Chapter 22 Mass casualty, chemical, biological and radiological hazard contingencies
AIMS AND OBJECTIVES
Incidents involving mass casualties are infrequent. However, they have the potential to overwhelm usual health resources with very little notice. It is therefore important that contingencies are developed, tested and ready for immediate implementation. Such contingencies outline the responsibilities for overall medical control, coordination and effective casualty management in major emergencies and disaster situations. They include the procedures for triage, first aid and resuscitation, some of which require modification when resource availability needs to be rationed.
PHASES OF A DISASTER
The phases of disaster management are prevention, preparedness, response and recovery.
Prevention
The prevention phase concentrates on strategies that minimise the severity of an incident. It aims to cushion the severity, reduce the effects, minimise adversity and contain the impact of a disaster. Prevention strategies also include incorporation of lessons learned from previous experiences.
ADMINISTRATIVE AND LEGISLATIVE MANDATES
Very broadly these legislative frameworks provide for:
MEDICAL RESPONSE PLANS AND AGENCIES
Components of a state medical response
Agencies or organisations responsible for health
The health department ensures coordination of:
The health department has direct responsibilities as the control agency for:
The ambulance service
Pre-hospital medical coordination/disaster scene
Area medical coordinator (AMC)/senior field emergency medical officer
Central medical coordinator (CMC)
The CMC is usually located in the ambulance communications centre. The CMC’s role is to:
Site medical control
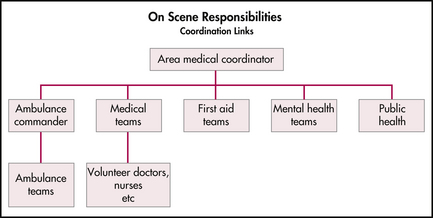
As an AMC or ambulance commander arrives on site, further assessments will be made and a joint medical command post established. All incoming medical responders report to the command post where tasks within the CCP are allocated. Further medical assistance required on site is requested through the central medical coordinator to avoid convergence and duplication of resources. A typical communication structure is outlined in Figure 22.1.
Life-saving procedures, such as airway management, immediate decompression of tension pneumothorax, arrest of haemorrhage, fracture stabilisation and relief of pain where necessary, may be the limit of medical assistance where medical resources are few. Thus effective triage or classification of casualties by a casualty collecting (ambulance) officer (CCO), medical officer or team leader from a medical team is essential.
Triage and reverse triage
Sieve
This triage method is used during the initial phase of managing mass casualties. It focuses on determining which patients will survive and channels resources to initially moving that cohort of patients from the scene to a casualty clearing post or station. Triaging in this manner is a repeated process to ensure refinement of urgency stratification and to respond appropriately to the ongoing evolution of a casualty’s injury complex and consequent physiology.
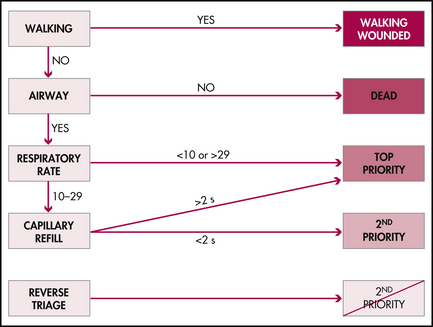
A standard clinical reasoning scheme for triage is outlined in Figure 22.3. SIEVE triage categories are as follows:
Table 22.1 Triage groupings and criteria for mass casualty situations
| Group | Priority | Criteria |
|---|---|---|
| 1 | Red—priority 1 | |
| 2 | Yellow—priority 2 | |
| 3 | Green—minor injuries | |
| 4 | Black—deceased |
SORT
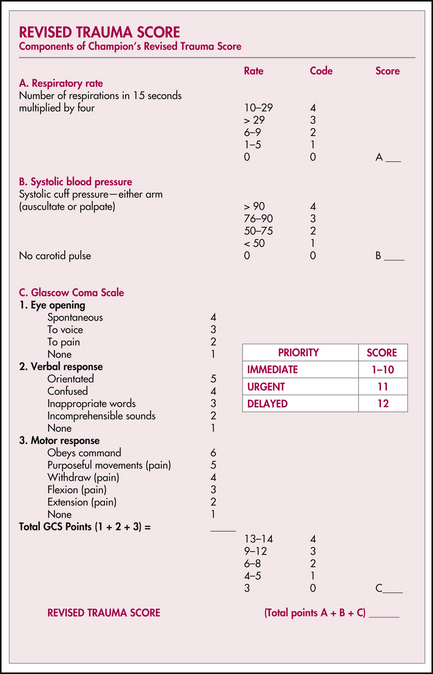
This method of triage is based on the Revised Trauma Score and is consistent with the Australasian Triage Scale, triage practices taught in emergency management of severe trauma (EMST), emergency life support (ELS), advanced paediatric life support (APLS) and major incident medical management and support (MIMMS) courses. It is identical to the practices employed by ambulance, first responder and other emergency medical services personnel for determining the time-critical patient. It is a repeated process that is dependent upon traditional ongoing patient observation.
SORT is generally implemented in the field utilising the Revised Trauma Score in order to rank physiological embarrassment and allocating an ordinal score. This assists with re-prioritisation or risk stratification of casualties. Scores of 1–10 are associated with the immediate category. A score of 11 identifies an urgent patient. A score of 12 or higher identifies casualties that can wait for delayed management (Figure 22.4).
Further refinement of triage can be assisted by attention to pattern of injuries or mechanism of injuries. However, in a trauma related mass casualty incident, a considerable number of patients may be classified as time-critical on mechanism of injury alone (Table 22.2
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree