226 Mass Critical Care
The devastating events of September 11, 2001, in the United States, subsequent acts of bioterrorism, and emerging infectious disease pandemics have brought new challenges to the field of disaster management and multidisciplinary hazard mitigation. Even though war- and terrorism-related disasters have gathered much attention recently, natural disasters have occurred with increasing frequency over the past decades. This has been attributed to the growth of human populations in geographically disaster-prone areas, rapid industrialization, and increasing exposure to toxic and hazardous materials.1–3
Analyses of the response of different healthcare systems to major disasters in the past have demonstrated the need for a more clearly identified planning process to attend to the response to multihazard events.4 This provides a basic understanding of common disaster scenarios and highlights the role of the intensivist in the medical response to disasters. It is important for the practicing critical care clinician to keep in mind that their role is first and foremost as a first receiver, rather than first responder; a well-trained intensivist may be of much greater value remaining in the hospital setting rather than quickly mobilizing to the field, where their lack of situational preparedness may make them more of a hindrance than an asset.5
 Background
Background
Major disasters occur regularly and cause widespread human death and suffering. Over the past 2 decades, more than 3 million lives have been lost worldwide to major disasters. A total of 39,073 persons were reported killed by disasters alone in 2001, with the decade’s annual average of around 62,000. Even though the numbers of geophysical disasters such as earthquakes and volcanic eruptions have remained fairly constant over the past decade, the past 2 years have seen the highest number of weather-related disasters reported over the decade.6 As populations grow and occupy spaces that are vulnerable to different hazards, disasters will increase in severity and impact. Recent events since the September 2001 terrorism attacks have brought attention to the effects of manmade disasters on the healthcare system and the need to anticipate and plan for such low-probability yet catastrophic events. Even though there is basic similarity in the response to various hazardous events, each type of disaster presents responders with unique demands. After any disaster, healthcare systems are tasked with preventing excessive deaths, mitigating suffering, and dealing with often overwhelming inadequacy of resources. Over the past few years, disaster medicine has thus grown into a unique specialty to deal with planning and preparing for such cataclysmic events. It shares a common ideal with public health: “greatest good for the greatest number.”3
 Terminology
Terminology
Physicians and healthcare personnel should be familiar with basic nomenclature and terminology in disaster medicine. Clear, common, and concise definitions are important to effective communication and evoking appropriate responses to disaster situations. Uniform use of terminology across healthcare systems provides a basis for analysis and construction of an effective disaster plan and response by all responders.7 Controversies surrounding the definitions of disasters, hazards, and causalities are included in the discussions that follow.
The word disaster connotes a subjective assessment that has various meanings to different people and has an inherent bias, depending on the person using it. For example, a local, state, or federal “disaster declaration” implies commitment of financial and other resources. Similarly, a disaster in one community is not necessarily the same to another. Currently there is no uniformly accepted definition for the word disaster.7 De Boer recognizes the lack of a meaningful definition for the word and proposes instead the term medical severity index (MSI).8 This term, however, has not gained sufficient acceptance for routine use. Different modifiers can lead to different definitions of the term disaster. They include the type of disaster, geographic area involved, timing, onset of the event, size of the community affected, baseline resources available to the community, and finally, the physical, psychosocial, and economic injury caused by the event. However, from a healthcare standpoint, the most important variable that defines a disaster is its functional impact on the healthcare facility.7 Despite various attempts to clear the confusion surrounding the terminology, the issue remains unresolved.7,9–10 What follows are the commonly used definitions in disaster medicine from a healthcare perspective:
