Minor Trauma
Richard Bachur MD
LACERATIONS AND ABRASIONS
Anatomy, Physiology, and Pathology
The three layers of skin include the epidermis, dermis, and subcutaneous layer. The epidermis, which has no blood vessels, protects the dermal layer from infection and desiccation. The dermis provides the tensile strength of the skin and contains capillary blood vessels. The subcutaneous layer contains loose connective tissue, fat, and the large vessels and nerves.
The term abrasion is used for superficial defects of the skin in which the outer layers have been scraped away. The most superficial abrasions involve loss of the epidermis, leading only to transudation of serous fluid but no bleeding. Deeper abrasions into the dermis will cause bleeding. Laceration implies a cut through the skin: superficial lacerations in the epidermis will not bleed, those into the dermis will have capillary bleeding, and lacerations into the subcutaneous layer will gape open and can have substantial bleeding.
Wound healing occurs in defined stages: coagulation, inflammation, proliferation, and maturation. Coagulation occurs immediately at the time of injury. First, the platelets adhere and form plugs. Second, the extrinsic clotting system is activated, leading to fibrin deposition. Inflammation, by polymorphonuclear cell migration, occurs within hours for defense against bacteria. As a result of chemotactic factors released by platelets, monocytes migrate to the area and, over days, clean up necrotic tissue and foreign material through phagocytosis. The macrophages also stimulate proliferation of surrounding fibroblasts. Myofibroblasts apply a collagen matrix that enables wound contraction. This proliferation phase is clinically seen as beefy red granulation tissue composed of macrophages, proliferating fibroblasts, and growing capillaries. As this process heals the dermal layer, reepithelialization of the epidermal layer occurs. Fibrin deposition and reorganization takes weeks to months to complete. During that time, the wound stays erythematous as a marker of ongoing healing.
Good nutrition, including adequate amounts of protein and vitamins A and C, optimizes wound healing. Several drugs interfere with healing: aspirin inhibits the coagulation phase, steroids inhibit cellular immunity and reepithelialization, and chemotherapeutic agents affect the number and function of white blood cells.
Management
Initial Approach to Lacerations
Providers should approach all lacerations in the context of the whole patient with regard to prioritizing the evaluation of other potentially more serious injuries. They can obtain hemostasis with direct pressure using a sterile dressing. Rarely will a patient require a tourniquet. The provider should question the patient about the details of the injury (time, mechanism), any pertinent past medical history, current medications, medication allergies and prior exposures to local anesthetics, tetanus status, possibility of foreign bodies in the wound, and paresthesias or weakness.
The clinician should inspect the wound for size and depth (this often requires the removal of dry blood on the skin), the condition of the skin edges, the presence of a foreign body, and the potential involvement of underlying structures including arteries, nerves, tendons, ligaments, and bones. Accurate inspection may require local anesthesia (with or without restraint or sedation); however, the provider needs to determine neurologic function and vascular status prior to anesthetic administration. He or she needs to do probing and deep inspection under sterile conditions. Proper inspection cannot occur without hemostasis and good lighting. In cases of suspected foreign body or injury of underlying bone, the provider should obtain a radiograph. When he or she cannot close wounds immediately, the clinician should apply saline-soaked gauze to prevent retraction and desiccation of the wound edges.
The clinician should clean surrounding skin with an antiseptic solution and irrigate the wound with sterile saline under pressure. Pressure irrigation is best achieved with a ready-made irrigation device or simply by connecting a 50 cc syringe to a 20 g intravenous (IV) catheter. The minimum volume for irrigation is 200 cc; considerably more is necessary for large or dirty wounds. The clinician should wear proper eye and face protection. After irrigation, he or she must carefully explore the wound, debride the edges, and formulate a strategy for closure. The provider must avoid extensive debridement, especially in cosmetic areas. If closure will be delayed, the clinician should apply a moist dressing and keep the wound elevated.
Wound Repair
Repair of lacerations is done to reduce the risk of infection and to hasten healing. Ideally, wounds are closed within 6 hours following the injury, although providers must give individual consideration to location, likelihood of contamination, and vascular supply of the area. Clinicians can treat most lacerations without subspecialty consultation but need to consider their own level of experience, the wound’s location and complexity, and the patient’s need for sedation. Providers should consider consultation under the following conditions:
Potential or definite injury to nerve, tendon, ligaments, or bone
Need for conscious sedation or general anesthesia to properly repair the wound
Stellate lacerations or other complicated wounds (because of jagged or complex edges or wound tension)
Highly cosmetic injuries (eg, flaps, vermilion border of the lips, animal bites to the face)
Many small wounds can be successfully anesthetized with local, topical anesthesia such as LET (lidocaine, epinephrine, and tetracaine) or TAC (tetracaine, adrenaline, and cocaine). The latter, however, requires refrigeration and management of a controlled substance. Larger wounds require injections of lidocaine locally or a nerve block. Providers should not inject epinephrine into areas of end circulation or cartilage.
Clinicians should not use topical anesthesia with epinephrine near mucosal surfaces or areas of end circulation or cartilage (ie, digits, tip of nose, penis, and pinna).
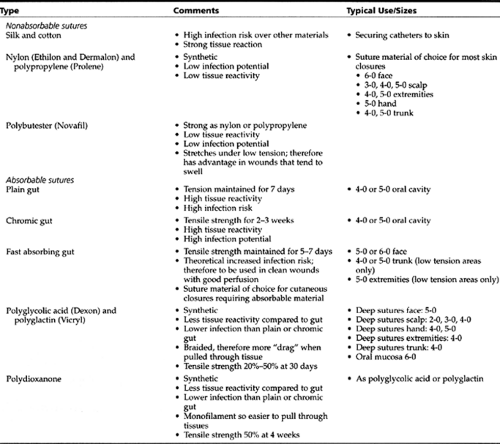
The mechanics of suturing are beyond the scope of this text, but a few principles can be expressed. If deep (“buried”) sutures can be placed, then they should be placed. Providers should close all cavities or dead space or place a drain to avoid infection created by fluid collecting in the space. All buried sutures should be absorbable suture materials. Cutaneous closure can be either absorbable or nonabsorbable; however, absorbable sutures cannot be used for skin closure in wounds under tension (such as those over joints). If absorbable sutures are to be used for cutaneous closure, clinicians should use the fast-absorbing variety to avoid prolonged inflammation and, therefore, increased scarring. The varieties of suture and their uses are presented in Table 43-1.
Removal of Sutures
The timing of removal of nonabsorbable sutures is based on wound condition, vascularity of the region and wound, presence of tension across the wound, and cosmetic importance. Sutures are typically removed after 5 days for the face, 7 days for the scalp, 7 to 10 days for the torso, and 10 to 14 days for the extremities. Wounds over joints or under tension may require skin tapes and prolonged immobilization after suture removal. In general, infection rates and scarring at the suture entry points increase with time. Additionally, providers may need to delay suture removal under conditions of poor perfusion or high tension (although they should watch the wound carefully for infection).
Alternatives to Sutures
Skin Tape
Providers can use skin tapes (Steri-Strips, Shurstrips, and Clearon) to repair superficial lacerations or to provide skin closure on a wound approximated with deep sutures. Tape is not useful in areas under tension (eg, over joints), areas likely to get wet, or in young children who are more likely to remove them. Clinicians should use tape only after they have cleaned and explored the wound and the edges are dry. The tape will not adhere to moist skin. Applying benzoin can markedly approve its adherence. Providers must instruct parents to keep the wound dry and to allow the tape to self-detach.
Skin Staples
Staples are readily available in disposable units and are particularly good for small scalp lacerations. Providers can place staples much more rapidly than they can sutures. Certainly, staples require less equipment than sutures. Placement of staples can often be done with local, topical anesthesia. Because of the potential of scarring, providers should not apply staples to the face.
Tissue Adhesives
Adhesives have recently become available and are as good as sutures in small, simple, clean lacerations (Bruns, 1996). Adhesives are not only faster but also less painful. Evaluation and cleaning of the wound is still very important; therefore, the patient may still require local anesthesia for proper cleaning even if he or she does not need it for wound closure. Because it is fast drying, application around the eye and mouth must be done carefully. Clinicians should carefully read recommendations related to use, including time of drying, number of layers, avoidance of drips, and follow-up care. The manufacturer also offers techniques to undo mistakes. Providers should contact an ophthalmologist for eye exposures.
Follow-up Care
Following initial management of the wound, the provider must give the patient instructions related to wound care, dressing changes, follow-up (eg, suture removal), and reasons to return. In general, dressings should be changed daily unless otherwise specified by the person who cared for the wound. For small wounds, dressings may be unnecessary, or parents can simply apply a smear of antibiotic ointment. Larger wounds require a non-adherent dressing (Xeroform, Adaptic) against the wound, a layer of gauze to “sponge away” any drainage, and an outer wrap to guard against dirt and to secure the dressing.
• Clinical Pearl
Prophylactic antibiotics are not part of routine wound management but may be indicated in certain situations such as dirty wounds, wounds older than 12 hours prior to repair, punctures, bite wounds, exposure of bone, involvement of tendon sheaths, or host factors such as poor circulation or immunodeficiency.
BURNS
Most burns in pediatric patients occur at home and are accidental but preventable. Children younger than age 4 years are at greatest risk because of their curiosity and mobility. Only 3% to 5% of burns are life threatening (often secondary to house fires). Eighty percent are minor burns secondary to scalds.
Burn prevention is as important as the wearing of seatbelts and bike helmets. Simple interventions such as decreasing the temperature of water heaters to 120°F, installing smoke detectors and sprinklers, using flame retardant upholstery, and conducting anti-smoking campaigns can have a huge impact on public safety.
Children with burns may present directly to an emergency room or medical office. As described in the following section, providers can care for most minor burns in the office.
Pathology
The skin acts as a barrier to infection, regulates water loss and temperature, and provides sensory information. The outer, non-living layer is termed the epidermis, and the undersurface is termed the dermis. The dermis includes blood vessels, nerves, hair follicles, secretory glands, and sweat glands, all of which are necessary for repair of damaged skin.
History and Physical Exam
Superficial burns (first-degree) affect only the epidermis; typically, redness and pain are the only signs (sunburns are the most common example). They heal in 3 to 5 days with or without peeling. Partial-thickness or second-degree burns extend into the dermis. Superficial second-degree burns involve the epidermis and up to half of the dermis. Increased capillary permeability leads to a moist appearance, often with blister formation and edema. Healing occurs in about 2 weeks, and scarring is minimal. Deep second-degree burns extend through most of the dermis. They tend to be paler and drier compared to more superficial burns. Thrombosed blood vessels may give a speckled appearance to the skin. Pain may be less than with superficial burns secondary to injury to nerves. Healing may take weeks to months with risk of hypertrophic scars. Full-thickness or third-degree burns involve destruction of the epidermis and entire dermis. The burn may have a pale or charred color and a “leathery” appearance. Destruction of nerves in the dermis makes the area anesthetic. The edges may not be full-thickness and therefore may be a source of pain. With all the dermal elements gone, the skin cannot regenerate except at the edges. These burns often require skin grafting. Burns may be considered fourth-degree with the involvement of fascia, muscle, or bone.
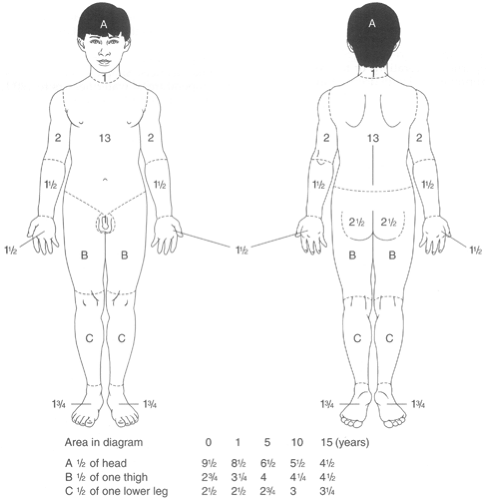
The severity of the burn depends on the burn source (eg, radiation, thermal, chemical, electrical), the size of the burn area relative to the body size [percent body surface area (BSA)], the depth, and the location. The “rule of 9s” estimates the body surface area in adults: head and neck (9%), anterior trunk (18%), posterior trunk (18%), each leg (18%), each arm (9%), and anorectal area (1%). In children, the head is larger relative to the body and changes by age; therefore, providers cannot use simple rules (see Figure 43-1). In general, the size of a child’s palm is roughly equivalent to 1% BSA.
Minor burns are defined as all first-degree burns, second-degree burns that cover less than 10% BSA in children younger than age 6 years, and second-degree burns that cover less than 15% BSA in older children and adults. Exceptions are burns that may cause loss of function or deformity (eg, burns over joints or circumferential burns), pose an infection risk, or involve the face, hands, feet, or perineum.
Moderate burns involve 10% to 20% BSA if second-degree and 2% to 10% if third-degree. Burns are classified as major
if second-degree and involving greater than 20% BSA, third-degree and involving greater than 10% BSA, or second- or third-degree and circumferential or crossing flexor creases. Additionally, burns are considered major when associated with the following: inhalational injury, electrical burn (see below), fractures or other major trauma, in patients with significant pre-existing medical conditions, or with suspected child abuse.
if second-degree and involving greater than 20% BSA, third-degree and involving greater than 10% BSA, or second- or third-degree and circumferential or crossing flexor creases. Additionally, burns are considered major when associated with the following: inhalational injury, electrical burn (see below), fractures or other major trauma, in patients with significant pre-existing medical conditions, or with suspected child abuse.
Management
Providers can manage all minor burns on an outpatient basis. Moderate burns often require hospitalization and consultation with a burn specialist. The decision to hospitalize is determined by the need for IV fluid therapy, pain control, need for close observation, or suspicious circumstances. Second-degree burns covering more than 10% BSA in an infant or 20% BSA in a child may require IV fluids to prevent dehydration. A specialist (eg, plastic surgeon) should manage all full-thickness burns and partial-thickness burns that are circumferential, cross joints, or involve the face, perineum, hands, or feet.
Initial Management of Minor and Moderate Burns
First-degree burns do not need special attention other than pain control with over-the-counter pain relievers (topical and oral). For partial-thickness and full-thickness burns, providers must prepare the wounds. They should remove clothing from the area. Initial care involves gentle irrigation with cool saline for pain control and to remove any dirt, debris, and dead skin. Clinicians must irrigate chemical burns extensively (they can place a small child in a sink or tub for this purpose). Pain control with narcotics may be necessary for adequate care. Providers also may use topical anesthetics such as viscous lidocaine for small burns (use in large burns can lead to toxicity). They can debride loose and necrotic skin, including flaccid blisters, with a forceps and scissors. Gentle wiping with saline-soaked gauze is quite effective for removing non-viable tissue. Providers should leave eschars, seen with deep partial-thickness and full-thickness burns, undisturbed. They should not try to remove any tar from wounds at the initial visit. They should leave blisters intact if fresh (less than 2 hours old). Large blisters (> 5 cm), flaccid or ruptured blisters, and any size blister crossing a joint are best debrided during the initial care. After debridement and irrigation, the provider should pat the wound dry with gauze.
Providers can manage burns in several different ways. The open method basically allows the burn to be its own dressing—whether it has a blister or eschar. A topical antibacterial ointment is applied to the open wound several times per day. Because children cannot be trusted to keep wounds clean, the open method is rarely used except in very small burns or in areas that are difficult to dress, such as the face. The closed
method of care applies gauze dressing after the wound is prepared. Antibacterial cream, such as silver sulfadiazine (avoid if sulfa allergy, G6PD) or bacitracin/polymixin B, is applied to the thickness of a tongue blade then covered with gauze sponges loosely held by tape or some form of wrap. Alternatively, the antibacterial cream may be applied first to the gauze. For burns of the hands and feet, gauze may be placed between the digits, avoiding skin-skin contact.
method of care applies gauze dressing after the wound is prepared. Antibacterial cream, such as silver sulfadiazine (avoid if sulfa allergy, G6PD) or bacitracin/polymixin B, is applied to the thickness of a tongue blade then covered with gauze sponges loosely held by tape or some form of wrap. Alternatively, the antibacterial cream may be applied first to the gauze. For burns of the hands and feet, gauze may be placed between the digits, avoiding skin-skin contact.
Follow-up Care for Minor and Moderate Burns
After 24 hours, the provider should reinspect and further debride the burn as necessary. Thereafter, dressing changes should be once or twice daily; depending on the wound and the caregiver’s abilities, these may be done at home with less frequent office visits. The frequency of follow-up visits will depend upon the extent of the burn, the need for ongoing debridement, and the ability, reliability, and comfort level of the primary caregiver. All caregivers must be vigilant for signs of infection that would necessitate aggressive treatment to avoid further complications and scarring. The deeper the wound, the more likely superinfection will occur. Standard tetanus prophylaxis is necessary with all second- and third-degree burns. Empiric antibiotics should not be used.
Management of Major Burns
For major burns, the patient should be managed in an emergency department and, immediately after stabilization, be referred to a pediatric burn center. Acute management must focus on the following complications:
Direct smoke inhalation of particulate matter, toxins, and hot gases can cause airway inflammation and injury leading to compromise of upper and lower airways.
Carbon monoxide poisoning should be suspected in all cases associated with enclosed fires or evidence of smoke inhalation.
Dehydration and shock are possible from fluid losses through the burned skin.
Renal failure is possible from myoglobinuria and dehydration.
Risk of superinfection and sepsis is possible.
Providers must give special attention to minimizing heat loss (exposure, cold IV fluids, wet dressings), providing sterile dressings, and adequately treating pain. Suspected carbon monoxide poisoning should be treated with maximal supplemental O2, and any signs of respiratory distress may prompt early endotracheal intubation. Aggressive fluid resuscitation and monitoring are paramount.
Chemical Burns
Many household chemicals can cause burns. Acid burns tend to coagulate skin proteins, which in turn limit the depth, while alkali burns liquefy the skin and tend to penetrate deeper. Chemicals tend to cause burning for longer than thermal burns because the process continues until adequate neutralization or washing occurs, whereas thermal burns tend to be brief exposures or cool quickly. The burn may initially appear superficial despite deeper tissue destruction.
Treatment of chemical burns (both acid and alkali) involves copious irrigation. Providers must protect surrounding normal skin and sensitive structures such as the eyes and mucosal membranes as they wash away the chemical. They should avoid attempts at neutralization unless given specific instructions by a burn specialist. Providers can monitor the pH of the runoff to determine when to stop. Referral to an ophthalmologist for chemical burns of the eye is necessary after irrigation has begun.
Electrical Burns
Burns from electricity have some unusual characteristics. Most burns involve young children exposed to electrical appliances, damaged electrical cords, and electrical sockets. The thermal energy released depends on the tissue resistance, the voltage and type of current, and the duration of the exposure. For the scope of this text, only burns associated with low-voltage current will be discussed. Because electricity tends to find the path of least resistance, the current will typically follow blood vessels, nerves, and muscles, not skin. Therefore, “entrance wounds” may be less impressive, but clinicians must be suspicious for deep tissue injury.
Although burns may occur from arcing of electricity instead of current literally passing through the body, the provider should thoroughly inspect the patient for exit wounds. For small fingertip injuries from household current, no additional testing need be done. If the history suggests prolonged contact, initial alteration in consciousness, or proximal pain or swelling, the provider should treat the burn as a major burn. For significant electrical burns, the provider should perform cardiac monitoring and an ECG for evidence of dysrhythmias. Elevated creatinine kinase or myoglobinuria suggest evidence of underlying muscle injury. In such cases, patients are admitted for monitoring, IV hydration, and alkalization (the latter if at risk for renal failure). A specific electrical injury to the lips occurs when a toddler bites an electrical cord. Providers should refer these burns to a specialist to minimize scarring and contracture. Bleeding from the labial artery 5 to 14 days after the injury may result in significant blood loss.
Inflicted Burns
Overall, approximately 10% of burns are inflicted, most of which are scalds. When an individual forcibly submerges a child’s hands or feet into hot water, the burns tend to be deep with clear lines of demarcation and symmetric involvement of both extremities. Similarly, scald burns of the buttocks and posterior thighs can result from forcible submersion. Clinicians should carefully note the characteristics of the edges and splash marks to determine if the burn pattern fits the history. Small deep burns from cigarettes and distinctive patterns from heaters and irons should raise concern for abuse. The distinctive pattern of symmetrical depth (perfectly flat contact with a solid object) or multiple burns is not typical of accidents.
HEAD TRAUMA
Head trauma is the leading cause of morbidity in children older than age 1 year (Frankowski, 1985). Each year in the United States, 250,000 children younger than age 14 years are hospitalized and 25,000 die or are permanently disabled from head trauma (Kraus, 1990). Males suffer head injuries twice as often as females and have a fourfold increase in fatal head injury (Kraus, 1990; Frankowski, 1985). Interestingly, males have an increasing rate of head trauma from ages 5 to 25 years, whereas females have a steady decline throughout the first 15 years of life.
The mechanism of head injury differs by age (Kraus, 1990). In infants and toddlers, head injury results from falls from
furniture or from a caregiver’s arms. In preschoolers, falls are still the major source of head injury, although motor vehicle collisions account for 25% of cases. In school-age children, falls, sports, and motor vehicles (sustained as a passenger, pedestrian, or bicyclist) equally account for head injuries. In adolescents, sports and motor vehicle accidents cause equal numbers of head injuries.
furniture or from a caregiver’s arms. In preschoolers, falls are still the major source of head injury, although motor vehicle collisions account for 25% of cases. In school-age children, falls, sports, and motor vehicles (sustained as a passenger, pedestrian, or bicyclist) equally account for head injuries. In adolescents, sports and motor vehicle accidents cause equal numbers of head injuries.
Anatomy, Physiology, and Pathology
The galea aponeurotics and the scalp cover the cranium. The galea is adherent to the scalp but only loosely connected to the cranium except at the margins. Inside the cranium, the dura is a fibrous membrane attached to the skull. Under the dura is the arachnoid. Finally the pia covers the brain. The space between the arachnoid and pia contains the cerebrospinal fluid.
The following factors make head injury common in pediatrics:
Poor judgement related to play activities and lack of safety with bicycles and crossing streets
Unfortunate dependence on adult supervision for seatbelt and helmet use
Relatively large head in proportion to the body, which makes head trauma likely during any form of injury
Brain injury can be divided into primary and secondary. Primary injury occurs from direct trauma to the brain either as a penetrating injury or by acceleration/deceleration injuries (as might occur with blunt trauma). Penetrating injury tends to produce focal injury, while acceleration/deceleration tends to produce a more diffuse injury. Blunt trauma occurs much more frequently than penetrating injuries in children. Secondary brain injury occurs from hypoventilation, hypoperfusion, or hypoxia either after isolated head injury or injury to other organ systems. The brain that has primary injury is much more susceptible to secondary injury.
The following is a classification of the different types of head injury:
Subgaleal hematoma. This represents bleeding beneath the galea aponeurotics. Because of the loose connection to the skull, blood loss in this space can be dramatic. Seemingly minor injuries, such as a tug on the hair, can cause dramatic bleeding. Despite the potential for large bleeds, complications such as orbital extension are rare.
Caput succedaneum. Scalp edema due to local pressure or suction may occur during labor and delivery. It is easily differentiated from cephalohematoma because the swelling is diffuse and not limited by the sutures.
Cephalohematoma. This is hemorrhage into the periosteum of the skull and therefore demarcated by the sutures. This finding is common in newborns from birth trauma.
Skull fractures. Skull fractures may present as focal swelling of the scalp, as a depression or crepitus to palpation, or on radiologic imaging of the brain following trauma. Fractures can be described as linear, depressed, or compound (ie, having multiple fragments). Basilar skull fractures should be considered in patients with epistaxis, hemotympanum, CSF rhinorrhea or otorrhea, or hemorrhage into the periorbital area (raccoon sign), postauricular skin (Battle’s sign), mastoid air cells (as seen on CT scan), or nasopharynx.
Concussion. This is the most minor brain injury that has a clinical definition based on some alteration in brain functioning or mental status. Examples are loss of consciousness, amnesia, and sleepiness. The definition implies no gross structural injury to the brain. Patients do not need to have loss of consciousness at the time of the trauma, but often have retrograde amnesia for events recent to and antegrade amnesia for hours to days following the injury. Patients may appear alert or have somnolence for one to two days. Higher cognitive functions that require mental concentration may be the sole disability.
Contusion. Cerebral contusion is equivalent to a bruise of the brain and often results from blunt trauma. The contusion can be termed “coup” if immediately adjacent to the site of impact or “contracoup” if opposite the site of injury. CT scan is used to diagnose contusions. Patients with contusions may present with altered consciousness, persistent vomiting or headache (or irritability in an infant), or focal neurologic findings or seizures.
Subdural hematoma. As implied by the name, hemorrhage occurs between the dura and arachnoid membranes. Direct blunt trauma or shaking injuries result in tearing of the cortical veins. Skull fractures are found in a minority of cases. Often there is associated brain injury underlying the hemorrhage. Acute subdural hemorrhage can present as seizures or signs of increased intracranial pressure or simply as vomiting or headache.
Epidural hematoma. Bleeding occurs between the dura and the skull. Epidural hematomas are often associated with overlying skull fracture. Classically, the middle meningeal artery is lacerated, leading to a rapid deterioration of the patient after a “lucid interval” following the head injury. Epidural hematomas, however, also can be of venous origin, with a much more gradual deterioration, or present simply has headache, vomiting, or somnolence after a head injury.
Diffuse axonal injury. This refers to non-hemorrhagic brain injury with acute and diffuse brain swelling. These patients may present with coma or initially focal findings that progress to global neurologic deterioration over the following 18 to 48 hours, coinciding with peak intracranial pressure. Brain involvement often is extensive; therefore, prognosis generally is poor.
History and Physical Exam
Head injury can vary from simple laceration of the scalp to penetrating injury of the brain. The patient may present with any of the following findings alone or in combination: headache, dizziness, altered mental status (confused, somnolent, combative, irritable), or unconsciousness (coma or postictal state from seizure). Usually the presentation relates to the mechanism of injury; however, exact mechanisms are not always known. The head injury may appear to be isolated, but the mechanism of injury should dictate whether the provider needs to consider injuries to the cervical spine or other body areas. The patient with a minor head injury from a motor vehicle collision might have altered mental status from shock. Hopefully, patients with major mechanisms of injury will not present to the office or clinic setting. In such a circumstance, rapid triage to identify signs of significant injury should redirect the patient to an emergency department.
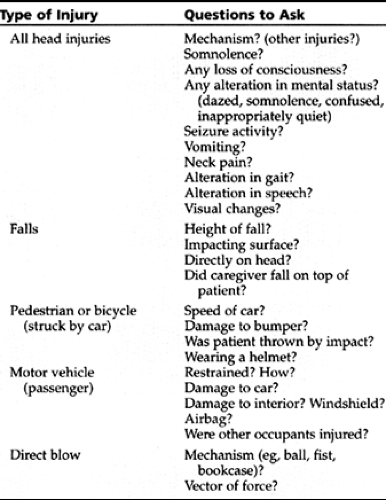
Important historical questions can provide an impression of the likelihood for brain injury (see Table 43-2). The provider should note the child’s behavior immediately antecedent to the accident: is it possible the child first had a seizure and then fell off the bike? When the mechanism is unclear or seemingly inappropriate for the injury, the clinician must consider child abuse. Specific features in the history may raise suspicion of abuse: unexplained injury, discrepancy
of the history between caregivers, mechanism of injury inconsistent with the injury or the developmental stage of the child, a delay in seeking medical care, or the presence of other injuries.
of the history between caregivers, mechanism of injury inconsistent with the injury or the developmental stage of the child, a delay in seeking medical care, or the presence of other injuries.
For patients who are unconscious or severely impaired, attention to airway, breathing, and circulation has priority. Patients who present with major alterations in consciousness after head injury require immediate transport to an emergency room after cervical spine immobilization. Medical personnel always must accompany the patient because of the potential for aspiration, airway obstruction in an unconscious state, and seizure. Providers always must consider other causes of altered mental status besides head injury (see Display 43-1).
DISPLAY 43–1 • Differential Diagnosis of Altered Mental Status
Central nervous system
Trauma
Intracranial bleed
Diffuse axonal injury
Concussion
Hydrocephalus
Seizure
Stroke
Tumor
Cardiovascular
Arrhythmia
Shock
Metabolic
Hyponatremia
Hypoglycemia
Diabetic Ketoacidosis
Hyperammonemia
Severe metabolic acidosis
Uremia
Toxin/ingestion
Gastrointestinal
Intestinal catastrophe
Intussuception
Liver failure
For the more common scenario of a seemingly minor head injury, key historical points include the time of the injury; the behavior of the child since the injury; the presence of vomiting, somnolence, irritability (in the young child), or head-ache (in the older child); and disturbance of vision, speech, or gait.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree