Chapter 34 Meningitis and Encephalitis in the Intensive Care Unit
Meningitis
4 What host factors are important to consider regarding risk and cause for acute bacterial meningitis?
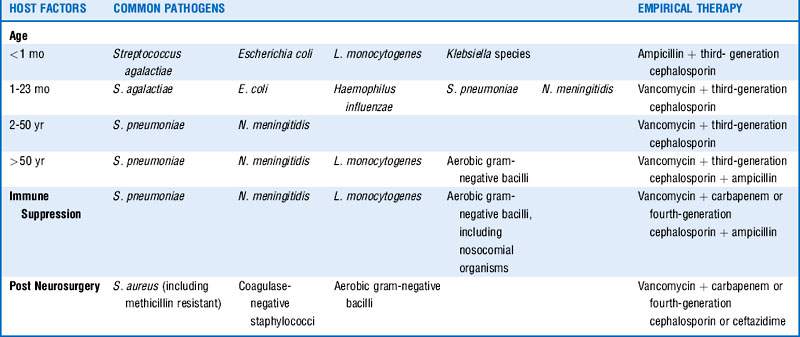
Factors such as age, immune deficiency or suppression, recent central nervous system (CNS) instrumentation, and possible exposures should be considered and will influence empirical therapy. See Table 34-1.
5 What are the most common causes of community-acquired acute bacterial meningitis in adults?
Table 34-2 includes the most common organisms in descending order based on case series with preferred antimicrobial therapy and suggested duration of treatment.
Table 34-2 Most Common Causes of Community-Acquired Bacterial Meningitis in Adults
| Pathogens | Preferred antimicrobial | Suggested duration of therapy |
|---|---|---|
| S. pneumoniae PCN MIC < 0.1 mcg/mL PCN MIC 0.1-1 mcg/mL PCN MIC ≥ 2 mcg/mL | PCN or ampicillin Third-generation cephalosporin Vancomycin + third-generation cephalosporin | 10-14 days |
| N. meningitidis PCN MIC < 0.1 mcg/mL PCN MIC > 0.1 mcg/mL | PCN or ampicillin Third-generation cephalosporin | 7 days |
| L. monocytogenes | Ampicillin or PCN | ≥ 21 days |
| Streptococcus agalactiae, pyogenes | Ampicillin or PCN | 21 days |
| S. aureus | MSSA → nafcillin, oxacillin MRSA → vancomycin | 14 days |
| H. influenzae β-Lactamase negative β-Lactamase positive | Ampicillin Third-generation cephalosporin | 7 days |
MIC, Minimum inhibitory concentration; MSSA, methicillin-sensitive S. aureus; PCN, penicillin.
10 Is there harm in awaiting CT and LP results before initiating therapy?
 Initiate antibiotic therapy and steroids.
Initiate antibiotic therapy and steroids.
 Obtain CT of head, and perform LP if safe. CSF cultures may be affected by pretreatment with antibiotics before lumbar puncture, but CSF findings including cell counts, chemical analyses, and Gram stain should remain helpful. Van de Beek, in his review, noted that yield of Gram stain was similar in patients who had been treated with antibiotics before LP as compared with those who had not.
Obtain CT of head, and perform LP if safe. CSF cultures may be affected by pretreatment with antibiotics before lumbar puncture, but CSF findings including cell counts, chemical analyses, and Gram stain should remain helpful. Van de Beek, in his review, noted that yield of Gram stain was similar in patients who had been treated with antibiotics before LP as compared with those who had not.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree