by 2 days.
When there is a low index of suspicion for a septic hip and there are no contraindications to NSAID use, place the child on ibuprofen (Motrin), 10 mg/kg tid for 5 days. In a small study, this was shown to shorten the duration of symptoms of transient synovitis by 2 days.
What Not To Do:
 Do not tap a joint through an area of obvious contamination, such as subcutaneous cellulitis. Synovial fluid may consequently be inoculated with bacteria. This is considered a relative contraindication to arthrocentesis.
Do not tap a joint through an area of obvious contamination, such as subcutaneous cellulitis. Synovial fluid may consequently be inoculated with bacteria. This is considered a relative contraindication to arthrocentesis.
 Do not send synovial fluid for chemistries, proteins, rheumatoid factor, or uric acid, because the results may be misleading. Synovial fluid glucose is not discriminatory for joint sepsis.
Do not send synovial fluid for chemistries, proteins, rheumatoid factor, or uric acid, because the results may be misleading. Synovial fluid glucose is not discriminatory for joint sepsis.
 Do not be misled by bursitis, tenosynovitis, or myositis without joint involvement. An infected or inflamed joint will have a reactive effusion, which may be evident as fullness, fluctuance, reduced range of motion, or joint fluid that can be drawn off with a needle. It is usually difficult to tap a joint in the absence of a joint effusion.
Do not be misled by bursitis, tenosynovitis, or myositis without joint involvement. An infected or inflamed joint will have a reactive effusion, which may be evident as fullness, fluctuance, reduced range of motion, or joint fluid that can be drawn off with a needle. It is usually difficult to tap a joint in the absence of a joint effusion.
 Do not treat hyperuricemia with drugs that lower uric acid levels, such as allopurinol or probenecid, during an acute attack of gout (see Chapter 114).
Do not treat hyperuricemia with drugs that lower uric acid levels, such as allopurinol or probenecid, during an acute attack of gout (see Chapter 114).
 Do not inject corticosteroids into a joint until infection has been ruled out.
Do not inject corticosteroids into a joint until infection has been ruled out.
 Do not use NSAIDs when a patient has a history of active peptic ulcer disease with bleeding. Relative contraindications include renal insufficiency, volume depletion, gastritis, inflammatory bowel disease, asthma, hypertension, and congestive heart disease.
Do not use NSAIDs when a patient has a history of active peptic ulcer disease with bleeding. Relative contraindications include renal insufficiency, volume depletion, gastritis, inflammatory bowel disease, asthma, hypertension, and congestive heart disease.
 Do not start maintenance NSAID doses for an acute inflammation. It will take 1 day or more to reach therapeutic levels and pain relief. When tolerated, always start with a loading dose.
Do not start maintenance NSAID doses for an acute inflammation. It will take 1 day or more to reach therapeutic levels and pain relief. When tolerated, always start with a loading dose.
Monarticular joint disease (especially monarthritis) should be regarded as infectious until proven otherwise. Infectious arthritis requires prompt treatment to prevent joint destruction and spread of infection.
It should be kept in mind, however, that any polyarticular disease, such as rheumatoid arthritis or systemic lupus erythematosus, can initially present in a single joint and later be revealed to occur in other joints.
The acute, swollen/painful joint is most commonly caused by trauma, infection, or crystal-related disease. Trauma is the most common cause, followed by infection. Gout is the most common crystal-associated arthropathy.
Most acute bacterial arthritis is monarthritis, but polyarticular infectious arthritis occurs in approximately 12% to 20% of cases. The infectious cause varies according to patient factors, particularly age and sexual activity. Staphylococcus aureus is cited as the most common cause of infectious monarthritis in adults. Neisseria gonorrhoeae is the most common cause of acute monarthritis in young, sexually active adults. It is three to four times more common in women than in men. Neonates and children are at higher risk for group B streptococcus, S. aureus, Escherichia coli, and other gram-negative organisms.
Risk factors for septic joint include skin infection, prosthetic joint, joint surgery, rheumatoid arthritis, age older than 80 years, and diabetes. Also, intravenous drug abuse allows organisms to access joints, such as the sternoclavicular joint, which is uncommonly thought of in infectious arthritis.
Gout and pseudogout can present with abrupt onset of pain and effusion, raising suspicion of infection. When the history reveals longstanding symptoms in a joint, with exacerbations of preexisting disease (e.g., gout, or worsening of osteoarthritis with excessive use), this still should be differentiated from a new superimposed infection.
In patients with rheumatoid arthritis, pain in one joint out of proportion to pain in other joints always suggests infection.
Intra-articular trauma is more likely than extra-articular trauma to present as acute monarthritis; fracture, meniscal tears, and other internal derangements (e.g., ligament tears) are common forms of intra-articular trauma.
The history of trauma is a potential pitfall in the approach to the patient with acute monarthritis. Although some patients with a traumatic cause may be unable to recall the event, others falsely and inadvertently attribute their joint pain to a relatively minor injury. Clinically, the physical examination of a patient with traumatic acute monarthritis may be indistinguishable from crystal deposition and infectious disease. In fact, trauma can be the precipitant of crystal deposition and infection.
Synovial fluid aspiration is universally recommended in the patient with acute monarthritis. The urgent reason for tapping a joint effusion is to rule out a bacterial infection, which could destroy the joint cartilage in as little as 1 or 2 days. Beyond identifying an infection (with the Gram stain, culture, and WBC), further diagnosis of the cause of arthritis is not particularly accurate, nor is early definitive diagnosis necessary to decide on specific acute treatment.
Reducing the volume of the effusion may alleviate pain and stiffness, but this effect may be short lived, because the effusion may reaccumulate within hours.
Identification of crystals is essential for the diagnosis of gout or pseudogout, but one acute attack may be treated in the same manner as any other inflammatory arthritis. The workup for an exact diagnosis may, therefore, be deferred to follow-up after acute infection has been ruled out.
Infants and young children may present with fever and reluctance to walk from septic arthritis of the hip or knee, and arthrocentesis may require sedation or general anesthesia.
Acute arthritis in prosthetic joints is always of concern. Infections in prostheses are disastrous and require urgent consultation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


