Migraines with Aura and Their Subforms
F. Michael Cutrer
Jes Olesen
DEFINITION OF MIGRAINE WITH AURA
IHS Code and Diagnosis
1.2 Migraine with aura
WHO ICD-10NA Code and Diagnosis
G43.1 Migraine with aura
Short Description (29)
Recurrent disorder manifesting in attacks of reversible focal neurological symptoms that usually develop gradually over 5 to 20 minutes and last for less than 60 minutes. Headache with the features of migraine without aura usually follows the aura symptoms. Less commonly, headache lacks migrainous features or is completely absent.
Other Terms (29)
Classic or classical migraine
Ophthalmic, hemipresthetic, hemiplegic, hemiparetic, or aphasic migraine
Complicated migraine
Migraine accompagnée
IHS Diagnostic Criteria for Migraine With Aura (29)
A. At least two attacks fulfilling criterion B
B. Migraine aura fulfilling criteria B and C for one of the subforms 1.21 to 1.26
C. Not attributed to another disorder. History and physical examination do not suggest any of the disorders listing in groups 5 to 12 of the IHCD-II classification, or history and/or physical and/or neurologic examinations do suggest that such disorder but it is ruled out by appropriate investigations, or such disorder is present but attacks do not occur for the first time in close temporal relation to the disorder.
The transient neurologic symptoms of migraine aura are at the same time fascinating and disturbing and are often the symptoms that motivate patients to consult a physician. For years, there has been ongoing debate as to whether migraine with and without aura represent two distinct pathophysiologic processes (5,55). However, there is increasing evidence from genetic studies of great heterogeneity within even small subtypes of migraine with aura (66). Underscoring this genetic heterogeneity is the fact migraine with aura has been linked to several distinct loci on different chromosomes (11q24 [12], 4q24 [67], 19p13 [36], and Xq24-28 [47]) and several genetic polymorphisms (37,39,41,52,54). Broad categories based on attack description, although very important in practice and in clinical research, may not always be reliable guides to the details of pathophysiology. In this context, the aura may be viewed a cortical phenomenon that may be one of the ways in which the trigeminocervical pain system is activated in susceptible individuals resulting in a migraine headache.
GENERAL CHARACTERISTICS OF THE MIGRAINE AURA
The aura consists of fully reversible visual, sensory, or language symptoms that precede or accompany the appearance of a migraine-like headache. Both the visual and sensory symptoms often have a bimodal progression with positive symptoms (shimmering lights, zigzagging line, or prickling paresthesias) followed by negative symptoms (blind spot or numbness). Also characteristic of the typical aura is a spreading or migratory quality in which the symptoms spread across the visual field, up an extremity, or across the face.
Because the aura is subjectively experienced, the most detailed and precise descriptions come from physicians or other professional who recount their own auras. This method can be criticized as being biased toward more complex or interesting symptomatology and less representative of aura as it is most commonly experienced.
Unfortunately retrospective chart reviews of symptomatology and to some extent questionnaire-based series, although more typical, are probably less accurate (Fig. 44-1). In 1996, Russell and Olesen published a nosographic analysis of migraine aura in 163 sufferers identified in a sampling of 4,000 Danish citizens (58). Because it was drawn from the general population, it was less likely to be affected by selection bias for more striking cases. In this series, 62 subjects had some migraine auras with headache and some attacks without headache, whereas 7 subjects experienced only auras without headache. In Russell’s study population, visual aura was overwhelmingly the most common aura symptom, occurring in 99% of cases, followed by sensory, aphasic, and motor auras. Visual aura occurred without any other aura symptoms in 64% of cases, whereas other aura types usually occurred in combination with another aura type (usually visual). These findings are similar to those seen in a small prospective study published 2 years earlier in which 54 migraine auras in 20 patients were described in detail (57). In this study, visual and sensory aura symptoms developed over 15 to 25 minutes and persisted for 20 to 55 minutes. When visual and sensory symptoms preceded a headache, the headache was typically migrainoid. However, if a headache preceded the aura symptoms, the headache was of the tension type.
Unfortunately retrospective chart reviews of symptomatology and to some extent questionnaire-based series, although more typical, are probably less accurate (Fig. 44-1). In 1996, Russell and Olesen published a nosographic analysis of migraine aura in 163 sufferers identified in a sampling of 4,000 Danish citizens (58). Because it was drawn from the general population, it was less likely to be affected by selection bias for more striking cases. In this series, 62 subjects had some migraine auras with headache and some attacks without headache, whereas 7 subjects experienced only auras without headache. In Russell’s study population, visual aura was overwhelmingly the most common aura symptom, occurring in 99% of cases, followed by sensory, aphasic, and motor auras. Visual aura occurred without any other aura symptoms in 64% of cases, whereas other aura types usually occurred in combination with another aura type (usually visual). These findings are similar to those seen in a small prospective study published 2 years earlier in which 54 migraine auras in 20 patients were described in detail (57). In this study, visual and sensory aura symptoms developed over 15 to 25 minutes and persisted for 20 to 55 minutes. When visual and sensory symptoms preceded a headache, the headache was typically migrainoid. However, if a headache preceded the aura symptoms, the headache was of the tension type.
In a recent study, Eriksen et al. (15) compared the characteristics of migraine with aura in patients with familial nonmotor migraine with aura to those seen in migraineurs with aura from Russell’s 1996 general population based study. Patients with familial migraine with aura had an earlier onset of attacks and a later age of cessation of attacks. They also had a higher co-occurrence of migraine without aura. In an outcome study of 53 patients initially seen for migraine with aura between 1977 and 1984, the long-term prognosis of for migraine with aura was good. At the time of a follow-up telephone interview, attacks had ceased for 2 years in 36% of patients (55% of males and 31% of females). Attacks had stopped in 41% of patients with visual aura without other aura symptoms and in 25% of those with sensory or aphasic aura besides their visual aura (P = .36). In those who continued to have migraine with attacks at follow-up, the frequency of attacks and headache intensity were improved in 44% and 41% of the patients, respectively. Because the symptomatology can be complex, diagnosis in the context of a primary care setting can be problematic. Recently, Eriksen and Olesen (17) developed and validated a simple diagnostic scale for migraine aura known as the Visual Aura Rating Scale (VARS). The scale is based on a quantification of the cardinal characteristics of the visual aura. The choice of the visual aura for quantification is based on the fact that a large majority of patient suffering from migraine aura experience visual symptoms (58). The VARS score consists of the weighted sum of the presence of five visual symptom characteristics. These include: duration 5 to 60 minutes (3 points), develops gradually (2 points), scotoma (2 points) zigzag lines (2 points), and unilaterality (1 point). A VARS score of 5 or more predicted the diagnosis of migraine with aura with a sensitivity of 96% and a specificity of 98% (17).
Visual Aura
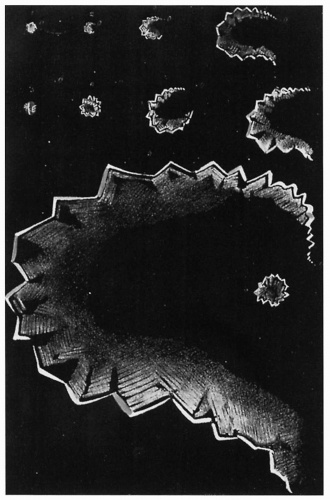
According to Schiller (60), the term fortifications was first used by Fothergill in his 1778 account of sick headache. He noted that during a migraine aura objects appear surrounded with luminous angles like those of fortifications. Over the next 100 years a number of British scientists described and accurately mapped their visual symptoms. Some of them experienced fortifications, others only hemianopsia. Hubert Airy (1) coined the term teichopsia (a translation of “seeing fortifications”) and published precise drawings of his own visual symptoms, which were not followed by headache (migraine aura without headache) (Fig. 44-2). Jolly (35) accurately recorded and drew 24 visual auras. In addition, he reported on his experience with several hundred visual auras over the years. His first symptom was usually a hazy spot close to the center of vision (Fig. 44-3). The spot was followed after 2 to 15 minutes by a star-shaped figure, which was shining and flickering, and then by a semicircular zigzag line (fortification). The fortification slowly moved away from the center of vision while expanding in size and finally disappeared at the extreme lateral margin of the visual field. Sometimes the
disturbance was more pronounced in the upper quadrant, sometimes in the lower quadrant, but it never crossed the midline. In 3 or 4 of about 100 instances, visual symptoms developed in the reverse order, that is, starting laterally in the visual field. Concerning the location of headache, Jolly observed a few attacks that were ipsilateral to the visual symptoms, but the vast majority of attacks were associated with contralateral or bilateral headache. In his later years, the visual auras were no longer followed by headache.
disturbance was more pronounced in the upper quadrant, sometimes in the lower quadrant, but it never crossed the midline. In 3 or 4 of about 100 instances, visual symptoms developed in the reverse order, that is, starting laterally in the visual field. Concerning the location of headache, Jolly observed a few attacks that were ipsilateral to the visual symptoms, but the vast majority of attacks were associated with contralateral or bilateral headache. In his later years, the visual auras were no longer followed by headache.
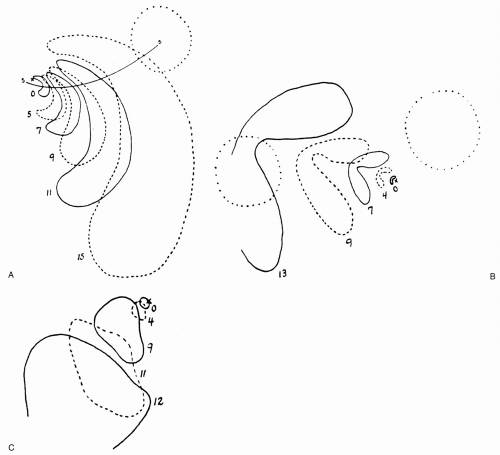
Lashley (40) suffered from visual auras without headache and mapped his auras very accurately. His profound knowledge of the visual system (he was a visual physiologist himself) enabled him to add considerably to existing descriptions of visual auras. There were a number of common features. The auras always started at or near the center of fixation and gradually spread laterally. They were almost symmetrical in both eyes and never impinged on the midline. Some of the scotomas were exclusively negative, whereas others scintillated at the edge, which appeared zigzag shaped (fortifications). In some instances only part of the scotoma scintillated above or below a certain point. As the scotoma moved laterally it increased in size and the rate of drift increased. In some auras the shape of the scotoma was very well preserved as it drifted, whereas the shape changed during other auras (Fig. 44-4). Usually the scotoma affected both the upper
and lower quadrant of the right or left hemifield of vision (see Fig. 4A and B), but occasionally only the lower or upper quadrant was affected (see Fig. 4C). The size and density of scotomas varied, and complete hemianopsia was observed in only one instance from more than 100. Close examination of the scintillations revealed series of parallel zigzag lines. There was a tendency for the pattern of figures in each part of the advancing front to remain relatively constant in both size and shape as the fortification drifted laterally. The period of inhibition after scintillations had passed varied (as indicated by the size of the scotoma) from approximately 5 minutes to approximately 30 minutes. Only a few auras were completely without scotoma, in contrast to the reports of Jolly (35), who usually had fortifications without scotoma (see Fig. 44-3). The rate of scintillations was estimated at 10 cycles/sec. A negative scotoma might completely escape observation. Hare (27) confirmed Lashley’s findings and added accurate measurements of the vertical diameter of the fortification figure. It was found to increase exponentially with time (Fig. 44-5).
The rate of shimmer of the fortification line diminished during the march. After 3 or 4 minutes, it was on the order of 10 to 15 cycles/sec, decreasing to about 3 or 4 cycles/sec toward the end. In contrast to the previous findings of Schumacher and Wolff (61), amyl nitrite had only minor and very short-lasting effects on the diameter of the fortification figure.
and lower quadrant of the right or left hemifield of vision (see Fig. 4A and B), but occasionally only the lower or upper quadrant was affected (see Fig. 4C). The size and density of scotomas varied, and complete hemianopsia was observed in only one instance from more than 100. Close examination of the scintillations revealed series of parallel zigzag lines. There was a tendency for the pattern of figures in each part of the advancing front to remain relatively constant in both size and shape as the fortification drifted laterally. The period of inhibition after scintillations had passed varied (as indicated by the size of the scotoma) from approximately 5 minutes to approximately 30 minutes. Only a few auras were completely without scotoma, in contrast to the reports of Jolly (35), who usually had fortifications without scotoma (see Fig. 44-3). The rate of scintillations was estimated at 10 cycles/sec. A negative scotoma might completely escape observation. Hare (27) confirmed Lashley’s findings and added accurate measurements of the vertical diameter of the fortification figure. It was found to increase exponentially with time (Fig. 44-5).
The rate of shimmer of the fortification line diminished during the march. After 3 or 4 minutes, it was on the order of 10 to 15 cycles/sec, decreasing to about 3 or 4 cycles/sec toward the end. In contrast to the previous findings of Schumacher and Wolff (61), amyl nitrite had only minor and very short-lasting effects on the diameter of the fortification figure.
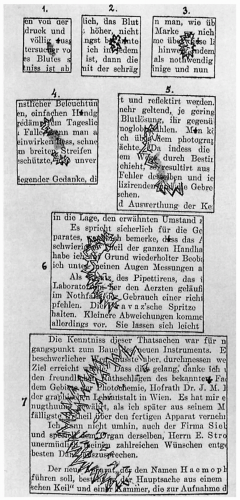 FIGURE 44-3. One of the visual auras experienced by Jolly. The typical features are obvious from the illustration. Little or no scotoma was associated with the fortification line. |
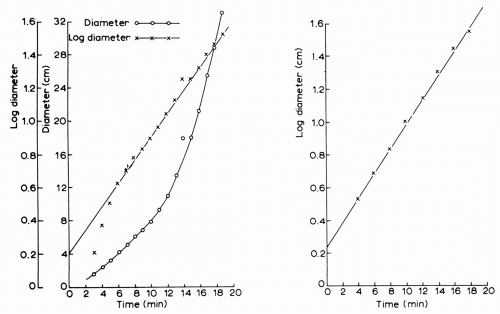 FIGURE 44-5. The vertical diameter of the fortification figure as measured by Hare (27). To the left, a logarithmic and a linear plot of this diameter at various times during a single aura. To the right, the mean of nine attacks plotted logarithmically. Note that the vertical diameter of the figure increases exponentially because it becomes a straight line in a logarithmic plot. |
In studies of larger numbers of patients, Alvarez (2) reported somewhat unsystematic observations in 618 migraine patients. The above pattern generally was confirmed. Most scintillations were uncolored, but sometimes colored lines appeared, usually behind the advancing scintillation. The scintillations varied in intensity from being almost blinding to being almost unnoticeable. The failure to observe negative scotomas was stressed by several patients, and Alvarez himself once noticed left-sided hemianopsia only when he failed to observe a car coming from the left. There was a preference for the hours between 11 AM and 1 PM in his own case, but this has not been described by others. He occasionally had two scotomas in a day, and in one instance a second scotoma started 10 minutes after another had disappeared. Such repetitive scotomas also had been observed by others (1,40), and occasionally more than one fortification figure has been seen at a time. Twelve percent of men, but only 0.7% of women, suffered from scotomas without headache according to Alvarez (2). Hachinski et al. (26) obtained drawings of visual symptoms from 100 children with migraine. Diffuse blurring, scotomas, distortions, and hallucinations were described, but the drawings were made retrospectively.
Bücking and Baumgartner (11) analyzed the symptomatology of auras in 87 migraine patients with aura, but it is not clear if it was by history alone or by prospective observation, probably the former. Only three did not have visual symptoms in addition to sensory, speech, or motor symptoms. The following numbers are therefore based on 84 patients. Six different types of visual disturbances were described (Table 44-1). They were mostly uncolored, but in eight cases spectral colors were reported, usually close to a fortification line. Only the fortification lines were clearly lateralized to one visual field, whereas other disturbances affected both sides. The different visual disturbances occurred in a typical order. Initially, unclear vision often changed into diffuse flickering spots that, again, progressed to grouped dysopsias and finally into a scintillating fortification line with scotoma. In 40 patients a gradual development of visual disturbances could clearly be described. Symptoms were reported to vary from attack to attack in the individual patient, but no quantitative data were given to support this observation.
In the 161 cases of visual aura studied by Russell and Olesen (58), 108 patients (69%) reported that symptoms were limited to one hemifield of vision, whereas 49 (31%) reported that symptoms were bilateral. Most commonly, the visual disturbance consisted of an uncolored, flickering zigzag-shaped line that usually appeared near the center of
vision (62%) and moved toward the periphery. A scotoma was left in the wake of the expanding visual disturbance about 50% of the time. The progression of the visual symptoms most often lasted less than 30 minutes (82%), and the total duration of the aura was under an hour in 111 patients (69%). When more than one symptom type occurred, the mean duration of the aura was increased (58).
vision (62%) and moved toward the periphery. A scotoma was left in the wake of the expanding visual disturbance about 50% of the time. The progression of the visual symptoms most often lasted less than 30 minutes (82%), and the total duration of the aura was under an hour in 111 patients (69%). When more than one symptom type occurred, the mean duration of the aura was increased (58).
TABLE 44-1 Localization of Components of the Visual Aura in 84 Patients with Classic or Hemiplegic Migraine | ||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||
Sensory Aura
Sensory migrainous symptoms are second in frequency to visual symptoms. The following frequencies have been given in patients with migraine with aura: 40% (34), 31% (58), 30% (45), and 41% (11). Of 36 patients in the study by Bücking and Baumgartner, 23 reported unilateral occurrence, usually in the upper extremity and periorally. This so-called cheiro-oral (hand-mouth) distribution was also noted in most of the patients of Manzoni et al. (45). Specifically, the spread of paresthesias to involve the tongue is very typical and rarely seen in cases of cerebrovascular ischemia (21). In 10 cases, a slow spread was noted, usually starting in the thumb and gradually spreading to the whole hand and to the perioral region. In six cases the leg was affected. Paresthesias affected only the hand, the face, or the foot in the rest of the patients. The affected side changed from attack to attack. Quite often paresthesias were the first sensory symptom leaving numbness in their wake. Heyck (31) noted a cheiro-oral distribution of sensory symptoms in 20 of 40 patients with sensory symptoms, and gradual spread of symptoms in 6 of 7 patients where sufficiently reliable information was available. Russell found that among 51 patients with sensory aura, the hand (96% of cases) and face (67%) were the body parts most often affected, whereas the leg (24%) and trunk (18%) were much less commonly involved. In Russell’s series, sensory symptoms tended to progress less than 30 minutes (82%), and the total duration was usually less than 1 hour (80%). When occurring with motor aura, the symptoms tended to last longer. The Australian neurologist Lord (44) was able to describe his sensory symptoms very accurately:
In attacks commencing with tingling of the hands or face, orderly march was the rule, and attack details were predictable using the sensory homunculus. In some right hemisphere attacks, a gradual progression occurred, beginning with a disturbance of hand sensation with tingling, then numbness followed by loss of awareness of position of the arm, and then visual disturbance with teichopsia moving from the periphery centrally, also conforming to known neuroanatomical boundaries. Typically, a band of tingling marched along a limb or face with the region remaining numb for many minutes thereafter.
In a group of patients selected because they had aura symptoms in the extremities, the duration of limb symptoms varied markedly (10) (Table 44-2). There are no published self-observations with accurate timing or plotting of sensory disturbances similar to those available for the visual aura. The findings of one of the cases studied by Russell and Olesen (58) are shown in Figure 44-6.
Language Aura
Language or aphasic aura follows sensory and visual symptoms in frequency of occurrence (48). Speech disturbances in patients with aura have been observed at the rates: 22% (11), 20% (34), 18% (58), 17% (45), and 9% (4). In patients with hemiplegic migraine, it was found in 47% (10). In the latter study the disturbance was characterized as aphasia in 44 and as dysarthria in 3 patients. Bücking and Baumgartner (11), on the other hand, felt that it was difficult to decide in many cases whether dysarthria or aphasia was present. In most but not all patients, speech difficulty has been associated with other evidence, indicating involvement of the dominant hemisphere. Heyck (31) described 25 patients with speech disturbance (Table 44-3). It is interesting that five right-handed patients were aphasic and yet had a left hemiparesis. The author observed several similar cases. Not infrequently, patients report that speech disturbance occurs as the spreading paresthesias reach the face or the tongue. Russell and Olesen found that the duration of language aura symptoms was usually under 30 minutes (59%). Paraphasic errors (76%) and other types of impaired language production (72%) were common, and impaired comprehension also occurred (38%).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree