Fig. 7.1
Glostavent® portable anesthesia machine; oxygen concentrating capacity may be added on
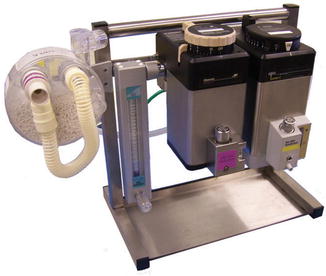
Fig. 7.2
G.A.S./U.V.S. portable anesthesia unit, with two vaporizers, variable flow meter, and CO2 scavenging capability to permit semi-closed circuit
Similar to the anesthesia machine situation, local physiologic monitors may not be as contemporary as desired. Lacking capnography and pulse oximeter probes for small children, they may be unsuitable for general and especially pediatric use. NGO supplied monitors may permit team anesthesiologists to provide the same standard of monitoring that a patient at home receives.
The type of proposed surgeries, number of operating rooms (ORs) and operating days, patient population, and ages need to be known or carefully speculated to determine types and amounts of supplies. While purchasing local supplies can save shipment space and costs, or extend care when transported supplies run out, caution must be taken. Local safety control measures and oversight may be lacking, and labeling in a different language can be problematic. Teams should plan amounts of supplies as if single-use disposables will be used only once, though some devices may be safely reused.
Well-established organizations will have equipment and supply lists that include basic anesthesia equipment, as well as mission-specific lists that vary according to type of surgery and location. Specific types of missions may require all general anesthetics (GA) with breathing tubes (e.g., cleft lip/palate), while others may rely heavily on neuraxial techniques with GA backup (e.g., gynecologic surgery). Yet others may rely heavily on peripheral nerve blocks, such as is suitable for hand surgery. As much as possible, bringing individual procedure supply components instead of procedure kits can drastically cut down on the amount of waste [9]. Proper planning for type and number of anesthetics will ensure adequate supplies are on hand to maximize human resources, and prevent shipping of unnecessary supplies which may or may not be useful to the host team. Table 7.1 provides a sample basic anesthesia equipment list that may serve as a starting point for planning.
Type of equipment | Specific equipment |
|---|---|
Anesthesia delivery | • Anesthesia machine with calibrated vaporizer • Machine circuits • CO2 scavenging supplies • Gas analyzer • +/− continuous drug infusion pumps • +/− portable ultrasound machine |
Monitors/lab | • Standard ASA: continuous pulse oximetry, end-tidal CO2, automated noninvasive blood pressure, and multilead ECG (with lead pads); temperature monitoring and probes available • Twitch monitor • +/− invasive hemodynamic monitors • Point-of-care blood analyzer with adequate cartridges (caution: require refrigeration) |
Airway management | • Facemasks, assorted sizes • Anesthesia circuits, appropriate size • Laryngoscope, blades, assorted sizes • Batteries, light bulbs • Video laryngoscope, blades, stylets assorted sizes • ETTs, stylets, assorted sizes • LMAs, assorted sizes • Bougies, assorted sizes • Ambu bag, appropriate size • EtCO2 disposable detector • Suction tubing and instrument • Oral airways, nasal airways, assorted sizes • Nasal cannula, non-rebreather masks • Hydrogel |
Vascular access | • IV catheters, assorted sizes • Tape and occlusive dressings • Tubing, appropriate type and size • Syringes, assorted sizes • Stop cocks • Alcohol swabs or alcohol solution and cotton swabs • +/− invasive |
Emergency equipment | • Ambu/self-inflating bag • Cricothyrotomy kit • Intraosseous needle • Defibrillator, pads appropriate sizes • Portable oxygen tank • LMAs, assorted sizes • Bougie • Stat laboratory for point-of-care testing • Flashlights and batteries • Portable fiberoptic bronchoscope |
Regional anesthesia supplies | • Ultrasound gel • Stimulatable needles, assorted sizes • Spinal and epidural needles, assorted sizes • Sterile drapes • Sterile prep • Sterile cotton • +/− spinal, epidural, PNB kits (Note: kits generate more waste than components) |
Equipment/maintenance | • Portable autoclave, indicator strips • Cleaning solutions, waste neutralizer • Bottle brushes • Tools • Repair kits |
Device Procurement
Medical devices may be obtained for medical missions in a variety of ways, including pilfering from home institutions (not recommended), collecting opened but unused items from one’s own hospital, appealing to manufacturers for donations of capital equipment and supplies, fundraising to purchase materials, and through organizations that collect and manage larger scale medical equipment and supply donations to facilitate efficient and reliable distribution for those in need.
US hospitals generate more than 5.9 million tons of medical waste each year [10]. Much of that waste consists of unused medical supplies that are opened and unused but no longer sterile even if they have never contacted patients. Due to legal concerns and Food and Drug Administration (FDA) regulations, these supplies are not usable or resalable in the U.S. but may be enthusiastically accepted by many US-based charitable organizations for use in the developing world where they are so desperately needed. Supplies in opened packaging are re-sterilized and repackaged by donor institutions, then collected for distribution. R.E.M.E.D.Y. [11], Recovered Medical Equipment for the Developing World, founded by Dr. William Rosenblatt in 1991, was the first such not-for-profit organization dedicated to actively promoting the recovery of unused medical supplies for the purpose of global aid, pollution prevention, and cost-effectiveness. In addition to R.E.M.E.D.Y., many other not-for-profit medical equipment and supply organizations exist, including MedWish, MedShare, Procure, Afya Foundation, Intervol RUMS, IMEC International Medical Equipment Collaborative, and AWH Advocates for World Health. Some organizations focus on acquisition of supplies, and others on repurposed capital equipment [12].
The bulk of equipment and supplies for medical missions are procured through not-for-profit donation organizations. Institutions and manufacturers are often approached to fill supply gaps. It is possible to solicit donations of refurbished equipment from manufacturers, or borrow equipment from them for specific missions, such as portable ultrasound machines or echo machines. Mission groups typically house a central supply space from which all trips are stocked. Responsibility is with the mission organization to arrange and pay for shipment to final destinations.
Transportation of Supplies
Substantial advanced planning is required to ensure surgical and anesthesia supplies arrive intact and in a timely fashion. Supplies are gathered from donors, sorted, and then boxed. Historically, airlines used to be very generous with providing shipping. Boxes could be sent by general carrier with or without the team, free of charge. Gradually that largesse has disappeared. Some organizations have been able to piggyback supplies with the shipments of willing companies that regularly do business in the host country, allowing both economy and efficiency. In general, the bulk of supplies travel with mission team members, who must maximize opportunities to check supplies as personal luggage. Additional supplies are shipped separately, and overall thousands of dollars are now commonly spent on shipping of supplies for each mission. As a result of shipping expenses, fewer dollars exist for NGOs to fulfill their annual mission goals. Mission groups have been forced to reconsider their model for materials procurement, and to look hard for what can be safely and reliably sourced locally. Not only do these types of efforts save money, but they also reduce pollution by reducing shipping, as well as reducing manufacturing, use, and disposal of excess supplies. As noted, local procurement must proceed with caution.
For materials that will travel with the team, shipping arrangements should consider the timing, possible delays, and meticulous documentation for customs agents. Endorsement letters from government agencies or internationally recognized charities may facilitate transit through customs. Materials beyond their expiration dates should not be shipped, and open packages should be avoided because the discovery of even one may provoke confiscation of the entire shipment. Similarly, controlled substances should not be mixed with equipment supplies. Strict guidelines also exist regarding shipment of flammable and explosive substances, which must be sourced locally. If shipments are not timed appropriately, mission teams may be forced to scramble “on the ground” to purchase local materials at increased expense and waste of transportation and supplies that may not be usable without the mission team. Once the supplies arrive in the host country, with or without the team, they are brought to the hospital and stored. Advanced planning for secured transportation and storage locations is required to avoid theft, damage, loss, and waste.
Equipment Maintenance and Cleaning for Responsible Reuse
There is growing concern regarding the amount of waste generated in the ORs, which indirectly impacts public health and healthcare costs to society. Upwards of 1/3 of the 5.9 million tons of annual hospital waste in the U.S. originates in ORs [2, 9]. Strategies to reduce waste are critical to protect society from illness stemming from pollution, and to prevent the production of greenhouse gas formation through burning of fossil fuels for resource extraction, de novo manufacturing, and through waste incineration. Strategies that reduce waste save money directly in purchasing costs, and indirectly through prevention of illness and loss of productivity [2, 13–15].
Use of single-use disposable medical equipment is proliferating in the U.S., faster than anywhere else in the world. The reasons are multifactorial, and typically include cheaper purchase price though this neglects to consider that higher upfront costs of reusables are offset by numbers of reuse. Other reasons for selection of disposable devices include concern for infection prevention. For highly infectious patients, and for hard to clean items such as needles and IV tubing, disposables are warranted. However, indiscriminate broad use of disposables appears unwarranted as there is a paucity of evidence to support reduction of infection rates over properly cleaned reusables. The biggest reason for the trend toward disposables likely is due to the convenience of throwing used supplies away rather than cleaning them [16]. Upholding high standards of infection prevention during administration of anesthesia in underserved areas is critical; however caution must be taken to prevent the exportation of wasteful behaviors that are commonplace in the U.S.
Reduce
The primary resource conservation strategy both at home and abroad starts with opening and using less supplies whenever feasible. While humanitarian organizations noted above thrive on the excesses of the US health system as a source of medical supply donation and equipment refurbishment, waste reduction strategies in the U.S. must not be avoided to support their cause. When REMEDY was first instituted at Yale, OR nursing staff reported the program raised awareness of wasteful practices and staff consciously worked to open fewer materials while successfully collecting supplies. Over time, however, they anecdotally reported that they reverted to original wasteful habits and rationalized, “I’ll just donate excess supplies so they won’t go to waste.” Unfortunately, only select supplies are desired by equipment donation organizations and so this attitude is misguided. Typically, medical missions provide an excellent opportunity to learn how to provide safe care with fewer supplies, and conservation practices ought to subsequently impact behaviors at home institutions.
In addition to clinical waste, another important opportunity for mission teams to reduce usage is through implementation of reusable food and beverage containers. One NGO provided each team member with a reusable coffee mug with the organization logo on it to help reduce waste, encourage conservation mindedness, and as a mission keepsake.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





