Chapter Five Massage based outcomes and assessment
Chapter contents
Introduction
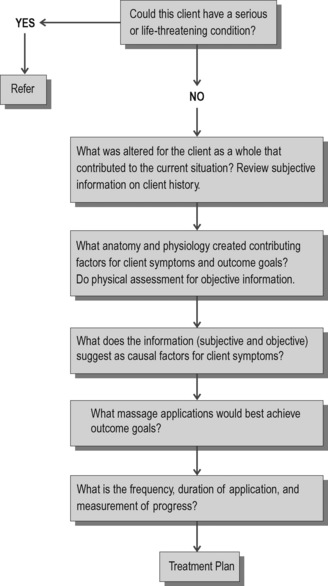
Assessment is a process of asking relevant questions and performing activities and then testing to answer those questions. Once a person has been able to obtain an accurate diagnosis of the pain condition and massage is recommended, then the massage therapist needs to perform assessment to determine the dysfunctional aspects that best respond to massage as well as to determine how massage will be delivered to support other treatments. Since massage has been shown through both clinical experience and scientific research to have beneficial outcomes for those with pain, it is important to be able to assess accurately for the factors that can be addressed by massage and to know when to refer the person for necessary medical treatment.
Clinical reasoning
We start with a health history and physical assessment. These procedures provide a great deal of information, but information alone does not solve the puzzle; it is just one of the pieces of the puzzle. We have to use our logic and intuition to sort and categorize the pieces of information to determine both the beginning and ending points. This sorting is the beginning of a clinical reasoning process.
• Recognizing the nature of the client’s reason for massage by clearly defining the outcome. Define the problem.
• Collecting and analyzing information related to the client and their outcome for massage. Collect the facts and do research.
• Evaluating information relative to the specifics of the client and brainstorming potential interventions. Generate possibilities.
• Drawing conclusions and making decisions. Develop an intervention plan.
Begin at the end – what is the outcome?
An individual may remain in pain but tolerance increases so they are able to perform daily work activities more effectively.
The cause of the pain condition – trigger point activity or myofascial shortening for example – can be altered resulting in pain reduction.
The individual’s pain threshold and tolerance remain unaltered but palliative measures mask sensation temporarily or reduce the suffering.
The painful condition remains but the individual is better able to cope because they are less anxious or depressed.
1. General full body massage. Outcomes – support autonomic nervous system balance (Box 5.1), normalize breathing, support production and utilization of neurochemicals that alter pain (i.e. endorphins, serotonin), support restorative sleep though relaxation and overriding painful sensation with pleasurable sensation, and develop a supportive therapeutic relationship.
2. Massage targeting the cause of pain. This is more of a mechanistic approach to massage. The methods attempt to change the anatomy or physiology that is causing the pain. Muscle tension can come from postural strain, scar tissue development, movement dysfunction, breathing dysfunction, trigger point activity, fascial tone issues, and circulation issues.
Outcomes for massage
How do you want to feel or what do you want to be able to do?
The three basic outcomes for massage are:
Assessment
Pain plan of care
A pain plan of care (i.e. treatment plan) should include a description of the pain treatment methods that will be utilized, their frequency, treatment goals, methods that will be used to measure progress towards the stated goals, and evidence that the person with pain was involved in the development of the pain treatment plan. The care plan needs to be reviewed and revised whenever significant changes in the person’s condition are observed, or when the treatment methods selected have not been effective.
In order to determine the appropriate treatment for pain, several questions apply:
Assessing pain
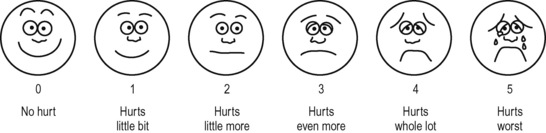
See Figure 5.2 for an example of a pain rating scale. The simplest measuring device, the verbal rating scale (VRS), records on paper, or a computer, what a patient reports whether there is ‘no pain,’ ‘mild pain,’ ‘moderate pain,’ ‘severe pain,’ or ‘agonizing pain’.
Numerical rating scale (NRS)
This method uses a series of numbers (0–100 or 0–10).
• Worst pain possible would equal the highest number on the scale.
• The patient is asked to apply a numerical value to the pain.
Visual analogue scale (VAS)
• The zero end of the line equals no pain at all.
• The 10 cm end equals the worst pain possible.
• The patient marks the line at the level of their pain.
• The VAS can be used to measure progress by comparing the pain scores over time. The VAS has been found to be accurate when used for anyone over the age of five.
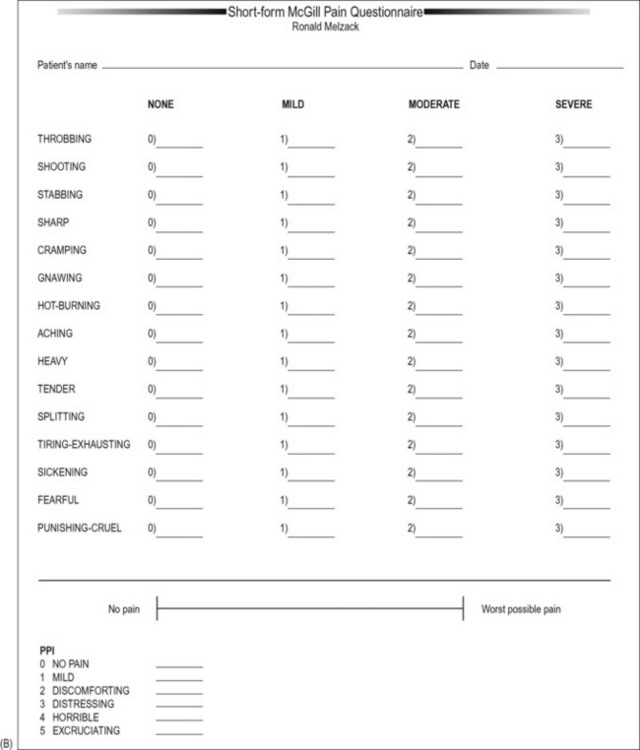
Questionnaires
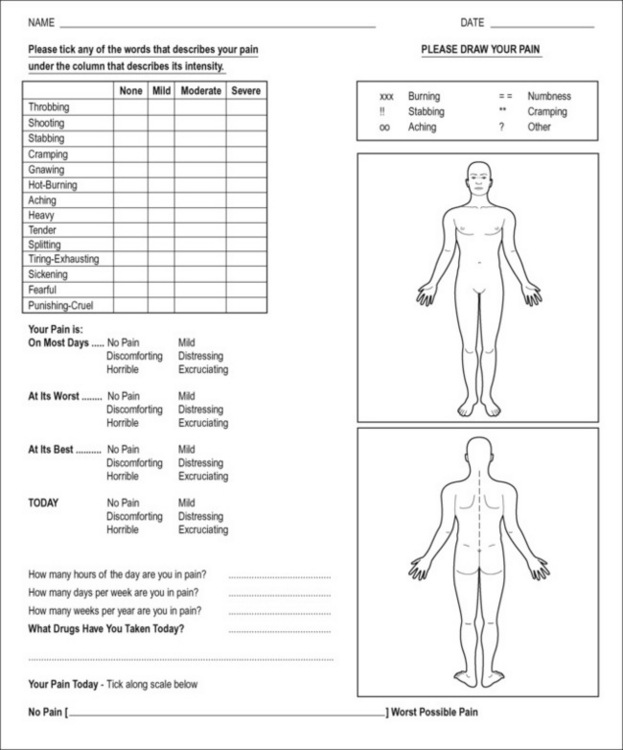
A variety of questionnaires exist, such as the McGill Pain Questionnaire and the Short McGill Questionnaire (and many others) (see Figs 5.3 & 5.4)
Pain drawings
It can be useful for the patient to color the areas of their pain on a simple outline of the human body using a red pencil (see Fig. 5.3). The shaded or colored areas can be very useful when searching for trigger points during a massage.
A single sheet of paper can easily contain a VAS, a shortened McGill Questionnaire, as well as a series of simple questions such as those illustrated in Figure 5.4.
Pain threshold
• Applying pressure safely requires sensitivity.
• We need to be able to sense when tissue tension/resistance is being ‘met,’ as we palpate, and when tension is being overcome.
• When applying pressure you may ask the patient ‘Does it hurt?,’ ‘Does it refer?’
• To make sense of the answer it is important to have an idea of how much pressure you are using.
• The term ‘pain threshold’ is used to describe the least amount of pressure needed to produce a report of pain, and/or referred symptoms, when a trigger point is being compressed.
• It is important to know how much pressure is required to produce pain, and/or referred symptoms, and whether the amount of pressure being used has changed after treatment, or whether the pain threshold is different the next time the patient comes for treatment.
• It would not be very helpful to hear: ‘Yes it still hurts’ only because we are pressing much harder!
How can a person learn to apply a particular amount of pressure, and no more? It has been shown that using a simple technology (such as bathroom scales), physical therapy students can be taught to accurately produce specific degrees of pressure on request. Students are tested applying pressure to lumbar muscles. After training, using bathroom scales, the students can usually apply precise amounts of pressure on request (Keating et al 1993).
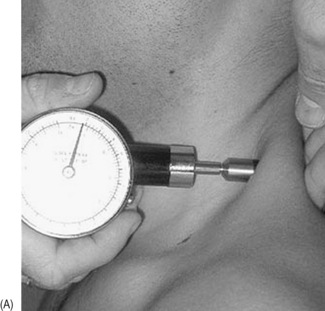
Algometer
A basic algometer is a hand-held, spring-loaded, rubber-tipped, pressure measuring device that offers a means of achieving standardized pressure application.
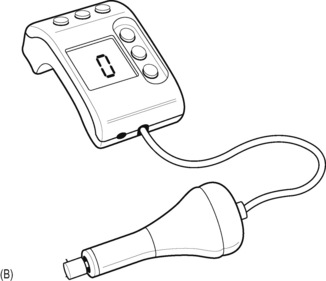
An electronic version of this type of algometer allows recording of pressures applied, however these forms of algometer are used independently of actual treatment, to obtain feedback from the patient, to register the pressure being used when pain levels reach tolerance, for example (see Fig. 5.5A & B).
A variety of other algometer designs exist, including a sophisticated version that is attached to the thumb or finger, with a lead running to an electronic sensor that is itself connected to a computer. This gives very precise readouts of the amount of pressure being applied by the finger or thumb during treatment (see Fig. 5.5C & D).
Baldry (2005) suggests that algometers should be used to measure the degree of pressure required to produce symptoms, ‘before and after deactivation of a trigger point, because when treatment is successful, the pressure threshold over the trigger point increases.’ If an algometer is not available, and in order to encourage only appropriate amounts of pressure being applied, it may be useful to practice simple palpation exercises.
Emotional distress
Significant pain often is accompanied or preceded by emotional distress and pain related fear. Emotional status and traits can have a significant impact on treatment outcome. Thus, comprehensive pain outcomes approaches should include methods to assess the varieties of emotional distress. There are numerous emotional distress instruments available for use and the psychologist is the most logical person to assess this area.