Links: Intro & Definitions | Risks | S/s | Angina | Women | Exam | Risk Stratification | Dx AMI | Serum Markers | Tx of AMI | Complications | Lead Changes | Q-waves | Ddx | Nitro Drip | Thrombolytics | Hemodynamic Changes | UAP / NQMI / NSTEMI / Acute Coronary Syndrome | GP IIb / IIIa Blocker | Chronic Angina | Variant Angina | Syndrome-X | Post-AMI | CAD | Post-AMI Tx, F/u & Testing | TOC |
The term MI describes the death of heart cells caused by an interruption in the flow of blood to those cells. The universal definition states that the term MI should be used when there is evidence of myocardial necrosis in a clinical setting consistent with myocardial ischemia.
Acute Coronary Syndrome (ACS): often defined as any group of clinical sx’s compatible with acute myocardial ischemia. The covers non–ST-segment-elevation MI (NSTEMI), unstable angina or STEMI (Mayo Clin Proc 2009;84:917-38). Some authors even include those with >70% stenosis on coronary angiography or positive noninvasive cardiac stress test but these may be just CAD if stable sx’s.
Unstable Angina: 1 or more of 3 presentations: Rest angina (usually lasting >20 min). New onset (<2 mo’s previously) severe angina. Crescendo pattern of occurrence (increasing intensity, duration, frequency or any combination). Algorithm involves starting ASA (use Clopidogrel if ASA intolerant) and then selecting a management strategy of either going to direct invasive testing or conservative (anticoagulate, ck LVEF and stress testing. If high risk proceed with angiography. If low risks & EF >40% cont ASA indefinitely and Clopidogrel for at least 1 mo) (Mayo Clin Proc 2009;84:917-38).
ST-segment-elevation myocardial infarction (STEMI) = Acute ST elev >1mm (coved over) in 2 or more contiguous leads. ST segment elevation events usually involves development of a Q wave. Infarct size is usually larger. Initial prognosis is worse. See NSTEMI | Silent MI |
Info: 15% of ECG completely normal. Infarction is usually due to fibrin rich thrombus occluding the vessel. Only 30% of all admitted to monitored beds rule in, yet some pt’s with left main stenosis have a normal ECG. Average delay for pt to get to ED after onset CP is 3hr. 50% of infarcts occur in people w/o prior CP or with <50% stenosis lesions. Medicare hospitalizations for AMI declined by 23% from 2002 to 2007 (Circulation 2010;121:1280)…..suggests that improvements in prevention and treatment really are translating into lower rates of AMI.
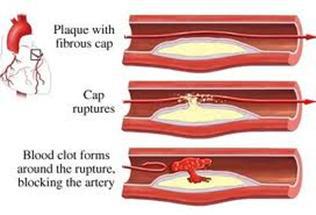
PP: Most acute coronary events involve plaque rupture. With plaque rupture, thrombogenic substances are exposed to platelets. Platelet response involves adhesion, activation, and aggregation. Platelet adhesion molecules are strongly thrombogenic and bind to von Willebrand’s factor (VWF). Thrombin, collagen, shearing forces, adenosine diphosphate (ADP), thromboxane A2, and serotonin are potent platelet activators. Platelet glycoprotein IIB/IIIA receptors cross-link fibrinogen or VWF as the common pathway of aggregation. The severity of ACS depends upon the extent of O2 deprivation by thrombus, with complete occlusion resulting in cell death. AMI results in injury to both the conduction system, leading to ectopy and dysrhythmia, and left ventricle pump function, leading to increased filling pressures.
• The incidence of MI is higher in winter mo’s, as is mortality (21.7% vs 20.1%) (peaks in December, not the result of decreased use of evidenced-based therapies) (Ann Intern Med 2005;143:481-485).
• The morphology and associated clinical presentation of ruptured coronary plaques differs between men and women (Am J Cardiol 2007;100:185-189)….the ruptures seen in women are more often linked to thrombus and have more acute presentation than those in men. A study found that most STEMIs and non-STEMI/UAP occurred at the site of severe coronary stenosis (diameter stenosis severity was <50% in a only 10% of cases (Am J Card 2009;103:1183-1188).
International Cardiology Societies Collaborate on MI Definition:
(Circulation 2012 Aug 24;e-pub ahead of print)
The preferred biomarker overall and for each specific category of MI is cardiac troponin (cTn) (I or T), which has high myocardial tissue specificity as well as high clinical sensitivity. An increased cTn concentration is defined as a value exceeding the 99th percentile of a normal reference population (upper reference limit, URL).
Myocardial infarction is determined by the specified cTn value, and at least one of the five following diagnostic criteria:
1. Symptoms of ischemia
2. New (or presumably new) significant ST-T wave changes or left bundle branch block
3. Development of pathological Q waves on electrocardiogram (ECG)
4. Imaging evidence of new loss of viable myocardium or regional wall-motion abnormality
5. Identification of intracoronary thrombus by angiography or autopsy
• The diagnosis of myocardial infarction should be made when the clinical setting suggests ischemia and testing reveals a rising and/or falling pattern of biomarkers with at least one value above the 99th percentile of the upper reference limit. This value is different for each assay, so clinicians need to know which assays are in use at the sites in which they are practicing. Defining a changing pattern is also assay-dependent and can be challenging; it can easily be accomplished, however, with the help of laboratory professionals who can calculate the difference necessary to establish that a change is not a variation in the measure itself.
• In some populations — such as the elderly, individuals with diabetes, and those who have just undergone surgery — presentation of MI can be atypical, so clinical judgment is necessary.
Several types of MI are defined:
• In type 1, or spontaneous MI, plaque rupture is the presumed etiology of the MI.
• Type 2 MI events are caused by supply–demand imbalance, which can be associated with all of the above clinical findings and can be present with or without coronary artery disease.
• Type 3 MI is when death occurs before biomarker values can be obtained or before a rising pattern can be established.
• Type 4a MI occurs after percutaneous coronary intervention (PCI) and requires a normal baseline biomarker value (<99th percentile URL) or a documented stable or declining set of values prior to the PCI. If the baseline value is normal, the diagnosis requires a 5-fold elevation in biomarkers, along with either symptoms or angiographic complications. If baseline values are stable or declining, a >20% increase (as with reinfarction) is required, again with the requisite signs and/or symptoms.
• Type 4b MI refers to infarction with stent restenosis and uses the criteria for types 1 and 2.
• Type 5 MI occurs after coronary artery bypass grafting and requires a 10-fold increase in biomarkers and ECG or imaging evidence of an event.
Key Risk Factors: M>45, F>55, current smoking, HTN, DM, HDL<35, FHx premature CAD (AMI/sudden death 1st Male relative <55 or 1st Female relative <65yo). CAD | Major Risks of CAD | Minor Risks | Cold weather snaps can trigger MIs (2-fold risk if mean temp < -4 C = 24.8F), particularly in people with high blood pressure (European Society of Cardiology Congress 2004), there was also a 62% greater risk of MI when the temp difference between the day before and the day of the attack was >5 degrees C.
• The risk of acute MI (plaque rupture) appears to be higher between the hours of 6 a.m. and 12 noon (circadian rhythm of arterial pressure surge accompanied by an increase in heart rate and vascular tone, and decreased serum cortisol levels) than in any remaining six-hour period of the day (Am J Cardiol 2004;93:1-5).
• Acute infection can apparently trigger a cardiovascular event in susceptible individuals (NEJM 2004;351:2611-2618), the risk does not appear to be affected by influenza, tetanus or pneumococcal vaccinations.
• Working while ill significantly increases the risk of AMI in men (Am J Public Health 2005;95).
• Users of tricyclic antidepressants or SSRIs appear to be briefly at a heightened risk of having a first acute myocardial infarction (Heart 2005;91:465-471) (odds ratio for MI in 1st week was 1.90 & 2.59), this may be due to depression-related effects rather than to the agents themselves.
• The incidence of acute MI, but not stroke, is increased in the 24 hours after a rapid fall in barometric pressure (Am J Cardiol 2005;96:45-51).
• Acute coronary syndromes may be precipitated by subclinical UTI, perhaps through inflammatory disruption of atherosclerotic plaque according to a case-control study (Am Heart J 2005;149:1062-1065).
• Physical exertion and anger may trigger the onset of chest pain and other sx’s in pt’s with acute coronary syndrome according to an observational trial with 295 men and women (Heart 2006;92:1035-1040).
S/s: Links: See below for ECG Evolution & QTc changes | Key Exam Findings | Serum Markers | Women | Silent MI |
Classic Presentation of AMI is unremitting CP (atypical Vs silent) –> pressing, squeezing, aching, burning. Pain radiating to L or R arm, R shoulder, or jaw, with CP being the most important sx.
Autonomic sx’s –> N/V/diaphoresis/ SOB/ weak/ dizzy/ palpitations/ anxiety/ sense of impending doom, rise & fall in serum enzymes. ~2/3 of pt’s describe the new onset of angina or a change in their anginal pattern in the month preceding infarction.
Other concerns: clutching chest, ashen appearance, abnormalities in the vital signs.
No Chest Pain at Presentation: 1/3 of pt’s. Seen in older (74 vs. 67yo), females, diabetics, prior heart failure. These pt’s have a worse prognosis as more likely to have stroke, arrest or pulmonary edema. Any sx associated with exacerbation should be considered ischemia, even tooth pain. Many people have old MI’s (Q’s) on ECG’s w/o having had “sx’s”. One can always consider a “mini-EST” by having them run in place a few minutes to reproduce sx’s from a fixed lesion. More than one quarter of pt’s PTCA report no sx’s during induction of coronary occlusion, contrary to previous reports, diabetic pt’s are no more likely than nondiabetic subjects to perceive myocardial ischemia (Am J Cardiol 2003;91:965-968). ~80% of pt’s with acute MI have an initial ECG (Lead Changes) that shows evidence of infarction or ischemia not known to be old, and any pt who has such abnormalities has too high a risk to be safely discharged, regardless of the clinical history or physical examination.
ED personnel failed to identify important, high-risk features on the ECG’s of about one in eight pt’s presenting with an acute MI in a retrospective analysis based on the two-year experience, 1684 pt’s of five medical centers (Implications of the failure to identify high-risk electrocardiogram findings for the quality of care of pt’s with acute myocardial infarction. Results of the Emergency Department Quality in Myocardial Infarction (EDQMI) study. Circulation 2006;114:1565-1571).
Ischemia and QT: Prolonged QTc (>32 ms) is an early sign of transmural ischemia that precedes ST elevation (>1 mm in two contiguous leads) according to a study in 74 pt’s undergoing elective cardiac catheterization (J Am Coll Cardiol 2007;49:1299-305)(found prolongation in 100% of pt’s at an average total balloon occlusion time of 40 seconds)(the uncorrected QT interval prolongation averaged 16 ms and was only seen in 77%)…QTc prolongation was followed by T-wave changes at 24 seconds, ST elevations at 29 seconds, and ST depression at 35 seconds. However, only 7% of pt’s had T-wave changes, 15% had ST elevations, and 7% had ST depression….THUS a prolonged (previously normal) QTc interval in a pt with chest pain and without another explanation (e.g., medications) can reasonably be considered a harbinger of worsening ischemia and should prompt frequent repeated ECGs, at the very least.
Angina Pain: from epigastrium to jaw. Most often retrosternal, parasternal, or felt across the anterior chest. May radiate to jaw, shoulder, arm (usually left side) as heaviness or numbness. Associated with dyspnea, diaphoresis and nausea. Is the discomfort reproducible and predictable? Responds to NTG within 10min (so does diffuse esophageal spasms). Inability to describe the discomfort is the most common sx. The practice of supporting or excluding the dx of myocardial ischemia should not be based on a pt’s response to nitroglycerin.
Other Links: Angina Response to Nitro | Chronic Angina | Tx Angina | Women and chest pain | S/s AMI | Types of Angina & Functional CP | Silent MI |
Angina equivalents –> dyspnea, N/V, diaphoresis, acute weakness, syncope.
Unusual but possible pain characteristics –> burning/ indigestion-like, sharp/ knife-like chest pain, pleuritic, chest wall pain reproducible on palpation, positional, improves with NSAIDs or GI cocktail.
Fixed threshold –> elderly & diabetics with DOE = anginal equivalent.
Variable threshold –> depends on time of day, related to vasomotor tone.
Factors associated with inappropriate discharge of pt’s with chest pain from emergency departments: younger age, female sex, non-white ethnicity, atypical sx’s, no previous MI, and normal or near-normal ECGs. There is no absolutely fail-safe way to exclude myocardial ischemia or infarction at the time of a pt’s initial presentation.
Exam: Most useful in excluding other potentially serious causes of the pt’s chest pain. May have a dyskinetic apical impulse on palpation, a 4th heart sound and less commonly a 3rd heart sound. Often have normal to muffled heart sounds. Hypotension (SBP <80), pulmonary crackles, cannon A waves if AV dissociation. Response to SLN may be complete, partial or none, but any response is helpful.
New systolic murmur –> papillary m. dysfunction, rupture of papillary head, rupture of chordae tendinea, acquired VSD, TR from RV infarct/ pulmonary embolus or pseudoaneurysm.
RV infarct –> hypotension, incr JVD, clear lung fields, Kussmaul’s sign, inferior infarct.
Key Physical Findings: Sinus tachycardia is common (anxiety). Either hypotension caused by left or right ventricular dysfunction or arrhythmia or HTN caused by adrenergic discharge may be present. RR may be elevated because of anxiety or pain or because of hypoxia. The jugular venous pressure may be elevated, reflecting RV dysfunction (common with inferior infarction). Atrioventricular dissociation may produce so-called cannon A waves (abnormally high jugular venous waves caused by atrial systole occurring when the AV valves are closed). The lung examination is typically normal, rales (crackles) may indicate CHF resulting from LV dysfunction. Pt may have a dyskinetic apical pulsation on palpation; a 4th or occasionally a 3rd heart sound may be audible. Ischemic mitral regurgitation (papillary muscle dysfunction) may be present. If a LBBB is present, abnormal splitting of the 2nd heart sound may be heard. The exam is most useful in excluding other potentially serious causes of the chest discomfort (PE, aortic dissection, PTX, pericarditis, and cholecystitis) rather than in confirming a dx of AMI. Higher blood pressures when patients were first admitted to the hospital with acute chest pain were associated with a better long-term mortality in a Swedish study (JAMA 2010; 303:1167-1172)……a systolic pressure of 200 or above was better than one of 160 mm Hg…..the author believes his study shows that these high pressures are an appropriate reaction to high stress.
Goldman Chest Pain Protocol: Link: Killip Class Risks | Tx of AMI | Women and chest pain | Testing & Interventions |
High risk if (>7% risk of AMI) –> elevated ST or Q waves in >2 leads not known to be old (high risk, 80%). ST-segment depression or T-wave inversion (moderate risk, 20%). CP >48hr with ST-T changes or ischemia or stain not known to be old. H/o angina or MI with longest episode of pain >1hr or pain worse than usual or the same as prior MI.
Intermediate risk if (4%) –> History of CAD but no ECG changes (Evaluation of chest pain. Mayo Clin Proc 2010;85:284-99).
Low risk if (2%) –> No Hx of AMI or CAD, age <40, CP reproduced with palpation, “stabbing” CP, no ST-T changes, longest episode of pain <1hr. Several hours spent in a chest pain observation unit for pt’s with undifferentiated chest pain appear to reduce the rate of hospital admission (36.7% Vs 53.8%) and return visits to hospital emergency departments compared with standard care (BMJ 2004;328:254), pt’s are observed for several hours, measured for biochemical cardiac markers, and undergo ECG and provocative cardiac testing when necessary.
• Routine telemetry monitoring of low-risk cardiac pt’s (Goldman risk scores <8% with negative initial troponin I and CK-MB) does not appear to be warranted (Ann Emerg Med. 2004;43:71-6).
• Low-risk pt’s (based on medical history, ECG results and cardiac markers) with chest pain can safely wait several days for exercise treadmill testing according to a study with 7,178 pt’s (Ann Emerg Med 2006;47:427-35).
• Among patients who presented with a chief complaint of chest pain and had low-to-moderate risk for acute coronary syndrome, women were less likely than men to have significant coronary artery disease according to data on 970 hemodynamically stable adult patients (40% women; mean age, 60)(CJEM 2010;12:405)…..Women were significantly more likely than men to have low (<10%) pretest probability for ACS (85% vs. 76%) and were significantly less likely than men to have known coronary artery disease (21% vs. 34%), pain characteristics typical for ACS (37% vs. 46%), positive stress test results for cardiac ischemia (4% vs. 8%), and acute myocardial infarction within 30 days (5% vs. 8%)……The take-home message from this study is that although women who present with chest pain have a lower likelihood of coronary artery disease than their male counterparts, the incidence is still substantial and women should undergo the same evaluation as men do.
Rouan Decision Rule for AMI:
Clinical Characteristics: One point for each clinical characteristic. Age >60 yo. Diaphoresis. History of MI or angina. Male sex. Pain described as pressure. Pain radiating to arm, shoulder, neck, or jaw.
Score –> Risk of MI.
0 –> Up to 0.6%.
1 –> Up to 3.4%.
2 –> Up to 4.8%.
3 –> Up to 12%.
4 –> Up to 26% (Am J Cardiol 1989;64:1087-92). Other add that the likelihood of MI is higher if there is pain radiating to both arms, hypotension, an S3 gallop or diaphoresis. Reduced likelihood if pleuritic chest pain or palpation of tender area reproduces chest pain. If score <3, and outpatient clinic setting with normal ECG, ck troponins at 6-72 hours after onset of CP to determine whether hospitalization or outpatient evaluation with stress testing is warranted (routine treadmill of low prob, add perfusion or echo in intermediate and angiogram if high).
Chest Pain in Primary Care Vs ED Setting:
Diagnosis –> %.
Musculoskeletal condition –> 30-36% Vs 7%.
Gastrointestinal disease –> 10-19 Vs 3%.
Serious cardiovascular disease –> 13-16 Vs 54%.
Stable CAD –> 8-10 Vs 13%.
Unstable CAD –> 1.5 Vs 13%.
Psychosocial or psychiatric disease –> 8-17% Vs 9%.
Pulmonary disease –> 5 Vs 12%.
Nonspecific chest pain –> 16 Vs 15%. (Episodes of care for chest pain. J Fam Pract 1994;38:345-52).
4 Risk Groups for ACS and AMI: (JAMA 2005;294:2623-9)
Low risk: pain that is pleuritic, positional, or reproducible with palpation or that is described as stabbing.
Probable low risk: pain that is not related to exertion or that occurs in a small inframammary area of the chest wall.
Probable high risk: pain described as pressure that is similar to pain of prior AMI or worse than prior anginal pain, or pain accompanied by nausea, vomiting, or diaphoresis.
High risk: pain that radiates to one or both shoulders or arms or that is related to exertion.
Vancouver Chest Pain Rule:
Step #1:
A. Age < 40: Normal initial ECG* and no prior history of ischemic chest pain** –> Suitable for Early Discharge.
B. Age >40 and low risk chest pain characteristics***:
Step #2:
A.Initial CK-MB <3.0 µg/L –> Suitable for Early Discharge.
B.Initial CK-MB = 3.0 µg/L –> No change in ECG or rise in CK-MB or Troponin from 0-2 hours after arrival –> Suitable for Early Discharge.
* T-wave flattening is the only acceptable ST-T abnormality
** Prior ischemic chest pain is defined as a past known diagnosis of MI or angina, previously prescribed nitroglycerine or a clear history of effort-related angina.
*** Low risk chest pain characteristics defined as pain not radiating OR increased with deep breath OR increasing with palpation.
• The Vancouver Chest Pain Rule sensitivity was high, the rule missed 1.4% of patients with acute coronary syndrome events at 30 days according to a sample 593 consecutive patients >25yo (Acad Emerg Med 2012;19:837)…..Use of the rule would have categorized 49.2% of study patients as low risk and eligible for discharge. Four of those patients (1.4%) developed ACS within 30 days; none of them died. The rule had a sensitivity for ACS within 30 days of 95.1%, a specificity of 56.3%, and negative and positive predictive values of 98.6% and 25.9%, respectively. Two of the four patients missed by the rule would have been identified by adding troponin-T measurement to the algorithm. This isn’t perfect, but it comes pretty close. This external validation study shows that the rule remains highly sensitive when applied outside the institution where it was developed. Although the rule doesn’t integrate troponin measurement, this additional information may improve its performance.
Info: Certain chest pain sx’s that decrease the likelihood of ACS include “stabbing or sharp” “pleuritic”, “positional” and “reproducible by palpation”, whereas sx’s such as “chest pain radiating to one shoulder” or “both shoulders”, “associated with N/V diaphoresis or “precipitated by exertion” increase the likelihood (JAMA 2005;294:2623-29)….but none alone or in combination can safely identify pt’s that can be discharged without further evaluation. The authors reiterate that studies have clearly demonstrated that relief of chest pain after administration of nitroglycerin or a GI cocktail is not useful for predicting ACS and AMI.
• The presence of inducible ischemia without self-reported angina is associated with a greater than 2-fold increased rate of recurrent CHD events according to a study with 129 pt’s that found that 24% of patients with stable CHD had inducible ischemia, and more than 80% of these patients did not report angina (Arch Intern Med. 2008;168(13):1423-1428)…..During a mean follow-up of nearly 4 years, CHD death or nonfatal MI occurred in: 7% of those without inducible ischemia or angina; 10% of those with angina alone; 21% with ischemia alone; 23% with both ischemia and angina.
• Older age, female sex, black race, Latino ethnicity, and presence of diabetes are associated with delays in presentation of acute coronary syndrome according to analysis of 3522 patients (Arch Intern Med 2008;168:1049). Routine cardiac stress testing in young adults evaluated in the emergency department for acute coronary syndrome is of limited utility as false positive results are very common (Ann Emerg Med 2009;54:12-16)….of 220 low-risk patients, younger than 40 years of age evaluated, 6 patients (2.7%) had positive stress test results and 4 of these patients underwent subsequent angiography that showed no obstructive coronary disease.
• An ER study on 1107 adult patients who presented with chest pain during the 7-month study period, 804 were triaged to monitored beds, and 303 were triaged to the waiting room……ACS was diagnosed in 10.6% of patients overall — 11.7% in the monitored-bed group and 7.6% in the waiting-room group (Ann Emerg Med 2010;May 23;e-pub ahead of print)…..No cases of ACS were missed in either group. Adverse events (mostly tachyarrhythmia’s) occurred in 4.0% of patients in the monitored-bed group and in 0.7% in the waiting-room group (not a significant difference).
See Syndrome-X / Microvascular | 40% of deaths in women are due to CV dz. There are a number of risks and sx’s differences. Heart disease in women should be called ischemic heart disease because it is different from the coronary artery version most common in men (l Am Coll Card 2009;Oct 15)…..the change could help focus attention on the greater symptom burden, functional disability and adverse outcomes experienced by women. The frequency of ischemic episodes is highest from the end of the luteal phase to the beginning of the menstrual phase and is lowest in the follicular phase. This likely reflects the cyclic variation in estrogen levels affecting endothelial function (Ann Intern Med 2001;35:977).
• Women who smoke present at the hospital for a major heart attack nine years earlier — on average — than women who don’t smoke cigarettes (AHA 2007;November. Abstract 1528). Risk factor profiles of coronary angiography patients differ by gender (J Intern Med 2010;Jan 14)……women were less likely to have severe disease than men (22.3% versus 36.5%)…..However, the women had higher rates of Canadian Cardiovascular Society class IV angina (56.7% versus 47.8%)……Class IV angina was a stronger predictor of severe disease among women (odds ratio, 1.82) than men (odds ratio, 1.28)…..Among other factors independently associated with severe disease were being male (odds ratio, 2.43), having diabetes (odds ratio, 2.0) and age (odds ratio, 1.05). Women are more likely than men to have exclusively noncalcified coronary plaques and are less likely than men to have calcified or mixed-composition plaques, which may in part explain why women are at lower risk of cardiac events according to a multidetector CT angiography study with 416-patient (Am J Cardiol 2010; 105:453–458).
Women with Chest Pain: An analysis of 1,941 pt’s with acute coronary syndromes, men were more likely to present with CP, left arm pain and diaphoresis, whereas nausea is more common in women (Am J Card 2006;98:1177-1181). Women have a greater number of sx’s (~3.4 Vs 2.5 for men), as well as “vague chest pain”, often c/o of dyspnea, N/V, indigestion, dizziness, fainting or fatigue. The pain may come and go w/o any identifiable activity or stress. Women ultimately diagnosed with MI have sx’s that are incorrectly diagnosed or dismissed as anxiety more frequently than men who are diagnosed with MI
• At least 75% have at least one prodromal sx of either extreme fatigue (71%), severe sleep disturbance (48%) or shortness of breath (42%) for >1 month prior to AMI (Circ 2003;108:2619-23).
• Although chest pain was the most common presenting symptom for acute coronary syndrome, about 1 woman in 3 with ACS presents without chest pain or discomfort (Arch Intern Med 2007;167:2396)(atypical presentations such as dizziness, jaw pain, and nausea).
• Women are as likely as men to feel chest pain or other typical heart-attack symptoms according to an study on 305 patients (39.7% women, average age 64) undergoing a nonemergent PCI were asked a series of open-ended questions about their sensations and experience while the angioplasty balloon was creating an ECG-evident ischemia(Can J Cardiol 2009;25(suppl B):115b)…..patients may not say they are feeling chest pain if another pain is more dominant. So providers must ask questions that elicit a more complete description of the patient’s symptoms in order to make an accurate diagnosis, she explained.
High risk –> (80%) likelihood if >2 major risk factors or 1 major + 2 minor/intermediate.
Low Risk –> 20% chance of dz if no major, and no more than 2 minor or 1 intermediate.
Major (typical angina, postmenopausal and no HRT, DM, peripheral vascular dz).
Intermediate (HTN, smoking, lipid d/o).
Minor (>65yo, central obesity, sedentary, FHx of CAD, other CAD risks). (NEJM 1996;334:1311)
Women and CAD: Presents at later age (post-menopause @ ~52yo), typical angina is not always present (often with shoulder/ jaw pain or dyspepsia, nausea), DM is a stronger influence than in males. More likely to die after 1st AMI, more long-term disability. Women less likely to undergo angioplasty or CABG. Low HDL a stronger predictor of risk compared to men. Women have a higher incidence of nontransmural MI and clinically silent infarctions. Exercise stress echo is less sens & spec in women.
Major prodromal sx’s (month or more before experiencing): Prodromal Symptoms: Average = 5.71, +/- 4.36 sx’s. In order of frequency of occurrence: Unusual fatigue @ 70%. Sleep disturbance @ 48%. Shortness of breath @ 42%. Indigestion @ 39%. Anxiety @ 35%. Heart racing (27%). Weak/heavy arms (25%). Changes in thinking or remembering (24%). Vision changes (23%). Loss of appetite (22%). Hands/arms tingling (22%). Difficulty breathing @ PM (19%). Arm aching (19%). Cough (18%). Incr Frequency of H-A (13%). Centered high chest pain
(14%). Scapula pain (13%). General chest pain (13%). Left shoulder/arm pain (12%). Numbness both hands (11%). Left breast pain (9%). Incr Intensity of H-A (9%) (Circulation 2003;108(21);2619–2623).
Major acute sx’s during AMI: Average 7.3, +/- 4.8 sx’s. In order of frequency of occurrence: Shortness of breath @ 58%. Weakness @55%. Unusual fatigue @ 43%. Cold sweat @ 39%. Dizziness @ 39%. Nausea (36%). Weak/heavy arms (35%). Arm aching (32%). Hot or flushed (32%). Indigestion (31%). Centered high chest pain (31%). Racing heart (23%). Left arm/shoulder pain (22%). Scapula pain (21%). Arm/hand tingling (21%). General chest pain (20%). Loss of appetite (19%). Vomiting (19%). Neck/throat pain (16%). H/A (15%). Left breast pain (15%). Vision change (13%). Bilateral arm pain (12%). Cough (11%). Top of shoulder pain (10%). Jaw/teeth pain (10%). (National Institute of Nursing Research (NINR). Circulation 2003;108(21);2619–2623) Diabetic women have a poorer prognosis from CAD compared with men (9.6 Vs 7.4% 1yr mortality) (Diabetes Care 2003;26:3142-7).
• Exercise echo (stress echo) may be the most cost-effective method for the initial assessment of CAD in intermediate-risk women due to its higher sens & spec (Arch Int Med 2004;164:1610-20).
• Even with new, more objective criteria (cTnT >0.05 mcg/L), women are still less likely than men to have their heart condition accurately diagnosed as myocardial infarction (Heart 2005;92:237-238).
• AMI during pregnancy, labor and delivery occurs rarely, those with acute MI are more likely to be older (66% were older than age 30 and 7% were older than 40), multiparous, non-Hispanic white or African Americans and to have more maternal (HTN, DM) and neonatal morbidities (Obstet Gynecol 2005;105:480-484).
• In men MI increases the risk of death from heart disease more so than diabetes, but in women diabetes is a greater mortality threat (J Am Coll Cardiol 2005;45:1413-1418).
• Of pt’s presenting with chest pain who undergo cardiac catheterization, women are three times more likely to have angiographically normal coronary arteries than men, yet these same women are then nearly three times more likely to be hospitalized for acute coronary syndrome over the next year than men (ESC 2005 Congress: Abstracts 1642 and 1430, presented Sept. 5, 2005)…..angiographically normal females do not appear to be truly free of disease, whereas angiographically normal men are….authors suggest intravascular U/S in normal arteries.
• Lower income, not race, may explain why some women are more likely to die of heart disease than others (Importance of Socioeconomic Status as a Predictor of Cardiovascular Outcome in Women. American Heart Association Scientific Sessions 2005;Nov. Abstract 3746).
• Among pt’s with initial ST-depression, 22% of women and 54% of men developed acute MI (Int J Cardiol 2006;109:241-247), among women a previous history of acute MI and advanced age were independent predictors for the development of acute MI Vs the presence of ST-depression, Q-waves and elevation of any biochemical marker prior to hospital admission being the best predictors for men.
• Women tend to rate their cardiac disease as less severe than men do when controlling for other measures of cardiac disease severity (Am J Med 2005;118:1256-61).
• Among 184 heart attack sufferers, women were more likely than men to dial 911 (57% did, versus 28%) – but there’s a lot of room for improvement for men and women, alike (Am J Cardiol 2012;online October 9)…..Among 292 people with unstable angina, only 15% of women and 13% of men called 911. It’s not clear how everyone else got to medical attention – whether they hopped on the subway or hailed a cab, according to the authors.
Anxiety: Physicians tend to interpret chest pain or other CAD sx’s as psychogenic when the patient is an anxious woman as compared to a man (“Gender Bias in the Diagnosis, Treatment, and Interpretation of CHD Symptoms: Two Experimental Studies with Internists and Family Physicians” TCT 2008;Abstract 561)……87 general internists were asked to make a diagnosis based on vignettes that described a 47-year-old man and a 56-year-old woman, each of whom had many cardiovascular disease symptoms and risk factors……fewer women received a CAD diagnosis (18% versus 57%, P<0.001)……When stress was a confounder, women were also less likely to be referred to a cardiologist (35% versus 76%, P<0.001) and were less likely to be prescribed cardiovascular medications (9% versus 43%, P<0.001) than men with the same symptoms and same life stressors.
Resting ECG: Any abnormal ECG finding was an independent predictor of myocardial infarction, stroke, and coronary heart disease death in asymptomatic postmenopausal women according to WHI data (JAMA 2007;297:978-985) (55% risk for minor and 150% for major ECG abn)….The use of hormonal therapy did not significantly affect the overall cardiovascular disease risk assessment by the ECG. The researchers defined minor prevalent ECG abnormalities as first- and second-degree AV block, borderline prolonged ventricular excitation, prolonged ventricular repolarization, isolated minor Q and ST-T abnormalities, LVH without ST-T abnormalities, left atrial enlargement, frequent atrial or ventricular premature beats, and fascicular blocks. Criteria for major abnormalities included atrial fibrillation or atrial flutter, high-degree AV dissociation, LBBB, RBBB, indeterminate conduction delay, Q-wave MI, isolated ischemic abnormalities, LVH with ST-T abnormalities, and miscellaneous arrhythmias including supraventricular tachycardia, ventricular preexcitation and ventricular tachycardia.
PP: A byproduct of cholesterol metabolism (27-hydroxycholesterol = 27HC) may help explain why women’s risk of heart disease increases after menopause (Nature Med 2007; doi:10.1038/nm1641). 27HC competes for the same receptors as estrogen in the vascular system. When there’s too much 27HC compared to estrogen levels — after menopause, for instance — blood vessels no longer get the protective effect of estrogen and become stiffer and less able to repair themselves. 27HC is what is known as an oxysterol, a class of metabolites of cholesterol that are produced in peripheral tissues as a means to eliminate cholesterol itself. A SERMs like tamoxifen and raloxifene.
• Most MIs in women could be prevented by consuming a healthy diet, being physically active, not smoking, and maintaining a healthy weight (Arch Intern Med. 2007;167:2122-2127)….The 5% of the study population who ate healthily (vegetables, fruits, and legumes), drank alcohol in moderation, and maintained these three low-risk lifestyle behaviors (nonsmoking, waist/hip ratios less than the 75th percentile (<0.85), and being physically active) had a 92% decreased risk of MI compared with women without any low-risk diet and lifestyle factors.
• Oral contraceptives may raise arterial atherosclerosis 20% to 30% for every decade of use according to a random sample of 1,301 apparently healthy women ages 35 to 55 in Belgium who underwent ultrasound imaging of atherosclerosis of the bilateral carotid and femoral arteries (AHA meeting 2007; Abstract 3614).
• A study on 211 patients (37% women) concluded that peripheral arterial vasoconstrictive response to mental stress was more pronounced in men compared with women, which may suggest that men have higher susceptibility to mental stress–related adverse effects (Am J Card 2008;102:970-974). Additional studies are needed to determine the significance of this finding and it is thought that estrogen, a known vasodilator mediates this effect in part by stimulating the release of nitric oxide and prostacyclin from the vessel wall….additionally, some reports suggesting that women have better coping skills with situational stressors than men……This could potentially attenuate their physiologic adrenergic response to psychological stress and women typically have less age-matched atherosclerotic CAD compared with their male counterparts.
Pregnancy: Incidence of pregnancy-related MI has risen, but mortality rates have declined (J Am Coll Cardiol 2008;52:171)….Neither unfractionated heparin nor low-molecular-weight heparin crosses the placenta; however, discontinuation of either agent before delivery is preferred. Nifedipine and ²-blockers are safe during pregnancy, but angiotensin-converting–enzyme inhibitors, angiotensin-receptor blockers, statins, and warfarin should not be used, and the safety of aspirin during the first trimester is uncertain. Women who experience a miscarriage are at a greater risk for myocardial infarction (MI) later in life according to data on 2876 women (25%) had at least 1 miscarriage, 2053 (18%) had at least 1 abortion, and 209 (2%) had at least 1 stillbirth (Heart. Published online December 1, 2010)…..After adjusting for age, smoking, alcohol consumption, body mass index, waist-to-hip ratio, physical activity, education, number of pregnancies, hypertension, hyperlipidemia, and diabetes mellitus, the researchers found that each stillbirth was associated with a hazard ratio (HR) of 2.32 for MI (95% confidence interval [CI], 1.19 – 4.50)…..Three or more miscarriages were associated with an HR of 8.90 (95% CI, 3.18 – 24.90).
CV Outcomes Among Women with Nonobstructive CAD: An estimated half of all women who undergo coronary angiography do not have obstructive coronary artery disease. Women with symptoms and angiography findings of nonobstructed (or even normal) coronary arteries had worse outcomes than asymptomatic women according to data on 540 symptomatic women (Arch Intern Med 2009;169:843)….the 5-year annualized rate for cardiovascular events (MI, stroke, hospitalization for heart failure, or cardiovascular death) was higher among symptomatic women with nonobstructive CAD (16%) and symptomatic women with normal coronary arteries (8%) than among asymptomatic women (2.4%)…..The elevated rates were driven in part by a higher incidence of hospitalization for heart failure and stroke…….results highlight the need for aggressive management of cardiovascular risk factors in women with symptoms suggesting CAD, even when they have normal coronary arteries on angiography……The authors theorize that endothelial dysfunction is a mechanism that could explain these findings…..possibly should be considered for further testing for endothelial dysfunction.”
Dx AMI: Links: Serum Markers | Tx AMI | Silent MI | Hx & PE & ECG. Gold standard is based on cardiac enzymes and ECG. No assessment protocol or constellation of tests is totally accurate in diagnosing acute coronary syndrome, thus risk stratification is important (see above). Can dx AMI if have elevated enzymes (CK or troponin) with EITHER sx’s or ECG changes suggestive of ischemia (Arch Int Med 2002;162:1585). Pain that is pleuritic, sharp/ stabbing, positional or reproduced on palpation decreases the probability of an AMI. 80% of those with an AMI have >1mm ST segment elevation, 20% have ST segment depression or new TWI. If no ECG changes, there is still a 4% risk of AMI if pt has h/o CAD and a 2% risk in pt w/o a h/o CAD. 15% of those presenting to the ER with acute CP have an AMI and 30-35% have unstable angina (NEJM 2000;342:16). A six-step chest pain protocol may improve the accuracy and speed with which cardiac conditions are diagnosed and treated in the emergency room setting. The steps include: initial ECG, baseline CK-MB and troponin I, serial ECG monitoring to detect new or evolving ischemia/injury, tests to detect changes in CK-MB & troponin at 2 hours, physician judgment of whether ACS is present, and nuclear stress testing in selected pt’s (Ann Emerg Med 2002;40:575-597)
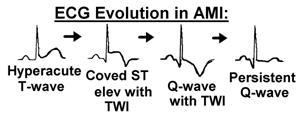
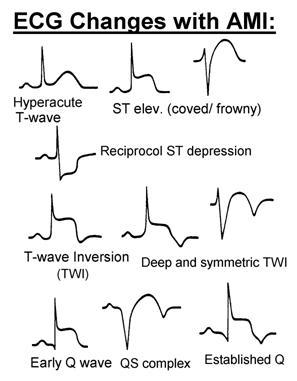
ECG Changes: (Lead Changes) ST elevation >1 mm in 2 contiguous leads (anterior V1-V4; inferior II, III, aVF; lateral I, aVL, V5, V6; true posterior R>S V1, V2). Followed by T wave inversion and ultimately Q waves. Or A new LBBB with compatible sx’s.
Notes: If severe, may get “tombstone” T-wave peak. ST elevation may be permanent if get a ventricular aneurysm. Look for reciprocal changes to identify acute.
Normal ECG During Chest Pain Does Not Rule Out ACS: Lack of changes on an ECG performed during chest pain often is thought to reduce the likelihood of ACS. Among chest pain patients with normal initial ECGs, a similar percentage had acute coronary syndrome whether the ECG was performed when chest pain was present or absent according to data on 387 patients who presented to an emergency department with chest pain, had normal initial ECGs, and were admitted for evaluation for A(Acad Emerg Med 2009;16:495)……..The prevalence of ACS did not differ significantly between the groups that did and did not have chest pain when the normal initial ECG was obtained (16% and 20%).
ECG compare Tip: Hold them up to light and view from the back, upside down a pw infarct will look like an ant wall. Avoid changes in lead placement, instruct the tech to either mark their position with ink or leave the leads in place.
Albumin Cobalt Binding Test: measures the amount of cobalt that binds to albumin in a blood sample. According to the FDA, structural changes in albumin can signal a severe illness such as heart attack. Structural changes in albumin can signal a severe illness such as heart attack, more cobalt is bound to the albumin, leaving less cobalt to be detected. The test involves adding a cobalt solution to a blood sample, with the results read on a chemistry analyzer. When used with an ECG and a troponin assay, helped rule out MI with a 70% accuracy rate (50% w/o). Costs $30 and takes 1-2 hrs.
High Risk Pt’s: include those with + troponins, ST-segment depression >0.5 mm, transient ST-segment elevation, or refractory pain with ECG changes despite medical tx (aspirin, heparin, beta-blockers), plus pt’s with acute CHF or hypotension. Consider early (<48hrs) cardiac catheterization for best results.
Any one of the these criteria would meet the diagnosis for MI: (Eur Heart J 2007;28:2525-2538)(Circulation. 2007;October 19: published online before print DOI: 10.1161/CIRCULATIONAHA.107.187397) “Expert consensus document” jointly sponsored by the American College of Cardiology (ACC), American Heart Association (AHA), European Society of Cardiology (ESC), and the World Heart Federation (WHF).
ACA/AHA 2012 Universal Definition for Myocardial Infarction:
• A cardiac troponin (I or T) level above the 99th percentile of a normal reference population, plus one or more of the following:
• symptoms of ischemia;
• new significant ST/T wave changes or left bundle branch block;
• pathologic Q waves on ECG;
• new loss of viable myocardium or regional wall motion abnormality, as observed on imaging;
• intracoronary thrombus diagnosed by angiography or autopsy.
Classification Description:
1. Spontaneous MI related to ischemia due to a primary coronary event, such as plaque erosion and/or rupture, fissuring, or dissection. Detection of rise and/or fall of cardiac biomarkers (preferably troponin) with at least one value above the 99th percentile of the upper reference limit together with evidence of myocardial ischemia with at least one of these — sx’s of ischemia, ECG changes indicative of new ischemia such as new ST-T changes or new LBBB; development of pathological Q waves in the ECG; or imaging evidence of new loss of viable myocardium, or new regional wall motion abnormality.
2. MI secondary to ischemia due to an imbalance of O2 supply and demand, as from coronary spasm or embolism, anemia, arrhythmias, hypertension, or hypotension
3. Sudden unexpected cardiac death, including cardiac arrest, often with sx’s suggesting ischemia with new ST-segment elevation; new left bundle branch block; or pathologic or angiographic evidence of fresh coronary thrombus — in the absence of reliable biomarker findings…death occurring before blood samples could be obtained, or at a time before the appearance of cardiac biomarkers in the blood.
4a. MI associated with PCI. Normal baseline troponins, elevations of cardiac biomarkers above the 99th percentile upper reference limit are indicative of peri-procedural myocardial necrosis. By convention, increases of biomarkers greater than 3 X 99th percentile upper reference limit have been designated as defining PCI-related MI.
4b. MI associated with documented in-stent thrombosis.
5. MI associated with CABG surgery. Normal baseline troponin values, elevations of cardiac biomarkers above the 99th percentile upper reference limit are indicative of peri-procedural myocardial necrosis. By convention, increases of biomarkers greater than 5 x 99th percentile upper reference limit plus either new pathological Q waves or new left bundle branch block, or angiographically documented new graft or native coronary occlusion, or imaging evidence of new loss of viable myocardium have been designated as defining CABG-related myocardial infarction.
Criteria could be used to identify a prior MI:
1. Development of new pathological Q wave with or without sx’s.
2. Imaging evidence of a region of loss of viable myocardium that is thinned and fails to contract, in the absence of a non-ischemic cause.
3. Pathological findings of a healed or healing myocardial infarction.
Info: Even in the absence of ECG changes, if you have a syndrome consistent with myocardial infarction or acute coronary syndrome, with a troponin elevation, then those two alone are sufficient to make the dx. Symptoms of ischemia: The discomfort of cardiac ischemia usually lasts at least 20 minutes and is diffuse as opposed to localized.
ECG changes indicative of ischemia in the absence of left-bundle branch block and left ventricular hypertrophy. The earliest ECG manifestations of myocardial ischemia are typical T-waves and ST segment changes. ST elevation is defined by elevation at the J-point in 2 contiguous leads with the cutoff points of at least 0.2 mV in men or at least 0.15 mV in women in leads V2-V3 and/or at least 0.1 mV in other leads. ST depression is defined by at least 0.05 mV in 2 contiguous leads. T-wave inversion is significant when is at least 0.1 mV in 2 contiguous leads with a prominent R wave or R/S ratio greater than 1. Development of pathologic Q waves on ECG. New left-bundle branch block.
“Triple Rule-Out” by Coronary CT Angiography: simultaneously rule out significant CAD, pulmonary embolism, and thoracic aortic dissection. A study on 200 patients who presented with chest pain that suggested acute coronary syndrome (ACS) were followed for 30 days found that that 65% of patients did not have CAD, 23% had mild disease (<50% luminal narrowing), and 11% had moderate-to-severe disease (Radiology 2008;248:438)…..At 30-day follow-up, 174 of 175 patients with no or only mild CAD had not developed acute coronary syndrome (negative predictive value, 99.4%); a single high-grade right coronary-artery lesion was present on CT but was missed by the reader. Three patients had pulmonary embolisms, and one had an aortic dissection……Clinically important noncoronary diagnoses that explained patients’ symptoms (found in 11% of patients) included pneumonia and congestive heart failure…….Clinically important diagnoses that did not explain patients’ symptoms (e.g., aortic aneurysm, emphysema, lymphadenopathy) were found in 14%.
• In a French study with 121 pt’s who underwent multidetector computed tomography (MDCT), pulmonary artery thrombosis occurred in 17% of acute chest syndrome (ACS) episodes (Am J Respir Crit Care Med 2011;184:1022)……75% involved segmental clots……all patients with positive MDCT scans also underwent Doppler ultrasound of the lower extremities, and none of these tests were positive……Magnetic resonance imaging was negative for fat in the clots……Traditional screening tests for venous thromboembolism, including D-dimer concentrations and Geneva score, were not predictive of thrombosis……Patients with positive scans did have higher platelet counts as well as lower levels of hemolysis markers (i.e., lactate dehydrogenase, total bilirubin) than other patients.
Physicians’ estimates of patient risk in ACS’s do guide their treatment decisions but are often inaccurate when compared with validated risk scores (Arch Intern Med 2009;169:372)….physicians paradoxically associated older age with lower risk, resulting in systematic underestimation of risk in older patients……suggest that informal risk estimates do not ensure optimal patient care and that physicians should follow practice guideline recommendations to use validated risk models in determining appropriate therapy for ACS.
Links: Below for Troponins | CK & Summary | Myoglobin & Other | See Major Risks | Minor Risk Factors | CRP | BNP |
Only 20% MI’s have +CKMB 3hr after sx onset, sensitivity best @ 4-8hr after sx onset: Need 25-50% rise between two values. Troponin-48%, MB-84%, reaches 90% at 8-12hr for Troponin and at 6hr for MB to r/o AMI. Rapid reagent card with Troponin I, MB, & Myoglobin has 99% specificity with 2nd set at 4hr, does not exclude unstable angina. The degree of elevation does appear to indicate the degree of risk for complications in acute MI. Cardiac troponin T levels predict short-term prognosis in pt’s with acute coronary syndromes regardless of their level of creatinine clearance (NEJM 2002;346:2047-2052).
Troponins: proteins found in cardiac and skeletal muscle tissue expressed by different genes. Cardiac troponins T and I are components of the contractile apparatus of cardiomyocytes and are the preferred biochemical markers of myocardial necrosis in patients with suspected acute coronary syndromes and among such patients, a strong association between elevated troponin levels and recurrent coronary ischemic events has been firmly established. It has been shown that even very small elevations in troponins are associated with an increased risk of an adverse outcome in patients with acute coronary syndromes (Am J Med 2003;115:178-184). They are located in the myofibrils at 400-A intervals along the actin filaments), where they regulate the interaction of actin monomers with the myosin heavy chain. There are of 3 kinds: troponin C (calcium binding), T (tropomyosin binding), and I (inhibitor of interaction). It is generally accepted that cTnI elevation in blood is a consequence of ischemic damage to cardiomyocytes (Am J Crit Care 2006; 15:280).
“Troponinosis”: false alterations (usually lower ranges) with non-AMI such as, unstable angina, pericarditis, myocarditis, CHF, Afib, pulmonary embolism or renal failure. May get cross reactive autoantibodies (assay interference with heterophile Ab, RF, excess fibrin or specialized fluids such as albumin or plasmin). Troponin elevation can be a secondary result of stroke in different brain areas, including the insular cortex (due to both reflex influences on sympathetic terminals in myocardium directly and catecholamine production outside it (Neurology 2006;66:1325-34).
Highly sensitive troponin I assays: The highly sensitive troponin I (hsTnI) assay (Architect STAT High Sensitivity Troponin; Abbott Diagnostics) and an established troponin I (eTnI) assay (Architect STAT). Use of either type of highly sensitive troponin I assay can safely exclude or confirm AMI within 3 hours of emergency department admission (JAMA 2011;306:2684)…..Of 1818 consecutive patients with suspected acute coronary syndrome who were enrolled at three hospitals in Germany during 2007 and 2008…..Using a diagnostic cutoff troponin concentration representing the 99th percentile of a reference population, hsTnI at admission had a sensitivity of 82% and a negative predictive value (NPV) of 95% for AMI, and eTnI had a sensitivity of 79% and an NPV of 94%….Sensitivity and NPV at 3 hours for both assays were 98% and 99%, respectively. Combining the measurement at admission with the relative change at 3 hours yielded positive predictive values of 96% for both assays.
One-hour rule-out and rule-in: using high-sensitivity troponins. An algorithm based on high-sensitivity cardiac troponin T accurately ruled out acute myocardial infarction in 60% of chest pain patients in 1 hour (Arch Intern Med 2012 Aug 13;e-pub ahead of print). Serum troponin was measured at presentation and at 1, 2, 3, and 6 hours using a high-sensitivity cardiac troponin-T (hs-cTnT) assay. Two independent cardiologists with access to all results adjudicated the final diagnosis. In the derivation set, no patient with a baseline hs-cTnT level below 12 ng/L and an absolute change of less than 3 ng/L in the first hour had AMI. For rule-in of AMI, the researchers determined that using either a baseline hs-cTnT level of 52 ng/L or higher or a change over 1 hour of 5 ng/L or more provided the greatest accuracy. When applied to the validation set, the algorithm had 100% sensitivity and 100% negative predictive value for AMI. The algorithm ruled out AMI in 60% of patients, and these patients had a 0.2% rate of all-cause mortality at 30 days. The algorithm ruled in AMI in 17% of patients, yielding 97% specificity and 84% positive predictive value. In 23% of patients, hs-cTnT values did not meet rule-in or rule-out criteria, and these patients were categorized as requiring additional evaluation.
Troponin T (cTnT): only in myocardium cells where 3-8% is freely dissolved in the cytoplasm and immediately released after cardiac cell injury. More cardiac specific than CPK, first rises in 3-4hr (as does CPK-MB), bedside assay takes 20 min., >0.2ng/ml high risk death/ reinfarction. Two neg troponin values 4hr apart or >6hr after onset of atypical CP –> likelihood of acute coronary event low. Reference range in serum: 0-0.1 mcg/L. A single measurement of plasma cTnT at 96 hours after sx onset (plateau) is strongly associated with myocardial infarct size (J Am Coll Cardiol 2006;48:2192-2194)….infarct sizes were larger in STEMI pt’s (median cTnT levels 1.88g/L) than in NSTEMI pt’s (0.83 g/L).
• Elevated concentrations of cardiac troponin I (cTnI) in patients with stable CAD are associated with an 88% higher risk of cardiovascular death or heart failure, as well as a 44% increased risk of nonfatal MI (J Am Coll Cardiol 2013; DOI: 10.1016/j.jacc.2012.12.026).
Limitations: incr levels may occur in severe muscle injury due to cross-reactivity with skeletal muscle troponin, but this should be less frequent with more specific (second generation) assays. Sensitivity: > 98%, specificity: 80%. Serial monitoring more useful than single determinations.
Noncardiac causes of incr Troponin T: cirrhosis, malignancy, hypothyroidism, sepsis (31-80% of pt’s elevated with no evidence of CAD, likely due to cytokine mediated inflammation of the myocyte), ultraendurance exercise (20% of marathon runners have increased cTnI levels at the end), rhabdomyolysis, Duchenne’s muscular dystrophy, polymyositis/ dermatomyositis. Incr levels can occur in some pt’s with renal failure (uremia, 4-17% have elevated cTnI). Pt’s with renal failure tend to have higher levels of all cardiac enzymes. Cardiac strain (strenuous exercise, CHF, PE, pulmonary HTN, COPD), direct myocardial damage (contusion, cardioversion, pericarditis, chemo, infiltrative d/o), ischemia due to hypotension, hypovolemia, LVH, SVT, AF, sepsis).
• Prolonged exercise, such as running in a marathon, is often associated with detectable levels of cardiac troponin T, even though there is no ECG evidence of cardiac ischemia (Heart. 2005;91:1219-1220).
• Troponin levels may increase significantly in marathon runners, even reaching levels diagnostic for acute myocardial infarction, according to results of a study involving participants in the 2002 Boston Marathon (Ann Emerg Med 2007;49:137-143)….68% of runners had some degree of post-race troponin level increase, ranging from 0.02 to 0.74 ng/mL for troponin T and 0.05 to 4.17 ng/mL for troponin I….subjects had never before participated in a marathon, and their risk of elevated serum troponin was 3-fold higher than for experienced runners. Age less than 30 years and female gender were also associated with elevated troponin levels.
• Troponin elevations in hospitalized pt’s are frequently not associated with an acute coronary syndrome–they can, in fact, occur within a broad range of other clinical presentations (PE, sepsis, stroke, trauma, internal bleeding, renal failure, or other conditions), and when they do, indicate a worse prognosis, according to an observational study (Arch Intern Med 2007;167:276-281).
• Diseased skeletal muscle can be a noncardiac source of increased circulating concentrations of cardiac troponin T (J Am Coll Cardiol 2011;58:1819).
• The absolute change in high sensitivity cardiac troponin (hs-cTn) levels between presentation and 1 hour can distinguish between acute myocardial infarction and nonischemic disease states (Circulation 2012;126:31). In a prospective, multisite, international study, researchers used assays from several manufacturers to measure hs-cTnT and hs-cTnI at presentation and at 1 hour in 887 patients with symptoms suggestive of acute myocardial infarction (AMI). Patients received usual care, including an electrocardiogram. Final diagnoses were adjudicated by two independent cardiologists who were blinded to hs-cTn results. None of the hospital laboratories used hs-cTn assays.
The adjudicated diagnosis was AMI in 15% of patients and noncoronary cardiac disease in 14%. Patients with AMI had significantly higher median levels of hs-cTnT (0.113 µg/L vs. 0.012 µg/L) and higher absolute changes in hs-cTnT in the first hour (0.019 µg/L vs. 0.001 µg/L) than those with noncoronary cardiac disease. Combining the hs-cTnT level at presentation with the absolute change in the first hour yielded a higher diagnostic accuracy than either value alone (area under the receiver-operating characteristics curve, 0.94 vs. 0.89). No patient with an absolute change <0.005 µg/L had AMI. Using ST-segment elevation, hs-cTnT level at presentation, and absolute change in hs-cTnT within 1 hour, the authors developed an algorithm to distinguish between AMI and cardiac noncoronary disease; in an independent validation cohort, the algorithm had a negative predictive value of 98%. Findings were similar with hs-cTnI.
Troponin I (cTnI): not an early marker, yet very specific for the heart and is superior when confounding influence are present such as skeletal muscle injury or renal d/o. Excellent for retrospective dx of AMI as lasts 1wk, especially if pt in clinic says they had crushing CP lasting 6h four days ago.
Normal = <0.07 ng/ml.
0.08-0.14 = usually not significant (critical) in outpatients.
0.15-0.4 needs additional cardiac eval.
>0.4 strongly suggests AMI.
ACC Guidance on Interpreting Elevated Troponin Levels:
(J Am Coll Cardiol. 2012;doi:10.1016/j.jacc.2012.08.969)
The ACC notes that an elevated troponin level does not necessarily indicate a myocardial infarction, but it is a reliable indicator of myocardial necrosis. The document also includes a proposed algorithm for using troponin in clinical decision making.
Among the recommendations:
• Troponin testing should be performed only if clinically indicated for suspected MI.
• For nonischemic clinical conditions, routine testing is not advised, except for cardiac prognosis in patients with chronic kidney disease and patients undergoing chemotherapy who have drug-induced cardiac injury.
• For patients with non-ST-segment elevation acute coronary syndrome, global risk assessment — rather than any single risk marker — should be used to guide therapeutic decisions.
Info: Mild transient elevation of troponin I with a cut-off value of 0.1 ng/mL is associated with an increase in all-cause mortality and cardiovascular complications in hospitalized pt’s (Arch Pathol Lab Med. 2005;129:474-480) (cardiac imaging can aid in further risk stratification of those cases). An analysis of observational data suggests that even small elevations in troponins in stabilized patients with ACS predicts mortality (Circulation 2007;116:1907)….A cTnI elevation >0.01 µg/L was observed in 48% of patients at 6 weeks. At 6 months, this percentage had fallen to 36%, including new elevations in 11% of patients…..In multivariate analysis, cTnI elevation >0.01µg/L 6 weeks or more after ACS was associated with an approximately twofold increase in mortality at 5 years (from 6% to 13%); the increase in mortality remained significant at a cTnI threshold >0.02 µg/L, but not at a threshold of >0.04 µg/L…..the authors propose more intensive secondary prevention measures for patients with persistent troponin elevation.
• A positive troponin test in bacteremic patients without acute coronary syndrome appears to be associated with poor prognosis (Am J Med 2008;121:909-915)……”it does not appear warranted to admit patients with sepsis to coronary care units.”
• Patients with minimal elevation of serum troponin (TnT >0.01 µg/L or TnI >0.01-0.07 µg/L) have smaller infarctions, less aggressive treatment, fewer early complications, and a better early prognosis (hospital mortality was 3.5% vs 6.7%) than patients with higher serum biomarker levels (Am J Med 2008;121:1065-1071)…..After discharge, however, their prognosis currently appears no different from that of patients with a “classic” myocardial infarction event.
• Even very low levels of cardiac troponin T are associated with increased risk for heart failure and cardiovascular death among patients with stable heart disease, according to a study on nearly 3700 adults with stable coronary artery disease and preserved left ventricular function, and then followed them for roughly 5 years (NEJM 2009;online November 25, 10.1056/NEJMoa0805299).
• Cardiac troponin is a “crucial marker” of acute MI and should be used for risk stratification, but it can also be released in clinical conditions other than AMI (Eur Heart J 2010; DOI:10.1093/eurheartj/ehq251)……the release of troponin is highly specific for myocardial injury and “indicates serious and probably irreversible injury,” but that any type of injury, not just ischemic, can result in the release of troponin into the blood……damage secondary to ischemia, such as arrhythmias or chronic heart failure; damage not related to ischemia such as myocarditis or severe burns; and damage from indeterminate or multifactorial conditions such as renal failure are all the possible causes of elevations of troponin in the absence of overt ischemic damage.
• A study on 15,133 adults aged 45 or older (51.5% women) found that elevations in peak postoperative troponin levels after noncardiac surgery were significantly associated with 30-day mortality (JAMA 2012;307:2295)….clinical trials are needed to establish whether interventions based on elevated troponin measurements can reduce risk in individual patients….As peak troponin levels increased, so did 30-day mortality:
• 0.01 ng/mL or less, 1% mortality.
• 0.02 ng/mL, 4%.
• 0.03 to 0.29 ng/mL, 9.3%.
• 0.30 ng/mL or more, 16.9%.









