21
Middle years
Chest pain
The first major concern for many in this age group is chest pain as it is a major factor affecting the health of those in the middle year’s group. With ischaemic heart disease developing during this age period, many are concerned that they will suffer angina or, worse, myocardial infarctions. Despite health education campaigns cardiac disease remains one of the biggest causes of debilitation in the UK and is the most common cause of premature death in people aged under 75 years in the UK. The British Heart Foundation estimates there are around 146 000 myocardial infarctions and 96 000 new cases of angina each year, and 2.5 million people in the UK have coronary heart disease (Allender et al. 2008, Garner 2012).
The overall cost of caring for angina has been calculated by Stewart et al. (2003) to be around 1 % of the NHS budget, mainly because of hospital bed occupancy and revascularization procedures; however, the burden of chest pain is far greater than the burden of angina. Nilsson et al. (2003) report that 1.5 % of primary care consultations are for chest pain, but only 17 % of these are associated with definite or possible angina. Despite this anyone who suffers a sudden onset of chest pain must be encouraged to seek immediate treatment (National Clinical Guideline Centre 2010). Time is heart muscle and to leave ischemic chest pain untreated for any period can result in catastrophic illness.
The patient presenting to the Emergency Department (ED) complaining of chest pain requires careful assessment to determine the symptoms and subtle features that differentiate chest pain which is cardiac in origin from that which is non-cardiac (Box 21.1). Chest pain can be very frightening for the patient, especially if it is the first episode, and staff need to assess and determine the likely signs of such pain (Gerber 2010). A number of key characteristics may help the assessing nurse to distinguish cardiac pain from that of other causes:
• location: the location of the pain can give a big clue to the nature of the cause. Cardiac pain is centrally located and chest pain that is peripheral to the sternum is rarely cardiac in nature
• radiation: cardiac pain brought on by ischaemia can often radiate to the jaw, neck and arms. Pain situated over the left anterior chest and radiating laterally may have various causes, such as pleurisy, chest wall injury and anxiety
• provocation: angina pain is precipitated by exertion, rather than occurring after it. It disappears a few minutes after the cessation of activity when blood flow can again match the oxygen requirements of the muscle. In contrast, pain associated with a specific movement, such as bending, stretching or turning, is likely to be musculoskeletal in origin
• character of the pain: ischaemic pain is often described as ‘dull’ or like a heavy object sitting on the chest. Chest pain caused by gastric problems can be described as a bloating or full feeling. Conversely pleural pain may be described as ‘sharp’ or ‘catching’ (Box 21.2)
• pattern of onset: the pain of aortic dissection, massive pulmonary embolism or pneumothorax is usually very sudden in onset (within seconds). Myocardial infarction may build up over several minutes or longer, whereas angina builds in proportion to the intensity of the exertion. Pain which develops over a longer period, such as days or even weeks, is often associated with respiratory illness or muscular damage
• associated features: the severe pain of a myocardial infarct, massive pulmonary embolus or aortic dissection is often accompanied by autonomic disturbance, including sweating, nausea and vomiting. If the patient is flushed, it may reflect a pyrexia or it may be stress-related. Pallor may be indicative of inadequate cardiac function or shock. Breathlessness is associated with raised pulmonary capillary pressure or pulmonary oedema in myocardial infarction and may accompany any of the respiratory causes of chest pain. Associated gastrointestinal symptoms may provide the clue to non-cardiac chest pain, such as heartburn, peptic ulceration, diarrhoea and vomiting.
On assessment, it is essential to perform a full set of observations. Temperature, if high, can indicate infection, the rate and depth of the pulse can indicate cardiac damage or arrhythmia, respiration rate can indicate respiratory distress and blood pressure can show cardiac instability. This in conjunction with an ECG can give the assessor a clearer picture as to the nature and cause of the chest pain.
The classic pain of angina pectoris is diffuse and retrosternal and will often diminish after rest. In the case of myocardial infarct, it is localized in the centre of the chest, is usually severe in nature, radiating to the left arm and jaw, and is not relieved by rest. Myocardial infarction and its management will be addressed in Chapter 27.
It is vitally important to take a calm, careful history from the patient who presents complaining of chest pain. While diagnosing angina is not as vital as that of a myocardial infarction, it is crucial to know if the patient is developing it as if not a cardiac event it is an indication that the patient is developing coronary heart disease (Harvey 2004).
The patient should firstly be asked to describe the pain – its intensity, location, duration, what brought it on and whether there is any relevant history (Jerlock et al. 2007). Assessing whether the patient can talk in sentences or whether there is pain on movement can indicate whether the chest pain is respiratory or musculoskeletal in origin. Note also that the fear and anxiety brought on by chest pain can exacerbate symptoms in the patient.
Recording of temperature, pulse and blood pressure and a 12-lead ECG can offer an indication of the likelihood of cardiac-related chest pain. A raised temperature may be a result of the breakdown of cardiac enzymes in response to a myocardial infarct that has happened within the previous few hours or may be a result of underlying infection. Recording of pulse oximetry, which measures arterial oxyhaemoglobin saturation (SpO2), gives important information about the supply of oxygen to the tissues. However, Nicholson (2004) suggests there is no definitive evidence that oxygen has any effect on cardiac ischaemia. Patients whose oxygen saturation levels are under 95 % on air are regarded as hypoxic and should be given high-flow oxygen via a mask (Table 21.1). Supplementary oxygen intake to increase oxygen saturation levels helps to relieve tachycardia induced by hypoxia, thereby reducing cardiac workload.
Table 21.1
Oxygen masks, flow rates and approximate concentrations of delivered oxygen
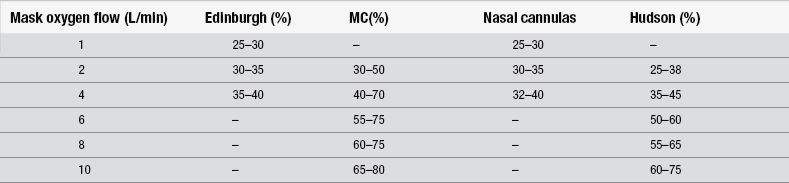
(After Jowett NI, Thompson D (1995) Comprehensive Coronary Care, 2nd edn. London: Scutari.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







