and elastase. This inflammatory response plays a key role in the development of acute respiratory distress syndrome (ARDS) and MODS. The metabolic response to severe trauma is biphasic. SIRS occurs during the initial 3–5 days; during this phase, a second insult (or hit), such as surgery, may provoke an exaggerated inflammatory response. Up to 50% of the patients developing organ failure early after trauma do so in the absence of bacterial infection. The initial phase is followed by a period (perhaps 10–14 days) of immunosuppression, when the patient is prone to infection. Multiple organ failure can occur during either of these phases.
Assessment and management of the trauma patient
Prehospital phase
In the UK, prehospital management of severely injured patients is performed mainly by paramedics, although doctors are increased involved, particularly with helicopter emergency medical services (HEMS). Paramedics are trained to minimise on-scene time; a prolonged time to definitive care will increase mortality. Unless the patient is trapped, on-scene interventions should be restricted to control of the airway and ventilation, and stabilisation of the spine. The prehospital presence of a doctor will enable rapid sequence induction (RSI) and intubation to be undertaken in patients with severe traumatic brain injury (TBI) and others in whom control of the airway and ventilation is considered important before transfer to hospital. The receiving hospital should be given advanced warning of the impending admission of a severely injured patient. Ambulance personnel should be able to communicate directly with emergency department staff via a talk-through link. Concise and essential information on the patient’s condition and estimated time of arrival must be given. Emergency department staff can then decide whether to alert the trauma team.
Trauma networks
There is evidence from the United States that severely injured patients who are treated in specialised trauma centres have better outcomes than those treated in smaller hospitals that treat relatively few such patients. In the UK, trauma networks were implemented widely in 2012 and severely injured patients are transferred directly to a major trauma centre (MTC) unless they have immediately life-threatening injuries that require initial stabilisation at the nearest trauma unit (usually a district general hospital) before secondary transfer to the MTC.
Preparation for resuscitation
With advance warning, medical and nursing staff can prepare a resuscitation bay in readiness for the patient’s arrival. This will include running through drip sets, turning on fluid warmers, and drawing up anaesthetic drugs. Members of the resuscitation team put on protective clothing comprising gloves, plastic aprons and eye protection. The relevant nurses and doctors are assigned tasks before the patient arrives. In hospitals with formal trauma teams, the roles of individual team members are usually well established (Figure 9.3). The team leader should be a suitably experienced doctor from one of the relevant specialties, e.g. emergency medicine, anaesthesia, general surgery or orthopaedic surgery.
| Team leader | Primary and secondary surveys, coordination of team, overall responsibility for the patient while in the emergency department |
| Doctor 1 & Nurse 1 | Airway, ventilation, central venous access, difficult peripheral access, fluid balance, analgesia |
| Doctor 2 & Nurse 2 | All other procedures, chest drain, fracture splintage, urethral catheter |
| Nurse 3 | Measure vital signs, record data, remove clothes, assist other team members |
| Radiographer | Chest and pelvis x-rays; other x-rays as requested by team leader |
| Porter | To take samples to pathology labs, to retrieve urgent blood from blood bank |
Primary survey and resuscitation
The initial management of the trauma patient is considered in four phases:
Primary survey
Resuscitation
Secondary survey
Definitive care
Although the first two phases are listed consecutively, they are performed simultaneously. The secondary survey, or head-to-toe examination of the patient, is not started until the patient has been adequately resuscitated. The aim of the primary survey is to look sequentially for immediately life-threatening injuries, in the order that they are most likely to kill the patient. The correct sequence is:
A. Airway with cervical spine control
B. Breathing
C. Circulation and haemorrhage control
D. Disability – a rapid assessment of neurological function
E. Exposure – while considering the environment, and preventing hypothermia
If life-threatening problems are detected, treat them immediately (resuscitate) before proceeding to the next step of the primary survey. In the presence of exsanguinating external haemorrhage it may be more appropriate to apply a CABC sequence, in which external bleeding is first controlled with external pressure or, if a limb is involved, by the application of a tourniquet. Use of the CABC sequence is particularly common in military settings.
Airway and cervical spine
Unless there is catastrophic external haemorrhage (when CABC applies), the first priority during the resuscitation of any severely injured patient is to ensure a clear airway and maintain adequate oxygenation (Crewdson & Nolan 2011). Place a pulse oximeter probe on the patient’s finger. Knowing the patient’s arterial blood oxygen saturation is very valuable, although sometimes peripheral vasoconstriction will make it impossible to obtain a reliable reading. If the airway is obstructed, immediate basic manoeuvres such as suction, chin lift and jaw thrust may clear it temporarily. A soft nasopharyngeal airway (size 6.0–7.0 mm) may be particularly useful in the semiconscious patient who will not tolerate an oropharyngeal airway. Give high-concentration oxygen to every patient with multiple injuries. In the unintubated, spontaneously breathing patient this is provided with a mask and reservoir bag (FIO2 = 0.85).
Care of the cervical spine
Every patient sustaining significant blunt trauma, particularly above the clavicles, should be assumed to have a cervical spine injury until proven otherwise. Such patients should have their cervical spines immobilised at the accident scene. The most effective method comprises a combination of an appropriately sized semi-rigid cervical collar, lateral supports and straps (Figure 9.4). Undertake all airway manoeuvres carefully without moving the neck. Significant subluxation of the cervical spine can occur during aggressive chin lift or jaw thrust despite the presence of an appropriate collar. Mask ventilation can displace the cervical spine as much as oral intubation. Manual in-line stabilisation of the neck will minimise movement of the cervical spine during oral intubation, but avoid excessive traction, which may distract a cervical fracture. In the resuscitation room, the cervical spine cannot be deemed undamaged until the patient has been examined by an experienced clinician and/or appropriate radiological procedures have been completed. A reliable clinical examination cannot be obtained if the patient has sustained a significant closed head injury, is intoxicated, or has a reduced conscious level from any other cause.
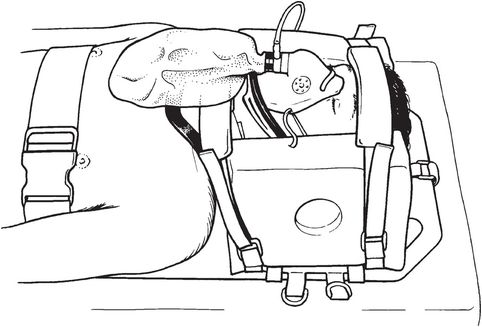
Cervical spine immobilisation with semi-rigid collar, lateral blocks and spine board
Advanced airway management
In the unconscious patient, or in the presence of haemorrhage from maxillofacial injuries, for example, the airway must be secured by placing a cuffed tube in the trachea. Other reasons for intubating the trauma patient during the resuscitation phase are to optimise oxygen delivery and to enable appropriate procedures to be performed on uncooperative patients. The choice of technique for intubating a patient with a suspected or confirmed cervical spine injury will depend on the indication and on the skill and experience of the individual clinician. If performed with care, tracheal intubation of a patient with a cervical spine injury carries relatively little risk (Crosby 2006). Occasionally, awake fibreoptic intubation may be appropriate, but this will take much longer to achieve and is rarely applicable in the resuscitation phase. Do not attempt blind nasal intubation.
The technique of choice for emergency intubation of a patient with a potential cervical spine injury is direct laryngoscopy and oral intubation with manual in-line stabilisation (MILS) of the cervical spine, following a period of preoxygenation, intravenous induction of anaesthesia, paralysis with suxamethonium and application of cricoid pressure. Manual in-line stabilisation reduces neck movement during intubation, but excessive axial traction must be avoided. An assistant kneels at the head of the patient and to one side to leave room for the intubator. The assistant holds the patient’s head firmly down on the trolley by grasping the mastoid processes. The tape or straps, lateral blocks and front of the collar are removed. The front of a single-piece collar can be folded under the patient’s shoulder, leaving the posterior portion of the collar in situ behind the head. Do not attempt laryngoscopy and intubation with the collar in place – it will make it very difficult to get an adequate view of the larynx. Placing the patient’s head and neck in neutral alignment will make the view at laryngoscopy worse: in this position the view of the larynx will be grade 3 or worse in approximately 20% of patients. Intubation will be aided greatly by the use of a gum-elastic bougie – it enables less force to be applied to the laryngoscope because intubation can be achieved despite a relatively poor view. The McCoy levering laryngoscope may also be useful: it reduces the incidence of grade 3 or worse views to 5%. A variety of videolaryngoscopes are now available, and use of these devices in the trauma setting is likely to become the standard of care.
If intubation of the patient proves impossible the airway should be secured by surgical cricothyroidotomy. A supraglottic airway device (SAD) may provide a temporary airway, but does not guarantee protection against aspiration (Timmermann 2011). A second-generation SAD, such as the ProSeal LMA, is probably better under these circumstances. The laryngeal tube and iGel are reasonable alternatives.
Needle cricothyroidotomy and jet insufflation of oxygen from a high-pressure source (400 kPa) is an alternative method of providing temporary oxygenation, but it seemed less successful than surgical cricothyroidotomy in the Fourth National Audit Project (NAP4) study (Cook et al. 2011). Standard cannulae may kink and become obstructed, so use a device manufactured specifically for needle cricothyroidotomy.
Breathing
Look and listen to the chest to confirm that both sides are being ventilated adequately, and measure the respiratory rate. The following chest injuries are immediately life-threatening and must be diagnosed and treated in the primary survey:
Tension pneumothorax
Open pneumothorax
Flail chest
Massive haemothorax
Cardiac tamponade
Tension pneumothorax
Reduced chest movement, reduced breath sounds and a resonant percussion note on the affected side, along with respiratory distress, hypotension and tachycardia, indicate a tension pneumothorax. Deviation of the trachea to the opposite side is a late sign, and neck veins may not be distended in the presence of hypovolaemia. Treatment is immediate decompression with either a large cannula placed in the 2nd intercostal space, in the mid-clavicular line on the affected side, or a rapid thoracostomy (small incision into the pleural space) in the 5th intercostal space in the anterior axillary line. Once intravenous access has been obtained, insert a large chest drain (32 F) in the 5th intercostal space in the anterior axillary line, and connect to an underwater seal drain.
Open pneumothorax
Cover an open pneumothorax with an occlusive dressing and seal on three sides: the unsealed side should act as a flutter valve. Insert a chest drain away from the wound in the same hemithorax.
Flail chest
Multiple fractures in adjacent ribs will cause a segment of the chest wall to lose bony continuity with the thoracic cage. This flail segment will move paradoxically with inspiration. The immediately life-threatening problem is the underlying lung contusion, which can cause severe hypoxia. The patient must be given effective analgesia – in the cardiovascularly stable patient a thoracic epidural is ideal (see below). Assisted ventilation, via a tracheal tube or by a non-invasive technique, is required if hypoxia persists despite supplemental oxygen.
Massive haemothorax
A massive haemothorax is defined as more than 1500 mL blood in a hemithorax, and it will cause reduced chest movement, a dull percussion note and hypoxaemia. Start fluid resuscitation and insert a chest drain. The patient is likely to require a thoracotomy if blood loss from the chest drain exceeds 200 mL per hour, but this decision will depend also on the patient’s general physiological state.
Cardiac tamponade
While not a disorder of breathing, it is logical to consider the possibility of cardiac tamponade while examining the chest, particularly if the patient has sustained a penetrating injury to the chest or upper abdomen. Distended neck veins in the presence of hypotension are suggestive of cardiac tamponade although, after rapid volume resuscitation, myocardial contusion will also present in this way. Ultrasound examination in the resuscitation room is the best way to make the diagnosis, and now that focused assessment with sonography for trauma (FAST) scanning is included in the emergency medicine curriculum there is usually someone immediately available to undertake this examination. If cardiac tamponade is diagnosed and the patient is deteriorating, a resuscitative thoracotomy and pericardiotomy is indicated. Needle pericardiocentesis is often unsuccessful because, contrary to traditional teaching, the pericardial blood is often clotted or re-accumulates rapidly once aspirated.
Chest drainage
Indications for chest drainage in the trauma patient are a tension pneumothorax (after decompression), simple pneumothorax, haemothorax, and multiple rib fractures in a patient requiring positive-pressure ventilation. Do not use a trochar for chest drain insertion: it can cause serious lacerations of the lung and pulmonary vessels. The practical technique is given in Figure 9.5. It is reasonable to observe carefully (but not insert a chest drain initially) in cases where there is a small pneumothorax that is seen on CT scan but not a chest x-ray (‘occult pneumothorax’) or when positive-pressure ventilation is used in the presence of relatively undisplaced rib fractures. In both these cases, ensure that there is immediate access to the chest in case a chest drain is required.
|
Circulation
Control any major external haemorrhage with direct pressure. Severe haemorrhage from open limb injuries may be controlled with a properly applied tourniquet. In the past, use of tourniquets in this way was discouraged, but recent military experience with blast injuries, in particular, has shown them to be very effective. Rapidly assess the patient’s haemodynamic state and attach ECG leads. Until proven otherwise, hypotension should be assumed to be caused by hypovolaemia. Less likely causes include myocardial contusion, cardiac tamponade, tension pneumothorax, neurogenic shock and sepsis.
Intravenous access
Insert two short large-bore intravenous cannulae (14 gauge or larger) into a peripheral vein. Most anaesthetists are confident in inserting central lines but this may not be easy in the hypovolaemic patient and there is a risk of creating a pneumothorax. The femoral vein provides a good route for a large-bore cannula. In the severely injured patient, central venous access is valuable because it enables delivery of multiple drug infusions as well as central venous pressure (CVP) monitoring. The intraosseous (IO) route (usually via the proximal tibia) is useful and modern devices enable infusion of fluids at up to 200 mL min–1, which makes this route useful for fluid resuscitation of adults as well as children. Insert an arterial cannula for continuous direct blood pressure monitoring and send a sample for arterial blood gas analysis – severely injured patients will have a marked base deficit, and its correction will help to confirm adequate resuscitation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







