CHAPTER 8 Lumbar Stabilization Exercise
Description
Terminology and Subtypes
Exercise, loosely translated from Greek, means “freed movement” and describes a wide range of physical activities. Therapeutic exercise indicates that the purpose of the exercise is for the treatment of a specific medical condition rather than recreation. The main types of therapeutic exercise for low back pain (LBP) include (1) general physical activity (e.g., advice to remain active); (2) aerobic (e.g., brisk walking, cycling); (3) aquatic (e.g., swimming, exercise classes in a pool); (4) directional preference (e.g., McKenzie); (5) flexibility (e.g., stretching, yoga, Pilates); (6) proprioceptive/coordination (e.g., wobble board, stability ball); (7) stabilization (e.g., targeting abdominal and trunk muscles); and (8) strengthening (e.g., lifting weights).1 This chapter focuses exclusively on stabilization exercises for chronic LBP (CLBP).
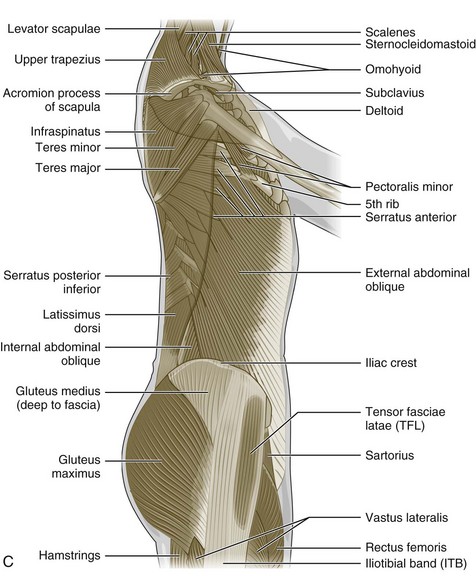
Therapeutic exercise for individuals with LBP has evolved over time. Recently, there has been a focus on exercises that aim to maintain stability in the lumbar spine.2 This type of exercise approach has been termed lumbar stabilization, core stabilization, or segmental stabilization. Although no formal definition of lumbar stabilization exercise (LSE) exists, this approach is generally aimed at improving the neuromuscular control, strength, and endurance of muscles central to maintaining dynamic and static spinal and trunk stability. Several groups of muscles are targeted through LSEs, particularly the transversus abdominis (TrA), lumbar multifidus, and other paraspinal, abdominal, diaphragmatic, and pelvic musculature (Figure 8-1).
History and Frequency of Use
In the 1980s, Bergmark undertook a mechanical engineering approach to the study of the lumbar spine.3 His goal was to assess the role of the trunk musculature in providing stabilization for the lumbar spine and measure the specific forces applied to the spine by different muscles to understand the biomechanical “rationale” for the complex anatomic features of the lumbar spine. Using a mechanical modeling approach, musculature acting on the lumbar spine was divided into two groups: local and global. The global musculature (e.g., erector spinae, rectus abdominis) was thought to transfer load between the thoracic spine and pelvis. The local musculature (e.g., multifidus) consists of muscles that act directly on the lumbar spine and are attached to the lumbar vertebrae. Functionally, the global musculature was thought to balance the outer loads on the body, enabling the local system to maintain force control within the lumbar spine and center postural activity at a range within the load tolerance of the spinal structures.
Panjabi then proposed a basis for understanding spinal stability, injury, dysfunction, and recovery by asserting that there are three interdependent subsystems that function to stabilize the spine: passive, active, and neural.4 The passive subsystem includes the vertebrae, intervertebral discs, ligaments, zygapophyseal joints, and passive components of the associated musculotendinous structures. The active subsystem comprises the musculotendinous units attached to, or influencing, the spinal column.4 The neural subsystem includes sensory receptors in the spinal structures, their central connections, and cortical and subcortical control centers. These three subsystems are interdependent and work together to maintain spinal stability and intervertebral motion. For example, an injury or breakdown in the passive subsystem, such as a fracture, disc herniation, or disc degeneration, may decrease the inherent stability of the spine and alter segmental motion patterns. Enhancement of the neural and active subsystems could potentially help compensate for this loss and partially restore stability.
A number of authors have assessed the role and activation patterns of trunk musculature as they relate to spinal stability. Cresswell and colleagues5–7 conducted a series of studies on intra-abdominal pressure and activation of trunk musculature. They reported that intra-abdominal pressure was increased during functional tasks by muscles that did not create a significant flexion movement of the lumbar spine (particularly the TrA and diaphragm), and activation of the TrA was correlated with changes in intra-abdominal pressure. It was also discovered that abdominal wall muscles were activated before the erector spinae if ventral loading of the trunk was expected, and concurrently with the erector spinae in unexpected ventral loading. This finding suggested that abdominal musculature may play a role in enhancing spinal stability during trunk motion or loading.
Hodges and Richardson8 further pursued this line of research by studying activation patterns of trunk musculature with alteration of spinal posture by movement of an upper limb. In those without LBP, the TrA was the first muscle activated, contracting before upper limb movement regardless of direction of motion. This suggested that the TrA provides stability for the lumbar spine in anticipation of perturbations of posture. In individuals with LBP, however, the contraction of the TrA was significantly delayed, indicating a potential for decreased spinal stability and fundamental problems with motor control. Similar findings were noted in later studies on the effects of lower extremity motion in those with and without LBP.9,10
There have also been several studies on the lumbar multifidi in those with LBP. In 1994, Hides and colleagues11 reported finding significant ipsilateral atrophy in the lumbar multifidi of individuals with unilateral LBP, whereas they noted very little asymmetry in these muscles in a control group of subjects without LBP. Patients with acute, first-episode LBP who were treated with usual medical management had limited recovery of multifidus muscle mass after 10 weeks, whereas those treated with a specific exercise program had greater recovery of multifidus muscle mass.12 On the basis of these conceptual models, Richardson and Jull2 described a specific exercise program to train co-contraction of the deep trunk muscles, particularly the TrA and lumbar multifidi, to enhance spinal stability in individuals with LBP. This treatment program has been the basis for a large number of further clinical studies and other publications and for what is commonly used in “core stability” programs.12–25
Other authors, and particularly Stuart McGill, have addressed additional aspects of stabilization training to emphasize broader and more integrative approaches and effects.21,26,27 Early studies on the effects of these exercise programs indicated that they may have substantial benefit in the treatment of individuals with first-time acute LBP or with specific structural abnormalities in the spine.13,16 In clinical practice, these programs are applied to a wide range of patients with LBP, although the popularity of these treatment programs is difficult to quantify. The number of recent studies conducted on this topic, along with the publication of a recent systematic review (SR) of stabilization exercises on LBP, suggest that these programs are increasingly popular.26,28–31
Procedure
The exercise program of Richardson and Jull2 addressing the TrA and multifidi is described in detail in their text, and formal training in this program is generally administered by a physical therapist. The initial aim of this program is to achieve isometric co-contraction of the local muscles of the trunk, with activation of the TrA and multifidi being considered the “basic functional unit of a movement skill.”2 Patients are instructed to draw in the lower abdominal wall while simultaneously contracting the multifidi isometrically. A number of techniques were proposed to facilitate the learning of this particular motor skill, including visual correction, specific verbal instructions, manual facilitation, and use of a pressure biofeedback unit; specific postures are also advocated to assist in motor learning. A strong emphasis is placed on the accurate performance of the maneuvers, and the patients are progressed into functional positions while maintaining muscle activation. Exercises can be advanced when the patient is able to maintain 10 isometric “holds” for 10 seconds without fatiguing. In their study using this training protocol, O’Sullivan and colleagues13 noted that, for some subjects, it took 4 to 5 weeks of training just to obtain an accurate pattern of isometric co-contraction of these muscles. This program has been modified by other investigators, and many have described progression through functional programs that incorporate previously painful motion patterns. A variety of exercises have been developed over the years to promote trunk stabilization (e.g., Figures 8-2 and 8-3), some of which can be performed with exercise equipment such as Swiss balls (e.g., Figures 8-4 and 8-5).
Additional methods of facilitation, including the use of ultrasound, educational pamphlets, and video demonstrations, have also been applied.23–25 Reflecting the nonstandardized and generally multifactorial nature of many physical therapy treatments, studies have varied in their use of cointerventions such as manual therapy techniques, general conditioning, and varying degrees of physical and cognitive behavioral therapy. Settings also varied among studies that used either group classes or individual treatment approaches. It is difficult to describe a “typical” treatment course, but 6 to 12 sessions of LSE instruction are relatively common for a straightforward clinical scenario. However, many patients have a number of mitigating conditions that may affect the frequency and duration of care required.
Theory
Mechanism of Action
Lumbar Stability
Lumbar stabilization exercises provide an opportunity to simultaneously exercise the passive, active, and neural subsystems of spinal stabilization proposed by Panjabi.4 It has been suggested that injury to the vertebrae, intervertebral discs, ligaments, or zygapophyseal joints that comprise the passive subsystem could perhaps be compensated by enhancing the neural and active subsystems, thereby restoring lumbar stability. Lumbar stabilization exercise may also improve abdominal muscle strength and endurance, thereby compensating for decreased stability due to lumbar musculature injury. Improving function of abdominal muscles such as the TrA through LSE involving limb movements could also prevent spinal instability by compensating for injured lumbar muscles.9,10 Lumbar stabilization exercise emphasizing co-contraction of the TrA and lumbar multifidi could also enhance spinal stability in individuals with LBP, thereby reducing their risk for reinjury.2 When combined with dynamic and isometric intensive resistance training, LSE was associated with increased cross-sectional lumbar musculature.32 Because these changes were not noted with LSE alone, they may be attributable to the progressive resistance exercises, or possibly an interaction effect of lumbar stabilization and strengthening.
Indication
The use of LSEs has been recommended for nonspecific mechanical CLBP with or without specific anatomic abnormalities such as spondylolisthesis. Isometric exercise of the trunk musculature may be an appropriate consideration for any LBP beyond the acute stage. By extrapolating from Panjabi’s model of spinal instability and the work of many of the authors previously discussed, there may be a rationale for using LSE in almost any patient with CLBP, including those with ongoing pain and a clearly definable structural source or those without correlative pathology identified on standard imaging.4 This intervention may be most effectively applied in a patient who presents with a reproducible, mechanical pattern of lumbopelvic pain that follows a specific plane of movement or functional task. Often these patients demonstrate altered activation patterns of stabilizing musculature or poor endurance of core stabilizing musculature with testing.
Assessment
Before receiving LSE training, patients should first be assessed for LBP using an evidence-based and goal-oriented approach focused on the patient history and neurologic examination, as discussed in Chapter 3. Additional diagnostic imaging or specific diagnostic testing is generally not required before initiating this intervention for CLBP. Nevertheless, several diagnostic tests are used clinically to apply the proper and safe dose of exercise, monitor progress throughout treatment, and document that the target muscles are being appropriately activated. These include a functional assessment of strength, flexibility, balance, endurance, and coordination, and potential assessment of lumbar muscle activity through real-time ultrasound and surface electromyography to allow a more precise prescription for LSE training.12,33–35
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree