Figure 12.1 Anatomy of the scrotum with blood supply. (a) Diagram of the normal scrotal anatomy showing tunica albuginea surrounding the testis and the extratesticular epididymis. Illustration by Laura Berg, MD. (b) Testicular blood supply. Artwork created by Emily Evans © Cambridge University Press
Additional structures in the scrotum should be recognized. The epididymis is an extratesticular curved structure, that measures 6–7 cm in length and lies posterolateral to the testis. The tail of the epididymis turns into the vas deferens as it moves superiorly out of the scrotum. The spermatic cord consists of the vas deferens, the arteries supplying the testes, a plexus of veins, the lymphatics, and the nerves of the testes. The normal spermatic cord lies just beneath the skin and is difficult to distinguish from the adjacent soft tissues of the inguinal canal on examination or with ultrasound. Finally, the appendix testis is a small ovoid structure located most commonly on the superior pole of the testis or in the groove between the testis and the head of the epididymis.
The blood supply of the testis is important to understand, in order to accurately interpret ultrasound with Doppler (Figure 12.1b). The supply of blood comes from the testicular, deferential, and cremasteric arteries. The majority of the blood flow to the testis is supplied by the testicular artery, which enters the spermatic cord at the deep inguinal ring and continues along the posterior surface of the testis. A transmediastinal arterial branch of the testicular artery is present in approximately one-half of normal testes; it courses through the mediastinum to supply the periphery of the gland. The deferential and cremasteric arteries primarily supply the epididymis and extratesticular tissues of the structures of the scrotum, but they also supply a small portion of the arterial supply to the testicle through anastomoses with the testicular artery. Venous drainage of the testes is via the pampiniform plexus of draining veins, formed around the upper half of the epididymis, and continues as the testicular vein through the deep inguinal ring. The right testicular vein empties into the IVC, while the left testicular vein empties into the renal vein.
Technique
Point-of-care questions
Transducer selection and orientation
Optimal results are obtained using a linear, high-frequency (5–10 MHz) transducer with the capabilities of performing power, color, and pulsed-wave Doppler ultrasonography. If greater penetration is needed because of scrotal swelling, a lower-frequency transducer may be helpful. Power Doppler is helpful in scrotal ultrasound as, unlike color Doppler, it is insensitive to direction of flow, and more likely to register low-pressure blood flow, as that found in testicles.
The scan is begun in the longitudinal axis to the testicle, with the indicator oriented towards the patient’s head. This will reveal the epididymis on the left side of the ultrasound screen (Figure 12.2a.) The testicle is then scanned through in its entirety, paying careful attention to any changes in the normally homogeneous organ. The scan is then repeated with the transducer turned 90° towards the patient’s right, giving a short-axis view of the testicle (Figure 12.3a).

Figure 12.2 Scrotal imaging, sagittal view. (a) Transducer placement for the sagittal view with indicator towards the patient’s head. (b) Normal right testis in the sagittal view. Note the homogeneity of the testicular tissue.
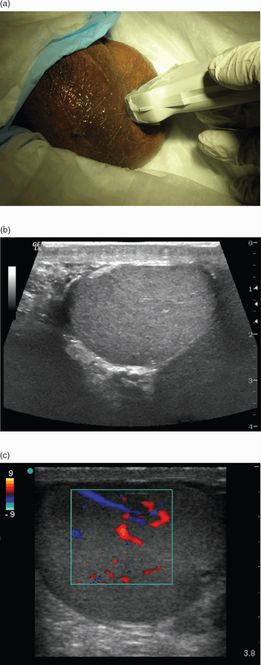
Figure 12.3 Scrotal imaging, transverse view. (a) Transducer placement for the transverse view, with the indicator towards the patient’s right side. (b) Normal testis in the transverse view. (c) Color Doppler flow to the testis in the transverse view.
Patient position and preparation
Scrotal ultrasound is performed with the patient in the supine position, traditionally with the scrotum supported by a towel placed between the thighs. If a young child is anxious or difficult to control, having a parent hold him may be advantageous.
Ultrasound imaging
Scrotal ultrasound is highly dependent on the skill of the operator. The detection of blood flow, which is integral in the assessment of testicular torsion, depends on the patient’s age, testicular volume, and the sensitivity of the equipment and type of Doppler used. Scanning is performed with the transducer in direct contact with the skin. The testes are examined in at least two planes, along the longitudinal (Figure 12.2b) and transverse (Figure 12.3b) axes. It is important to scan through the entire testicle so that any small areas of pathology are not missed. It is preferable to scan the unaffected scrotum first. Not only does this provide an important comparison of anatomy and blood flow, but also it helps to ease any patient anxiety regarding the ultrasound. When scanning the asymptomatic side first, the operator should set the grayscale and Doppler gain settings, in order to allow the highest sensitivity to detect blood flow with the least amount of artifact (Figure 12.3c). It is also helpful to obtain one image that contains both testicles side by side in the transverse or short-axis, also referred to as the “buddy” view (Figure 12.4). This allows for a more direct comparison of the size and echogenicity between the two testes and epididymis. The structures within the scrotal sac are also examined to detect extratesticular masses or other abnormalities. In patients presenting with palpable masses or nodules, the scan should include the region of concern. A finger may be placed beneath the nodule and the transducer placed directly over the nodule for scanning.
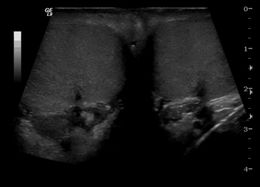
Figure 12.4 Scrotal imaging, “buddy” view. Transverse view showing both testes side-by-side in a single image, allowing for direct comparison.
The normal testis on ultrasound has a homogeneous appearance, and is composed of uniformly distributed medium-level echoes (Figure 12.2b, 12.3b). Its echogenicity is often compared with that of the liver or the thyroid gland. However, prepubertal testes typically have lower echogenicity than that of adults. The mediastinum testis is sometimes seen as a linear echogenic band extending through the center of the testicle in a caudo-cranial direction (Figure 12.5a). The epididymis is normally isoechoic or slightly hyperechoic to the testis. The epididymal head can often be distinguished from the rest of the testis as it often appears slightly brighter and is located atop the superior pole of the testis. The body of the epididymis is usually isoechoic and indistinguishable from the surrounding tissue (Figure 12.5b,c). The appendix testis is normally hidden by the epididymal head and often not seen by ultrasound, unless surrounded by anechoic fluid in such cases as a hydrocele (Figure 12.5d). The layers covering the scrotum are normally indistinguishable by ultrasonography, and are seen as a single echogenic stripe. In some cases of testicular torsion, a rotated spermatic cord may be visualized.
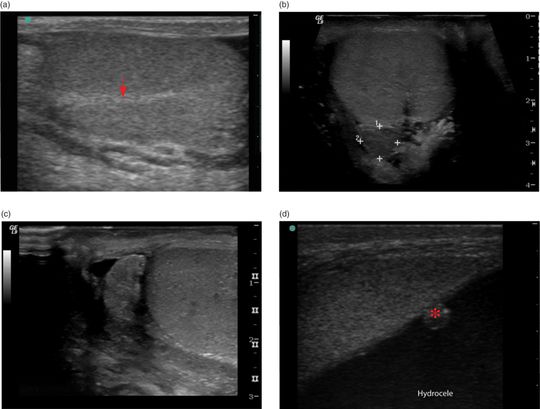
Figure 12.5 Normal structures within the scrotum. (a) The hyperechoic line extending horizontally is the mediastinum testis (arrow). (b) A view of a normal testicle showing the epididymis body and tail (calipers), in the transverse view. (c) The epididymis in sagittal orientation. (d) A normal appendix testis (*), seen in the presence of a hydrocele.
Ultrasound imaging: Doppler
An integral part of scrotal ultrasound is the use of power and spectral Doppler. Testicular perfusion can be evaluated with power, color, or pulsed-wave Doppler and is easily detected in both normal and pathologic testes. One of the most challenging aspects of scrotal ultrasound is confirming both arterial and venous blood flow. The failure to confirm the presence of both arterial and venous blood flow can lead to false-negative ultrasound examinations, when assessing for testicular torsion (Figure 12.6a,b). It is also important to recognize that flow is much more difficult to detect in prepubertal children and infants. Prepubertal boys have smaller testicular vessels and lower blood-flow velocities. The use of higher-frequency transducers and more careful examination may be necessary to detect blood flow. In the pediatric patient, it may be difficult to detect blood flow even in the normal testis.
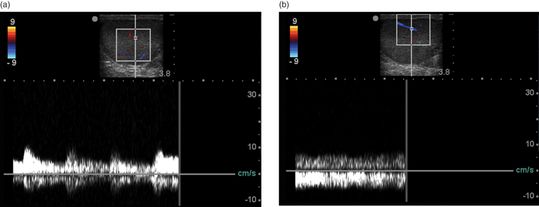
Figure 12.6 Doppler with arterial and venous waveforms. (a) Spectral Doppler showing the arterial waveform, which is more pulsatile than the (b) venous waveform, showing low continuous flow.
The evaluation of blood flow is a key aspect in the diagnosis of testicular torsion, as well as in diagnosing epididymitis, and orchitis. Higher power gains are more likely attained with power Doppler, yielding a higher sensitivity in detecting blood flow than with color Doppler (Figure 12.7). While power Doppler is helpful in detecting blood flow and comparing the two testes, spectral or pulsed-wave Doppler is becoming the modality of choice. Pulsed-wave Doppler is able to distinguish between venous and arterial flow, which is essential in assessing for testicular torsion. The assessment of blood flow, in general, must be interpreted with caution. In situations of ongoing torsion and detorsion or with spontaneous detorsion, as the testicle regains its blood supply an increased blood flow may be seen and interpreted as a false-negative finding for testicular torsion. This increased blood flow must be differentiated from the hyperemia seen in inflammatory and infectious etiologies. In these cases, serial clinical and ultrasound examinations are essential, and the patient should still be evaluated for potential surgical management.
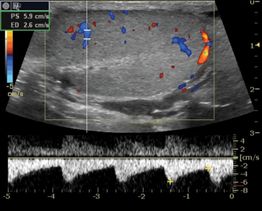
Figure 12.7 Doppler scanning of a normal testis. Sagittal view of a homogeneous right testicle showing both color and pulsed wave Doppler.
Scanning tips
Pitfalls
- Hyperemia may be seen with spontaneous detorsion and even in a necrotic testis. This may be mistaken for the hyperemia seen with epididymitis.
- There are reports of false-negative studies for torsion in cases of decreased blood flow in both testes, and in cases of incomplete or intermittent torsion where there is preserved blood flow.
- Failure to confirm the presence of both arterial and venous blood flow can lead to false-negative ultrasound examinations when assessing for testicular torsion in the patient presenting with a painful scrotum.
- Relying solely on a point-of-care ultrasound to rule in or rule out testicular torsion: the majority of portable ultrasound machines do not have high enough power to adequately assess for venous and arterial blood flow.
Tips to improve scanning
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