 Classification of Disasters
Classification of Disasters
Natural disasters arise from forces of nature and include earthquakes, volcanic eruptions, hurricanes, floods, fire, and tornadoes. In addition, infectious disasters can be classified as epidemic or pandemic and are discussed elsewhere. Manmade disasters are due to identifiable human causes and may be further classified as complex emergencies (e.g., wars, terrorist attacks) and technological disasters (e.g., industrial accidents, explosions from hazardous material).15 Other classifications include those based on onset (acute versus insidious disasters), predictability, duration, and frequency. From a public health perspective, disasters have to be defined by their effect on people and the healthcare system. The concept of functional impact to the healthcare system is thus paramount.15–16
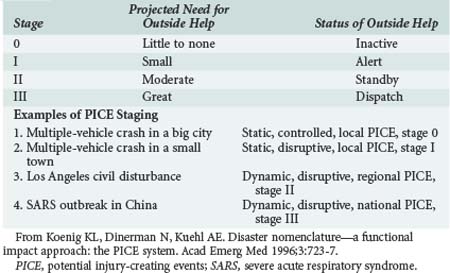
The PICE system attempts to create uniformity to address the wide spectrum of situations.7 The two major aims of this system are to effectively communicate both the operational consequences to a hospital or community and the type and amount of outside assistance needed. Four modifiers for an event are chosen from a standardized group of prefixes, and a stage is assigned (Table 226-1). Column A (first prefix) describes the potential for additional casualties. For example a finite number of persons injured in an airplane crash is a “static event,” whereas an ongoing fire is a “dynamic” event. Column B (second prefix) describes whether local resources are sufficient (“controlled”) or overwhelmed. If they are overwhelmed, the two modifiers “disruptive” and “paralytic” indicate whether they must be simply augmented or totally reconstituted. Paralytic PICE are the most daunting of all situations, and they can be either destructive or nondestructive (Table 226-2). Column C describes the extent of geographic involvement. PICE stage refers to the likelihood that outside medical help is required (Table 226-3). This PICE model provides important concepts for disaster planners, researchers, and responders. Using this system, disasters can be described both prospectively and retrospectively. PICE is a valuable tool for use in planning and disaster mitigation, but the system warrants validation on a wider scale. It may also require further refinement to delineate the type of aid needed by an affected community.7
| A | B | C |
|---|---|---|
| Static | Controlled | Local |
| Dynamic | Disruptive | Regional |
| Paralytic | National | |
| International |
PICE, potential injury-creating events.
Data from Koenig KL, Dinerman N, Kuehl AE. Disaster nomenclature—a functional impact approach: the PICE system. Acad Emerg Med 1996;3:723-7.
| Destructive | Nondestructive |
|---|---|
| Bomb explosion | Snowstorm |
| Earthquake | Employee strike |
| Tornado | Power failure |
| Civil unrest | Water supply cutoff |
| HazMat spill | |
| Fire | |
| Building collapse |
HazMat, hazardous materials; PICE, potential injury-creating events.
Data from Koenig KL, Dinerman N, Kuehl AE. Disaster nomenclature—a functional impact approach: the PICE system. Acad Emerg Med 1996;3:723-7.
 Natural Disasters
Natural Disasters
Earthquakes
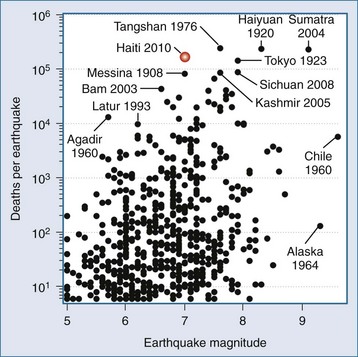
Earthquakes are a well-known and publicized model of a disaster that results in significant mortality,17 as can be seen in Figure 226-1 describing deaths from earthquakes since 1990. A homogenous population well trained in basic trauma and life support and the architectural design of the stricken area’s housing and public facilities are two major determinants of outcomes for earthquake victims. The massive earthquakes of the past 10 years in Turkey, Taiwan, Sumatra, Kashmir, Sichuan, and Haiti have shown us that sound engineering design for earthquake resistance in civil structures such as schools, hospitals, fire stations, and correctional facilities have a major impact on outcomes. In addition, urban earthquakes generate massive fiscal impact on the world in terms of reconstruction grants provided by wealthier countries for devastated urban areas. Moderately destructive earthquakes in the developing world usually cost up to $10 billion in reconstruction; the needs of developing countries with urban earthquakes may cost an order of magnitude more.
Responders from the very experienced Israel Defense Forces (IDF) air-deployed within 48 hours of the Haiti earthquake. This team had extensive experience over the years with international response and consists of 230 people. The team unpacked and built their portable hospital within 8 hours, and during 10 days of operation treated more than 1100 patients in a facility designed to provide 60 inpatient beds, including 4 intensive care beds and 1 operating room.18 Most of the first wave of casualties presented with crushed limbs with open infected wounds, with the later arrivals presenting with sepsis and poor chance of outcome. Despite the repeated experience from prior earthquakes showing that victims of crush syndrome and acute renal failure require emergency dialysis to prevent death, this facility relied on other international teams for dialysis. Their major dilemmas were practical implementation of the triage algorithm by military personnel to a civilian population. The simple priorities were urgency, resources available, and probability of saving life. Patients with brain injury, paraplegia due to spine injuries, or a low Glasgow Coma Scale score were immediately transferred to other facilities, since no neurosurgical capabilities were available. A triage panel of three senior physicians relieved individual physicians of personal accountability. Half of the intensive care capability was always dedicated to postoperative care, with the remaining 2 beds used for prolonged intensive care; only patients who were expected to stabilize within 24 hours were placed in these beds. The very early discharge policy permitted this military facility to treat more than 100 patients per day.
Second, let us consider the response of the U.S. military, which at this point had a considerable portfolio on providing international disaster relief in catastrophic events such as the Indonesian tsunami that devastated Sumatra. The United States Naval Ship (USNS) Comfort, one of Military Sealift Command’s two hospital ships, was deployed as part of the mission termed “Operation Unified Response.” It started accepting casualties within 7 days of the earthquake. The ship is a 1000-bed facility which includes 75 intensive care unit beds, blood bank, hemodialysis, pathology, physical therapy, morgue, and radiology with computed tomography and ultrasonography capability. It is staffed with 1000 active-duty U.S. medical personnel, including three physician intensivists, and it was allocated to stay up to 6 months.19–20
Third, let us consider the relearning of the lessons of civil-military collaboration in disaster response.21 A volunteer medical team with civilian personnel under the auspices of the international medical corps flew to the Dominican Republic and reached Hopital de l’Universite d’Etat d’Haiti in Port-au-Prince after a long bus ride on January 17. There were more than 800 injured in the partially destroyed facility, with the primary diagnoses being crush injuries, compartment syndrome, infected fractures, and hemorrhagic shock. One physician and one nurse were covering up to 80 critically ill patients in the wards. An aftershock of 5.9 magnitude resulted in an exodus of casualties and higher rates of heat stroke in dehydrated hypovolemic patients exposed to tropical temperatures. Destruction of the prison system released some 4000 criminals into the community, and no security was available until arrival of a U.S. airborne infantry regiment. With arrival of the USNS Comfort on January 20, evacuation of the most critically ill patients started, but a triage list developed rapidly, with ship facilities accepting preferentially complicated injuries, obstetric patients, and maxillofacial injuries. Patients with pelvic fractures, closed head injuries, complete spinal cord lesions, and mechanical ventilation cases were of too-high acuity for the USNS Comfort. Family structures became fragmented as separation of children from parents occurred. Yet the collaboration of civilian and military medical personnel was considered a success.
Next, let us consider the experiences of academic centers delivering care to victims of the Haitian earthquake on-site.22 The Miller School of Medicine of the University of Miami and Project Medishare had the advantage of long experience of collaboration with Haiti as well as close geographic proximity, and they were able to provide emergency relief within 20 hours. Within 8 days, they were able to establish a field hospital at the city airport, and by January 21, 140 patients were transferred into the upgrade facility. The well-organized command center with satellite links for telephone and Internet access were available. A joint adult-pediatric triage team accompanied by Creole-speaking medical staff of Haitian origin was used. Multiple surgeries were performed under local peripheral nerve blocks, with guillotine amputations being frequent. Highest-acuity patients were transferred to the IDF field hospital or the USNS Comfort. The command center eventually provided psychiatrists to manage the posttraumatic stress syndrome and a buddy system for follow-up support.
Finally, one must consider the critical care response from New York City. While many small teams and a large volume of supplies were dispatched, an organized response was delivered under the leadership of Dr. Ernest Benjamin, division chief of critical care in surgery at Mt. Sinai Hospital. Dr. Benjamin, with close family ties to Haiti, arrived in Port-au-Prince 3 days after the initial event and after rapid assessment of needs and resources available, organized the deployment of the 27-member critical care team to his home country, which arrived on January 20. The team remained on-site for 2 weeks and was responsible for postanesthesia and postoperative care delivery, with Dr. Benjamin being deputized as the director of critical care and recovery at the national hospital. The home institution effectively secured anonymous donations of private jets able to transport the team personnel and some 3000 pounds of medical supplies per flight. The team delivered intensive care with minimal technology but with kindness and dignity towards the suffering population. This certainly was not a medical tourism venture but a true integrated response with both language and cultural sensitivities and capabilities, so important in catastrophic situations that will take decades for the local population to recover from.23
Experience in managing catastrophic international disasters continues to accumulate with unfortunate regularity. The preceding discussion suggests that combinations of dialysis, orthopedic surgery, pediatric trauma, security, transportation, posttraumatic stress treatment, and cultural and language sensitivities are crucial in earthquakes. Disasters produce well-defined syndromes with well-defined mortalities. It is the recovery phase that continues to require persistence and improvement. One of the most experienced managers and thought leaders in disaster management, Dr. Eric Noji, enumerated the most important factors in public health after disasters: environmental health, epidemic management, immunization, controlling the spread of HIV/AIDS, management of dead bodies, nutrition, maternal and child health, medical services, and thorough public health surveillance. It is a common error to deliver a few weeks of heroic quality care then abandon the population to the ravages of destroyed infrastructure, including public health organization.24
Volcanic Eruptions
A volcano is a hill or a mountain built around a vent that connects with reservoirs of molten rock below the earth’s surface.25 Different types of eruptive events occur, including pyroclastic explosions, hot ash releases, lava flows, gas emissions, and glowing avalanches (gas and ash releases). Lava flows tend not to result in high casualties, because they are easily avoidable. The “composite” type of volcano is associated with a more violent eruption from within the chimney. These eruptions are associated with air shock waves, rock projectiles (some with high thermal energy), release of noxious gases, pyroclastic flows, and mud flows (lahars). Pyroclastic flows and lahars are often fast moving and are the main cause of damage and deaths from volcanoes, as evidenced by the small eruption of the Nevado del Ruiz in Columbia that killed more than 23,000 people.26 The release of ash and its subsequent rapid buildup on building structures can be substantial, causing them to collapse within a matter of hours. Ash is also responsible for the clogging of filters and machinery, causing electrical storms and fires, and interfering with communications. Ash is a main cause for respiratory-related syndromes and conjunctival and corneal injury. A variety of toxic gases (e.g., carbon dioxide, hydrogen sulfide, sulfur dioxide, hydrogen chloride, hydrogen fluoride, and carbon monoxide [CO]) are released during eruptions, causing bronchospasm, pulmonary edema, hypoxemia, cellular asphyxiation, topical irritation of skin and other mucosal surfaces, and death.27 Damage to health infrastructures and water systems can be severe. Problems related to communication (ashes cause serious interference) and transportation (poor visibility and slippery roads) are likely. Depending on the initial assessment, various needs can be anticipated. Reducing the risk for vulnerable groups of being exposed to ash, raising awareness of the risk associated with ash (health and mechanical risk), and maintaining food security conditions over the long term (lava, ash, and acid rain cause damage to crops and livestock) can help minimize suffering.28
Hurricanes, Cyclones, and Typhoons
The large rotating weather systems that form seasonally over tropical oceans are variously named, depending on the geographic region where they form.29–31 They consist of a calm inner portion called the eye, surrounded by a wall of rain and high-velocity winds. Based on central pressure, wind speed, storm surge, and potential destruction, their severity is graded on a scale of 1 to 5 (Saffir Simpson scale).30 They are among the most destructive natural phenomena. Cyclones during 1970 and 1991 in Bangladesh claimed 300,000 and 100,000 lives, respectively, due to flooding.32 The most devastating hurricane ever to hit the United States was in 1900 at Galveston, Texas. It claimed an estimated 8000 to 12,000 lives.33 The greatest damage to life and property is not from the wind but from secondary events such as storm surges, flooding, landslides, and tornadoes. Ninety percent of all hurricane-related deaths occur from storm surge–related drowning.1 The most common injury patterns include lacerations (during the cleanup phase), followed by blunt trauma and puncture wounds. Late morbidity can be due to post-disaster cleanup accidents (e.g., electrocution), dehydration, wound infection, and outbreaks of communicable disease.31,34 Data from hurricane Katrina confirmed data from previous meteorological events: the leading mechanisms of injuries are fall, lacerations, and piercing injuries, with cleanup being the primary activity at the time of injury.35 Recent experiences in the aftermath of hurricane Katrina in 2005 indicate that resources may have to be provided for an extended period after the initial inciting event, and that significant resources may have to be provided for patients with chronic medical illnesses.34,36
Floods
There are three major types of floods: flash floods (caused by heavy rain and dam failures), coastal floods, and river floods. Together, they are the most common type of disasters and account for at least half of all disaster-related deaths.37,38 The primary cause of death is drowning, followed by hypothermia and injury due to floating debris.39,40 The impact on the health infrastructures and lifeline systems can be massive and may result in food shortages. Interruption of basic public services (e.g., sanitation, drinking water, electricity) may result in outbreaks of communicable disease.38,40 Another concern is the increase in both vectorborne diseases (e.g., malaria, St. Louis encephalitis) and displacement of wildlife (e.g., poisonous snakes and rodents).39,40
Landslides
Landslides are more widespread than any other geologic event. They are defined as downslope transport of soil and rock resulting from natural phenomena or manmade actions. Landslides can also occur secondary to heavy storms, volcanic eruptions, and earthquakes. Landslides cause high mortality and few injuries. Trauma and suffocation by entrapment are common. Pending an assessment, needs can be anticipated, such as search and rescue, mass casualty management, and emergency shelter for the homeless.41,42
Pandemic 2009 H1N1 Influenza a Virus
Within weeks, the virus quickly spread worldwide through human-to-human transmission. On April 26, 2009, the CDC’s Strategic National Stockpile began releasing 25% of the supplies in the stockpile for the treatment and protection from influenza.43 On June 11, 2009, the World Health Organization (WHO) declared the 2009 H1N1 influenza a global pandemic, generating the first influenza pandemic of the 21st century, with more than 70 countries reporting cases of H1N1 infection. By June 19, 2009, all 50 states in the United States, the District of Columbia, Puerto Rico, and the U.S. Virgin Islands had reported cases of 2009 H1N1 infection. More strikingly, the Centers for Disease Control and Prevention (CDC) Emerging Infections Program (EIP) estimated the number of hospitalizations and deaths in people 64 years and younger. The virus was most likely to strike children, young adults, and those with underlying pulmonary and cardiac disease. Pregnant women in their second and third trimester were also at high risk. Patients requiring intensive care had a remarkable prevalence of obesity.43
Influenza vaccines are most effective not only to prevent but also to mitigate the severity of illness. The pandemic H1N1 influenza vaccine was promptly developed by the WHO and national authorities. A national influenza vaccination campaign was launched in the United States in October 2009, and the first H1N1 vaccine was made available at that time. Despite the rapid response of the authorities, developing countries in the Southern Hemisphere experienced delays and shortages of the vaccines. Thus, recent research and developmental work have been encouraging for developing a “universal” influenza vaccine that could provide efficacious cross-reactive immunity and induce broad protection against different variants and subtypes of the influenza virus.44
To date, the preliminary data show that about 8% of H1N1 patients were hospitalized (23 per 100,000 population); 6.5% to 25% of these required being in the ICU (28.7 per million inhabitants) for a median of 7 to 12 days, with a peak bed occupancy of 6.3 to 10.6 per million inhabitants; 65% to 97% of ICU patients required mechanical ventilation, with median ventilator duration in survivors of 7 to 15 days; 5% to 22% required renal replacement therapy; and 28-day ICU mortality was 14% to 40%.45–51
Critical care capacity is a key element of hospital surge capacity planning.10 The proportion of ICU beds occupied by patients with H1N1 varied. In Australia and New Zealand, it peaked at 19%7 while in Mexico, many patients required mechanical ventilation outside the ICUs.6 To match the surge capacity with increasing ICU demands during a pandemic is a difficult task, since uncertainty exists for many of these parameters. The disease brought a surge of not only critically ill patients but patients who required prolonged mechanical ventilation and ICU management. Hospitals should maximize the number of ICU beds by expanding ICUs and other areas with appropriate beds and monitors. Elective procedures should be minimized when resources are limited, and critical care capacity should be augmented.
Safe practices and safe respiratory equipment are needed to minimize aerosol generation when caring for patients with influenza. These measures include handwashing and wearing gloves and gowns. The use of N95 respirators reduces the transmission of epidemic respiratory viruses. Staff training in personal protective equipment use is essential. Use of bag-mask ventilation and disconnection of the ventilator circuit should be minimized. Moreover, the use of heated humidifiers on ventilators, Venturi masks, and nebulized medications should be avoided.52
When the number of critically ill patients far exceeds a hospital’s traditional critical care capacity, modified standards of critical care to provide limited but high-yield critical care interventions should be the goal in order to accommodate far more patients. Triage criteria should be objective, transparent, and ethical and be applied justifiably and publicly disclosed. The ICU triage protocols for pandemics should only be triggered when ICU resources across a broad geographic area are or will be overwhelmed despite all reasonable efforts to extend resources or obtain additional resources.53 The Sequential Organ Failure Assessment (SOFA) score, though not validated, has been proposed to determine qualification for ICU admission during mass critical care.
The major characteristics of 2009 H1N1 influenza A infection were the rapidly progressive lower respiratory tract disease leading to acute respiratory distress syndrome (ARDS) with refractory hypoxemia. A substantial number of H1N1 ICU patients required advanced ventilatory support (ranging from 1.7% to 11.9%) and rescue therapies including high levels of inspired oxygen and positive end-expiratory pressure (PEEP), inverse ratio ventilation, airway pressure release ventilation (APRV), neuromuscular blockade, inhaled nitric oxide, high-frequency oscillatory ventilation (HFOV), extracorporeal membrane oxygenation (ECMO), volumetric diffusive respiration, and prone-positioning ventilation.46,49,51,54 Of particular interest was the successful use of ECMO in the management of refractory hypoxemia in these patients in two studies. The median durations of therapy and survival rates to ICU discharge were 10 days and 15 days—71% and 67%, respectively.55,56
As of March 13, 2010, the CDC estimates of 2009 H1N1 influenza cases, hospitalizations, and deaths in the United States since April 2009 were 60 million cases, 270,000 hospitalizations, and 12,270 H1N1-related deaths, respectively.57 The virus did not mutate during the pandemic to a more lethal form. Widespread resistance to oseltamivir did not develop. The WHO declared an end to the H1N1 pandemic on Aug 10, 2010. According to Margaret Chan, the Director-General of the WHO, the H1N1 virus is no longer the dominant circulating virus worldwide. Based on the available evidence and experience from past pandemics, “it is likely that the virus will continue to cause serious disease in the younger age group, at least in the immediate post-pandemic period. The H1N1 virus is expected to take on the behavior of a seasonal influenza virus and to circulate for some years.”
Other Natural Disasters
Tornadoes occur most commonly in the North American Midwest. Over 4115 deaths and 70,000 injuries have been ascribed to them during the years 1950 to 1994. They cause widespread destruction of community infrastructure. Injuries most commonly seen are complex contaminated soft-tissue injury (50%), fractures (30%), head injury (10%), and blunt trauma to the chest and abdomen (10%).58,59 Firestorms, wildfires, tsunamis, winter storms, and heat waves are other natural phenomena capable of creating mass injuries from thermal burns, airway injury, smoke inhalation, heat-related disorders, and hypothermia.60–63
 Manmade Disasters
Manmade Disasters
Transportation Disasters
Transportation accidents can produce injuries and death similar to those seen in major natural disasters. Some of the largest civilian disasters in North America have been related to transportation of hazardous materials.64 Motor vehicle accidents, railway accidents, airplane crashes, and shipwrecks are some of the common transportation accidents. They cause a wide range of injuries including multiple trauma, fractures, burns, chemical injuries, hypothermia, dehydration, asphyxiation, and CO inhalation. The hazard risk to a healthcare facility increases with its proximity to a chemical plant or highway, and such factors should be considered in the emergency preparedness plan of the hospital.65
Weapons of Mass Destruction
Weapons of mass destruction (WMD) are those nuclear, biological, chemical, incendiary, or conventional explosive agents that pose a potential threat to health, safety, food supply, property, or the environment. Since the devastating terrorist attacks in September 2001 and subsequent intentional release of anthrax spores in the United States, there is growing concern around the world about the possible threat of chemical, biological, or nuclear weapons used against a civilian population. Compared with the frequency of natural and technology-related disasters, the incidence of use of WMD to cause death and injury is relatively rare. However, biological and chemical weapons are relatively accessible, and WMD are thought to be available to most foreign states and terrorist groups. In response to a WMD incident, healthcare personnel will be called on to manage unprecedented numbers of casualties in an environment of panic, fear, and paranoia that accompanies terrorism. Because most attacks occur without warning, the local healthcare system will be the first and most critical interface for detection, notification, rapid diagnosis, and treatment. The best defense in reducing casualties will therefore rest on the ability of medical and public health personnel to recognize symptoms and provide rapid clinical and epidemiologic diagnosis of an event. This requires that healthcare providers be well informed of potential biological, chemical, and nuclear agents. They must have a heightened index of suspicion and be able to identify unusual disease patterns to determine whether WMD are the etiologic agents of illness. Physicians will need to practice appropriate surveillance and reporting and develop knowledge of mass decontamination, use of proper personal protection equipment, and safety protocols related to a biological, chemical, or radiologic event.66–68 Salient characteristics and brief management strategies of the different WMD are discussed here. Detailed description of individual biological and chemical agents, diagnosis, postexposure management, vaccination, infection control measures, and use of personal protection equipment is beyond the scope of this chapter.
Biological Weapons
Biological weapons can be either pathogens (disease-causing organisms such as viruses or bacteria) or toxins (poisons of biological origin). Compared with other WMD, biological weapons are characterized by ease of accessibility and dissemination, difficulty in detection because of their slow onset of action, and their ability to cause widespread panic through the fear of contagion. They can be spread through various means, including aerial bombs, aerosol sprays, explosives, and food or water contamination. Multiple factors including particle size of the agent, stability of the agent, wind speed, wind direction, and atmospheric conditions can alter the effectiveness of a delivery system. Based on the ease of dissemination, ability to cause high mortality, public panic and social disruption, and requirement for special action for public health preparedness, the Centers for Disease Control and Prevention (CDC) has classified biological weapons into three categories (Table 226-4).69 Category A agents are of particular concern because they can cause widespread disease through their ease of transmission, result in high mortality rates, cause panic and social disruption, and require special attention during public health preparedness. General features that should alert healthcare providers to the possibility of a bioterrorism-related outbreak include70:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree