10
Maxillofacial injuries
Anatomy and physiology
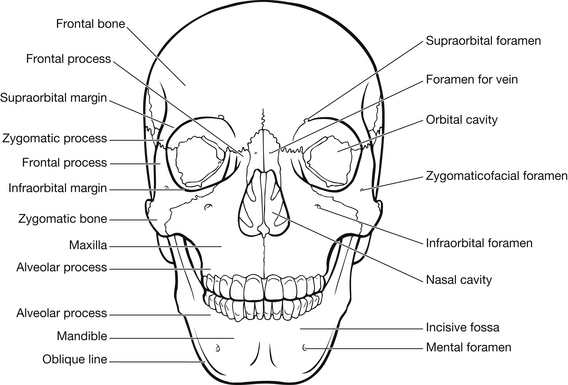
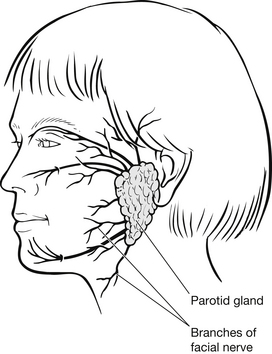
The face contains special structures and centres for airway, breathing, smell, speech, vision, hearing, mastication and facial expression (Parkins 2005) (Box 10.1, Fig. 10.1). Branches of the seventh cranial (facial) nerve provide sensory, parasympathetic and motor innervation to the face (Marieb 2001, Bickley et al. 2005) (Fig 10.2). Due to the location and superficial distribution of the facial nerve branches, these are often damaged in maxillofacial trauma. The face is highly vascular with the blood supply derived from branches of the internal and external carotid arteries. Venous drainage of the face, head and neck is collected through branches of the external and internal jugular veins and the vertebral vein (Marieb 2001, Bates et al. 2005). The face is vulnerable to a wide variety of injuries that can compromise the airway, cause haemorrhage, disrupt the appearance and impact on the ability to express emotions.
The diagnosis and treatment of maxillofacial injuries depends on the type of injury involved; therefore it is crucial to understand the anatomy and physiology of the injured area and mechanism of injury.
Mechanism of injury
Maxillofacial injuries result from blunt or penetrating trauma. Blunt injuries are more common and are caused by motor vehicle crashes, interpersonal violence (including domestic violence), sport activities, occupational trauma and falls (Macken 2009). Penetrating injuries are less common and include motor vehicle crashes, gunshot wounds, stabbings and explosions (Taylor & Dawood 2006, McQuillan & Thurman 2009). Mass, density and shape of the striking object, as well as speed of impact, directly affect the type and severity of facial injury. The amount of force required to fracture various facial bones may be classified as high impact (greater than 50 times force of gravity [g]) or low impact (less than 50 g) (Box 10.2).
It is generally accepted that the greater the speed of the motor vehicle the greater the maxillofacial injury. A history of a broken windscreen, damaged dashboard, and steering wheel deformity is associated with head, facial and laryngotracheal injuries. Although airbags and seatbelts have reduced the incidence and severity of maxillofacial injuries in motor vehicle crashes, facial lacerations, abrasions and burns are now more common with airbag deployment (Leslie & Skapetis 2007). Helmets are found to be effective in reducing head injuries, facial injuries and death in motorcycle crashes when compared with wearing no helmet; however, full-face helmets do not appear to have a significant effect on facial injuries when compared with open-faced helmets (Liu et al. 2009). Maxillofacial injuries caused by interpersonal violence account for many emergency department attendances. Studies in the US, Western Europe and Australia show that the majority of facial injuries occur in young males in the late teens to early 20s age group (Parkins 2005, Leslie & Skapetis 2007). The diagnosis and treatment can often be made more complex as alcohol intoxication plays a major part in many altercations; however, injuries tend to be less severe than those following road traffic accidents (Magennis et al. 1998, Elder et al. 2004).
The facial bony structures and sinus cavities offer protection to the brain and will collapse under force, expending energy away from the brain. The attachments of facial muscles also assist to expend this energy away by exerting downwards and backwards force to the maxilla. The mandible is often described as one of the strongest bones of the body; however, the condylar necks are frequent fracture sites as they absorb energy forces directed towards the brain. The incidence of maxillofacial injuries are less common in children, representing approximately 5–10 % of all cases, with the rate increasing with age. This is due in part to the resilience and elasticity of paediatric facial tissues and the usually protected, supervised environment given to younger age groups (Simpson & McLean 1995). When injury does occur, the pattern differs from adults as the relatively large cranium of the child protects the facial bones.
Airway assessment and management
Assessment of the patient requires a systematic approach such as advocated by the Advanced Trauma Life Support (ATLS) principles to identify and treat early any life-threatening injuries (Edwards 2005, American College of Surgeons 2008).
A thorough history is essential, with emphasis on those components that may impact on the assessment and subsequent management of the facial injuries and include, i.e., the mechanism of injury, alteration in mental status or loss of consciousness, if the patient has any allergies, their medical history and current medications (including prescription, non-prescription and recreational drugs), and last time the patient ate and drank (Hutchinson et al. 1996).
Initial airway assessment involves a rapid but thorough examination of the face, mouth and throat to identify any cause of obstruction such as foreign material, burns, lacerations and fractures (American College of Surgeons 2008). Obstruction may occur instantaneously or slowly, as oedema, secretions and bleeding progressively occlude the airway. Upper-airway obstruction is most commonly due to the tongue and foreign bodies, including vomitus, blood, dislodged teeth, broken dentures, oedema of the area surrounding the epiglottis and, uncommonly, injury to the larynx. During unconsciousness, tone is lost in the muscles that normally hold the tongue away from the pharyngeal wall. Abnormal or prolonged relaxation of these muscles will allow the tongue to prolapse back, obstructing the upper airway. Signs and symptoms of airway obstruction including agitation, combativeness, the use of accessory muscles, intercostal retractions, dyspnoea, stridor, gurgling, cyanosis, and a SaO2 less than 96% (Keane 2007, American College of Surgeons 2008).
Airway obstruction can be alleviated by either the chin-lift manoeuvre or the jaw-thrust manoeuvre to move the mandible anteriorly and thereby lifting the tongue. Both manoeuvres should not hyperextend the neck or compromise possible cervical spine fractures (American College of Surgeons 2008). Intubation may be inevitable where the patient has a decreased level of consciousness (Glasgow Coma Score of 8 or less), has poor gag, swallowing or coughing reflexes, or has difficulty in maintaining a patent airway or adequate oxygenation. Intubation is often difficult as the head must be maintained in a neutral position with in-line immobilization of the spine during the procedure. Performance of non-traumatic intubation is vital, as traumatic insertion causes increased intracranial pressure, which underlines the need to obtain experienced specialist help. The nasopharyngeal route should normally be avoided unless basilar skull fracture has been excluded. If attempts at intubation are unsuccessful, a cricothyrotomy or tracheostomy may be undertaken (American College of Surgeons 2008). While suctioning remains the primary method of clearing secretions, extreme care is needed so as not to stimulate the gag reflex or aggravate existing injuries. Where appropriate, the fully conscious patient may be allowed to hold their own suction catheter, thereby controlling the build up of secretions and eliminating the risk of over stimulation.
Examination
If there is no airway obstruction and the patient is haemodynamically stable, a systematic examination of the head and face can be performed (Box 10.3). Careful inspection and palpation of the scalp is undertaken for injuries and foreign bodies (such as glass and dirt) hidden by the hair. The head and face are inspected and palpated for bleeding, crepitus, bony irregularity, tenderness and soft tissue swelling. Visual acuity and extraocular movements are assessed to detect cranial nerve damage, globe rupture and extraocular muscle injury or entrapment. Diplopia may indicate the presence of an orbital floor fracture (Box 10.4).
The ears and mastoid areas are inspected for ecchymosis (Battle’s sign), lacerations, bleeding or discharge. Perforation of the eardrum, bloody or serous otorrhoea, haemotympanum and bilateral periorbital haematomas (‘panda’ or ‘raccoon’ eyes) are suggestive of a basilar skull fracture (Criddle 1995, McQuillan & Thurman 2009). The nose is examined for alignment, deformity, pain, swelling, ecchymosis, septal haematoma, epistaxis, rhinorrhoea and difficulty in breathing. The presence of bleeding and leakage of cerebrospinal fluid (CSF) are also suggestive of a basilar skull fracture. Thin, watery, nasal discharge should be considered CSF leakage until proven otherwise and the halo or dextrostix test should be undertaken. Nasal endotracheal and nasogastric tubes should not be inserted in the presence of a basilar skull fracture due to the risk of these being lodged intracranially or further aggravating the fracture.
The mouth is examined for fractures, subluxations and avulsions of the teeth as well as lacerations and contusions. Jaw malocclusion is assessed by checking for pain, malalignment, range of motion and loss of strength (Parkins 2005, Macken 2009).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree