Chapter Seven Modalities working with massage
Chapter contents
In this chapter a number of modalities that integrate well with massage therapy will be discussed. To support proficiency, practical examples and skill enhancement exercises are included. Let’s begin by reviewing concepts from previous chapters.
Massage and pain management
Let us summarize the application of massage to target pain.
Acute pain and chronic pain are managed somewhat differently; therefore it is important to make the distinction between the two. Intervention for acute pain is less invasive and focuses on supporting a current healing process. Chronic pain is managed with either symptom relief or a more aggressive healing and rehabilitation approach that incorporates a therapeutic change process.
Pain management massage strategies
Massage application targeted to pain management incorporates the following principles:
1. General full-body application with a rhythmic and slow approach as often as feasible with 45–60 minute durations.
Goal – Parasympathetic dominance with reduced cortisol.
2. Pressure depth is moderate to deep with compressive broad based application. No poking, frictioning, or application of pain-causing methods.
Goal – Serotonin and GABA support and reduced substance P and adrenaline.
3. Drag is slight unless connective tissue is being targeted. Drag is targeted to lymphatic drain and skin stimulation.
Goal – Reduce swelling and create counterirritation through skin stimulation.
4. Nodal points on the body that have a high neurovascular component are massaged with a sufficient depth of pressure to create a ‘good hurt’ sensation but not defensive guarding or withdrawal. These nodal points are the location of cutaneous nerves, trigger points, acupuncture points, reflexology points, etc. The foot, hands, and head, as well as along the spine, are excellent target locations.
Goal – Gate control response, endorphin and other pain-inhibiting chemical release.
5. Direction of massage varies, but deliberately targets fluid movement.
6. Mechanical force introduction of shear, bend, torsion, etc. are of an agitation quality to ‘stir’ the ground substance and not create inflammation.
Goal – Increased tissue pliability and reduced tissue density.
7. Mechanical force application of shear, bend, and torsion is used to address adhesion or fibrosis but needs to be specifically targeted and limited in duration.
Goal – Reduce localized nerve irritation or circulation reduction.
8. Muscle energy methods and lengthening are applied rhythmically, gently, and targeted to shortened muscles.
Goal – Reduce nerve and proprioceptive irritation and circulation inhibition.
9. Stretching to introduce tension force is applied slowly, without pain and targeted to shortened connective tissue.
Goal – Reduce nerve and proprioceptive irritation.
10. Massage therapists are focused, attentive, compassionate, but maintain appropriate boundaries.
Goal – Support entrainment, bioenergy normalization, and palliative care.
Now that the massage application and mechanisms have been described, what else can be done?
Remembering adaptation
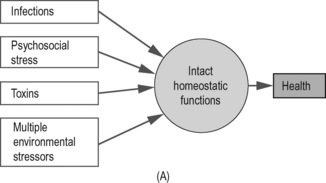
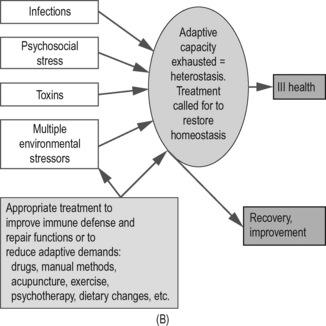
1. All health problems can benefit from reducing the adaptive load(s) being coped with, i.e. all the stresses of living, whether these are:
2. Additionally all health problems benefit from improved functionality – better circulation, mobility, strength, neural function, breathing, balance, posture, etc.
3. If the overall adaptive load is reduced, and/or if functions are improved, the self-regulating/self-repair systems and mechanisms of the body will be able to operate more effectively.
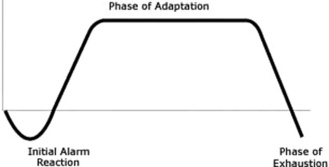
General adaptation sequence (see fig. 7.2)
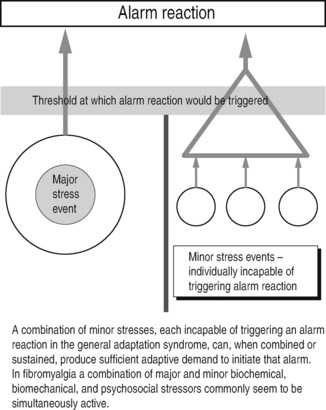
• An initial Alarm stage. An example of this is the ‘fight or flight’ (sympathetic arousal) response that might be triggered by a single stress event, or by a number of minor stressors acting simultaneously (see Fig. 7.2). If the stressor(s) continue to operate the body’s defense mechanisms move to what is known as:
• The Adaptation phase which continues until the ability of the body to compensate further is exhausted. This can be expressed as homoeostatic exhaustion, or a stage of heterostasis, where adaptation potential fails (think of a piece of elastic that has been stretched until it starts to fray, and eventually snaps). When this occurs we have reached:
• The Stage of exhaustion. The individual’s self-regulating/self-repair potentials will be exhausted (or severely strained) and chronic symptoms and frank disease follow. At this stage homoeostatic mechanisms may fail, decompensation features emerge, and treatment to slow, modify, or reverse the process is called for (Fig. 7.4).
Therapeutic choices available are limited to those that:
What helps?
Those that will be considered, later in this chapter, in relation to pain include:
• acupuncture (what you should know about this)
• high velocity manipulation (what you should know about this)
• lifestyle changes, including nutrition, exercise
Scope of practice limitations may not allow all massage therapists to utilize some of these methods, or to advise clients/patients specifically – for example, about nutritional influences on their symptoms; however, knowledge of these topics is important, so that at the very least, if they seem to apply in any given case, appropriate referral can be made. See Chapter 9 for more specific information on these methods.
General objectives based on an understanding of the adaptation process
1. To identify and help the individual to reduce the adaptive demands – the habits of life that are helping to create (or aggravate, or maintain) the dysfunctional state that allows minor trigger factors to activate the symptoms.
2. To enhance functionality by improving posture, breathing, mobility, etc.
3. To ease symptoms without adding to the person’s adaptive burden, emphasizing the importance of remaining aware of just how sensitive and vulnerable this person is.
4. To support self-repair, self-regeneration, self-healing processes.
5. To take account of the whole person, the lifestyle, habits, attitudes, and behavior – and not just the symptoms.
6. To keep in mind that the more complex the condition, and/or the more sensitive and unwell the individual is, the less that should be done therapeutically at any given time.
7. To try to focus on causes – and, above all…
Interacting causes
• In such cases what’s the real cause of pain?
• Is the trigger really a ‘cause,’ or is it just a final straw?
• Sensitization: as tissues respond to a variety of ongoing, or periodic, adaptive demands a degree of sensitization may occur, allowing minor stress factors (of any sort) to provoke pain. This feature of what is known as central sensitization is common to all forms of chronic pain and is discussed later in this chapter (Bendtsen et al 1996).
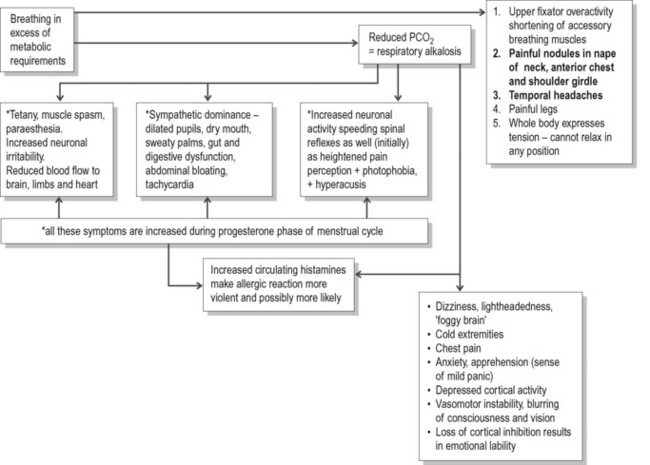
• Breathing pattern disorders: the common habit of upper chest breathing imposes physical stress (overuse) on the accessory breathing muscles, such as the scalenes, SCM, upper trapezius, as well as producing a wide range of biochemical and emotional changes (Fig. 7.5).
The sensitization model
Bendtsen (2000) has described a process of central sensitization (facilitation) that occurs after prolonged bombardment of pain messages from pain receptors (nociceptors) in myofascial tissues. At its simplest this means that nerves have become hyperirritable, so that even minor stimuli, that would previously not have caused any discomfort, can lead to a great deal of pain. This does not mean that the person is imagining the pain, but that the sensations reaching the brain are interpreted as being far stronger than would be the case under ‘normal’ conditions, before sensitization.
Once they exist, areas of facilitation/sensitization appear to be capable of being irritated by stressors of all types – physical, chemical, or psychological – even if there is no direct or obvious impact on the sensitized area (Bendtsen & Ashina 2000).
Example
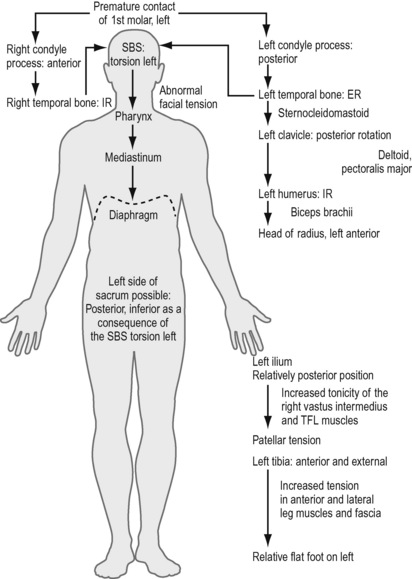
Liem (2004) has explained a sequence that results from a degree of malocclusion, involving, as an example, the first molar on the left, where premature contact occurs on bringing the teeth together.
Figure 7.6 shows something of the chain reaction of adaptations resulting from this apparently minor structural imbalance, in which cranial modifications absorb the stresses of this dental misalignment, followed by bodywide muscular and fascial adaptations that also include osseous changes involving the left clavicle, humerus, radius, ilium, patella, tibia, and foot.
Janda’s example of adaptation and facial pain
Janda (1982) describes a typical postural pattern, in an individual with TMJ problems, involving changes in upper trapezius, levator scapulae, scalenii, sternocleidomastoid, suprahyoid, lateral and medial pterygoid, masseter, and temporalis muscles. In this pattern (described below) all these muscles will show a tendency to tighten and/or to develop tendencies to spasm, tenderness, and the evolution of trigger points.
The postural pattern associated with TMJ dysfunction might therefore involve:
1. hyperextension of the knees
2. increased anterior tilt of the pelvis
5. rounded shoulders and winged (rotated and abducted) scapulae
7. compensatory overactivity of upper trapezius and levator scapulae
8. forward head position resulting in opening of the mouth and retraction of the mandible
9. intervertebral joint stress in the cervical spine
What’s to be done?
In any given case your role is to try to identify what can be done to help ease the current pain symptom (see previous chapters, and also Box 7.1), as well as what might be done, or what the person might do, to reduce the likelihood of further symptomatic episodes.
Box 7.1 Soft tissue modalities in a clinical management sequence
1. Identify local and general imbalances that may be contributing to the symptoms being presented (posture, patterns of use, local dysfunction).
2. Identify, relax, and stretch overactive, tight muscles, using massage and possibly muscle energy techniques (MET), positional release techniques (PRT), myofascial release techniques (MRT and others).
3. Mobilize restricted joints (possibly using MET, PRT).
4. Facilitate and strengthen weak muscles.
5. Reeducate (exercises, training, etc.) movement patterns, posture, and/or breathing function.
This sequence is based on sound biomechanical principles (Jull & Janda 1987, Lewit 1999) and serves as a useful basis for care and rehabilitation of the patient with musculoskeletal problems that may be contributing to pain. A variety of soft tissue normalization methods can be incorporated into this model (Greenman 1989, DiGiovanna 1991).
In these examples, using a biomechanical model of care, incorporating massage and appropriate soft tissue modalities (see Box 7.1) and rehabilitation strategies (posture, breathing, etc.) should certainly help to alter/improve the soft tissue status, enhance circulation and lymphatic drainage, and, if appropriate, assist in the deactivating of trigger points that may be contributing to pain.
A broader model of care
The biomechanical model outlined in Box 7.1 is one way of managing such problems. Other proposed models for effective care of musculoskeletal dysfunction incorporate somatic, as well as behavioral features. For example, Langevin & Sherman (2006) have described a model in which a broader therapeutic approach to musculoskeletal dysfunction in general can be understood.
In this way long-term preventive approaches might also include:
• Enhanced standing, sitting and sleep postures.
• Greater care over work and leisure activity postures and positions (ergonomics); for example, consider the often prolonged periods of distorted or strained positioning involved in people working in dentistry, hairdressing, construction, massage, house-painting, automobile repair, plumbing, gardening, nursing, home-making, running, jumping, throwing, climbing, etc. Consider also that in such situations repetitive, and/or prolonged, stresses may be being loaded onto already compromised tissues, which may have become shortened and/or weakened, fibrotic, indurated, or in some other way dysfunctional, long before current stress patterns were imposed.
• Breathing rehabilitation strategies.
• Stress management (see Box 7.2), including learning relaxation techniques.
• Counseling or psychotherapy, if appropriate.
• Mobilization of restricted spinal structures and joints of the limbs – including self-help measures (see below).
• Stretching shortened associated musculature – including self-help measures (see below).