7 Lower Extremities !++ R1–2 times a week, up to 12 weeks Orhtotech, ThE, MET, MM, Acu ! +++ R 3 times a week, up to 6 weeks PhysApps, FMA, ThE, MET !++ R 2 times a week, up to 4 weeks MM, FMA, PhysApps, Acu ! +++ R 2 times a week, up to 8 weeks MM, ThE, MET, Orthotech, PhysApps – achillodynia – knee flexion contracture – contracted drop foot – calf cramps at night !++ R 3 times a week, up to 6 weeks ThE, MA, MM, Orthotech, PhysApps – genua vara (bow legs) – dysfunction of the upper and lower ankle joints – partial weakness after disk herniation at L4/L5
 Complex Pain
Complex Pain
Patellofemoral Pain Syndrome (Runner’s Knee)
Indications
 Irritation of the patellar ligament and the distal area of musculus quadriceps femoris
Irritation of the patellar ligament and the distal area of musculus quadriceps femoris
 Patellar chondropathy and arthrosis of the knee joint
Patellar chondropathy and arthrosis of the knee joint
 Pes anserinus tendinosis
Pes anserinus tendinosis
 Patellar tendinitis (jumper’s knee)
Patellar tendinitis (jumper’s knee)
 Irritation of the infrapatellar nerve
Irritation of the infrapatellar nerve
Differential Diagnoses
 Inflammation of the knee joint (gonarthritis)
Inflammation of the knee joint (gonarthritis)
 Referred pain in disorders of the rectus femoris
Referred pain in disorders of the rectus femoris
 Referred pain in shortening of the vastus lateralis
Referred pain in shortening of the vastus lateralis
 Radiating pain in inflammatory changes of the sural nerve and radicular symptoms in the L 4 segment
Radiating pain in inflammatory changes of the sural nerve and radicular symptoms in the L 4 segment
Material
 Local anesthetic: 3–5mL
Local anesthetic: 3–5mL
 Needle: 0.4 × 40 mm
Needle: 0.4 × 40 mm
Technique
 The needle is inserted on the median line, inferior to the easily palpable patellar tip and is advanced approximately 1–1.5 cm. Following aspiration (to avoid intra-articular injection), 1–1.5 mL of a local anesthetic is injected.
The needle is inserted on the median line, inferior to the easily palpable patellar tip and is advanced approximately 1–1.5 cm. Following aspiration (to avoid intra-articular injection), 1–1.5 mL of a local anesthetic is injected.
 The next injections are performed in the pain area, approximately 1 finger width next to the midline, on the medial aspect of the knee. 1–1.5 mL of a local anesthetic is injected at points 1–1.5 cm apart across the joint, with the patient’s knee extended. The needle is inserted only 0.5–1 cm. Aspiration is vital to avoid intraarticular injection.
The next injections are performed in the pain area, approximately 1 finger width next to the midline, on the medial aspect of the knee. 1–1.5 mL of a local anesthetic is injected at points 1–1.5 cm apart across the joint, with the patient’s knee extended. The needle is inserted only 0.5–1 cm. Aspiration is vital to avoid intraarticular injection.
 In addition, superior to the patella, medially and laterally to the attachment site of the rectus femoris, 1 mL of a local anesthetic is injected. The borders of the muscle can be easily palpated by having the patient lift the extended leg.
In addition, superior to the patella, medially and laterally to the attachment site of the rectus femoris, 1 mL of a local anesthetic is injected. The borders of the muscle can be easily palpated by having the patient lift the extended leg.
Risks
 Unintentional intra-articular injection occurs very easily. Superficial injection suffices at this location; therefore, the insertion depth of 0.50–1 cm must not be exceeded and prior aspiration is required.
Unintentional intra-articular injection occurs very easily. Superficial injection suffices at this location; therefore, the insertion depth of 0.50–1 cm must not be exceeded and prior aspiration is required.
Concomitant Therapies
 Depending on the underlying disorder, physical strain must be adjusted through corrections to the soles of shoes (internal and external sole lift) and adjustments regarding the foot statics or leg length. Frequently, especially in younger patients, considerable imbalance of the vastus medialis and the vastus lateralis can be seen. This requires adjuvant strengthening exercises for the vastus medialis. If the tibiofibular joint is affected, joint mobilization through manual therapy is recommended.
Depending on the underlying disorder, physical strain must be adjusted through corrections to the soles of shoes (internal and external sole lift) and adjustments regarding the foot statics or leg length. Frequently, especially in younger patients, considerable imbalance of the vastus medialis and the vastus lateralis can be seen. This requires adjuvant strengthening exercises for the vastus medialis. If the tibiofibular joint is affected, joint mobilization through manual therapy is recommended.
 In persistent irritations and positive McMurray test result or Cooper sign, the joint should be assessed using arthroscopy or MRI. Osteochondritis dissecans and osteochondral necrosis may be ruled out using radiologic assessment.
In persistent irritations and positive McMurray test result or Cooper sign, the joint should be assessed using arthroscopy or MRI. Osteochondritis dissecans and osteochondral necrosis may be ruled out using radiologic assessment.
 In acute pain, temporary respite from athletic activities is recommended.
In acute pain, temporary respite from athletic activities is recommended.
 In knee pain without organic correlation but with headache, a combination of acupuncture points ST-36, close to the knee, and ST-6, ST-8, and LI-4 has been successful.
In knee pain without organic correlation but with headache, a combination of acupuncture points ST-36, close to the knee, and ST-6, ST-8, and LI-4 has been successful.
 Additional injection of 0.5 mL of a local anesthetic in the area of GB-34 and GB-40, yuan source point, is helpful. Always inquire about functional disorders of the lumbar spine in combination with headache.
Additional injection of 0.5 mL of a local anesthetic in the area of GB-34 and GB-40, yuan source point, is helpful. Always inquire about functional disorders of the lumbar spine in combination with headache.
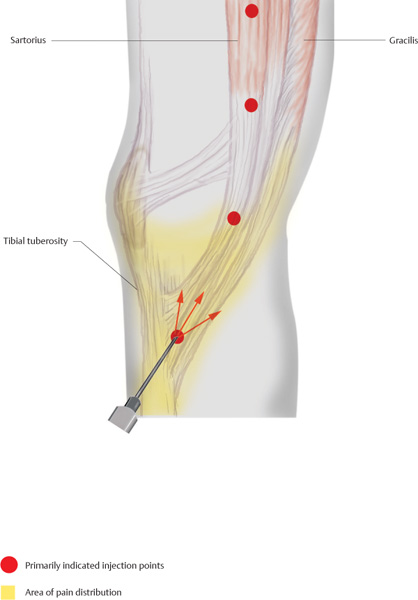
Gracilis and Pes Anserinus Pain Syndromes
Indications
 Median knee attachment tendinosis
Median knee attachment tendinosis
 Overstrain syndrome of the knee joint capsule
Overstrain syndrome of the knee joint capsule
 Adjuvant treatment in median gonarthritis
Adjuvant treatment in median gonarthritis
Material
 Local anesthetic: 3 mL
Local anesthetic: 3 mL
 Needle: 0.4 × 40 mm
Needle: 0.4 × 40 mm
Technique
 With the patient’s knee in extension, a strong tapering muscular bulge at the medial joint line can be palpated. If it is palpated distally, its attachment at the tibial head is located. Here, the needle is inserted pointing superiorly and the attachment area is flooded with a local anesthetic in a fan-shaped pattern.
With the patient’s knee in extension, a strong tapering muscular bulge at the medial joint line can be palpated. If it is palpated distally, its attachment at the tibial head is located. Here, the needle is inserted pointing superiorly and the attachment area is flooded with a local anesthetic in a fan-shaped pattern.
 On a vertical cranial line that initially deviates slightly posteriorly, two to three additional intracutaneous quaddles are set 2 cm apart. Each quaddle receives 0.2 mL of the injectable.
On a vertical cranial line that initially deviates slightly posteriorly, two to three additional intracutaneous quaddles are set 2 cm apart. Each quaddle receives 0.2 mL of the injectable.
Risks
 Anesthesia of the saphenous nerve and its infra-patellar branch
Anesthesia of the saphenous nerve and its infra-patellar branch
 Intra-articular injection
Intra-articular injection
 Intra-articular injection can be safely avoided if the needle is inserted as indicated, cranially at a shallow angle. If the saphenous nerve is temporarily anesthetized, the patient must be informed about the temporary characteristics.
Intra-articular injection can be safely avoided if the needle is inserted as indicated, cranially at a shallow angle. If the saphenous nerve is temporarily anesthetized, the patient must be informed about the temporary characteristics.
Concomitant Therapies
 Iontophoretic treatment, local cryogenic friction massage
Iontophoretic treatment, local cryogenic friction massage
 Relaxation of the sartorius, semitendinosus, and gracilis using physical therapy
Relaxation of the sartorius, semitendinosus, and gracilis using physical therapy
 Anti-inflammatory occlusive bandage
Anti-inflammatory occlusive bandage
 Alternating knee affusion according to Kneipp
Alternating knee affusion according to Kneipp
 Therapy through Muscles, Tendons, and Ligaments
Therapy through Muscles, Tendons, and Ligaments
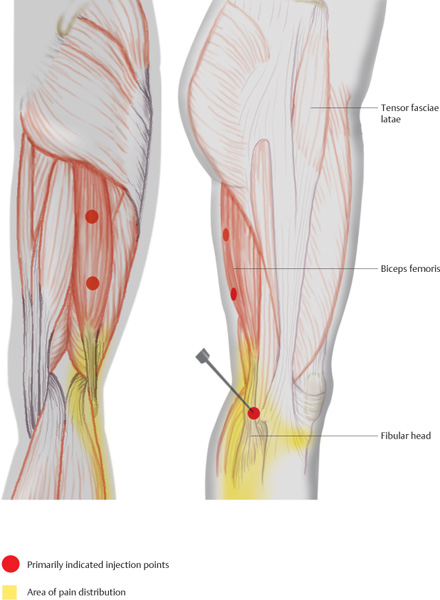
Biceps Femoris
Indications
 Painful lateral edge of the knee joint, painful fibular head
Painful lateral edge of the knee joint, painful fibular head
 Myotenositis of the biceps femoris
Myotenositis of the biceps femoris
Differential Diagnoses
 Lesion of the lateral meniscus
Lesion of the lateral meniscus
 Irritation of the infrapatellar nerve
Irritation of the infrapatellar nerve
 Maisonneuve fracture
Maisonneuve fracture
Material
 Local anesthetic: 2 mL
Local anesthetic: 2 mL
 Needle: 0.4 × 40 mm
Needle: 0.4 × 40 mm
Technique
 The fibular is easily located through palpation. The needle is inserted 1 cm superior, pointing toward the fibular head.
The fibular is easily located through palpation. The needle is inserted 1 cm superior, pointing toward the fibular head.
 After bone contact has been made, the injectable is administered as the needle is retracted.
After bone contact has been made, the injectable is administered as the needle is retracted.
Risks
 Anesthesia of the peroneus nerve. The nerve reaches the fibular head from posteriorly, and spirals around it in a superior direction. Anesthesia of the peroneus nerve can be safely avoided if the needle makes bone contact prior to injection.
Anesthesia of the peroneus nerve. The nerve reaches the fibular head from posteriorly, and spirals around it in a superior direction. Anesthesia of the peroneus nerve can be safely avoided if the needle makes bone contact prior to injection.
Concomitant Therapies
 Mobilization of the tibiofibular joint using manual therapy
Mobilization of the tibiofibular joint using manual therapy
 Friction massage
Friction massage
 Ultrasound applications
Ultrasound applications
 Cryotherapy
Cryotherapy
 Acupuncture (ST-36, ST-35)
Acupuncture (ST-36, ST-35)
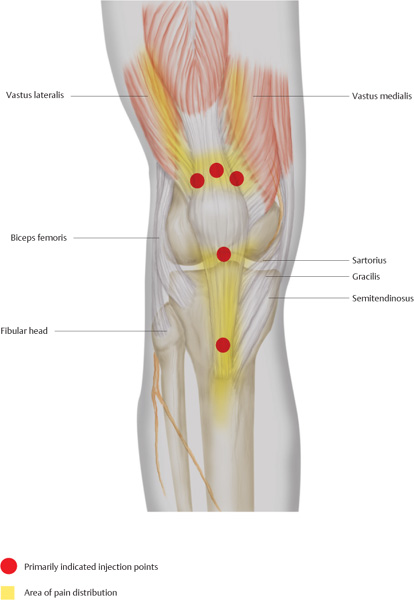
Quadriceps Femoris
Indications
 Pain appears especially near the knee joint superior to the patella and in terms of lower patellar pole syndromes.
Pain appears especially near the knee joint superior to the patella and in terms of lower patellar pole syndromes.
 Adjuvant treatment in patellar chondropathy and retropatellar arthrosis
Adjuvant treatment in patellar chondropathy and retropatellar arthrosis
Differential Diagnoses
 Free joint body
Free joint body
 Prepatellar bursitis
Prepatellar bursitis
 Gonarthrosis, gonarthritis
Gonarthrosis, gonarthritis
Material
 Local anesthetic: 3 mL
Local anesthetic: 3 mL
 Needle: 0.4 × 44 mm
Needle: 0.4 × 44 mm
Technique
 The superior edge of the patella is palpated and three or four injections are performed superior to the palpable bony edge. First an intracutaneous quaddle is set, the needle is then advanced 0.5 cm, and 0.3 mL of a local anesthetic is injected at each site.
The superior edge of the patella is palpated and three or four injections are performed superior to the palpable bony edge. First an intracutaneous quaddle is set, the needle is then advanced 0.5 cm, and 0.3 mL of a local anesthetic is injected at each site.
 In the area of the inferior patellar pole, the procedure is repeated. The insertion is directed toward the bone. Below the bone, close to the patellar periosteum, 0.5 mL of a local anesthetic is injected. The depth of insertion is 0.5 cm.
In the area of the inferior patellar pole, the procedure is repeated. The insertion is directed toward the bone. Below the bone, close to the patellar periosteum, 0.5 mL of a local anesthetic is injected. The depth of insertion is 0.5 cm.
 Finally, in the area of the palpable tibial tuberosity, a quaddle is set at its superior edge. The needle is then advanced until bone contact is made. After the needle has been retracted 1 mm, 0.5 mL of a local anesthetic is injected.
Finally, in the area of the palpable tibial tuberosity, a quaddle is set at its superior edge. The needle is then advanced until bone contact is made. After the needle has been retracted 1 mm, 0.5 mL of a local anesthetic is injected.
Risks
 Unintentional intra-articular injection; this can be avoided by observing the depth of insertion and making bone contact with the needle prior to injection.
Unintentional intra-articular injection; this can be avoided by observing the depth of insertion and making bone contact with the needle prior to injection.
Concomitant Therapies
 Traction mobilization of the patella
Traction mobilization of the patella
 In muscular imbalances, it is frequently necessary to strengthen the vastus medialis through exercises.
In muscular imbalances, it is frequently necessary to strengthen the vastus medialis through exercises.
 Prescription of quadriceps support aids, for example, negative heel
Prescription of quadriceps support aids, for example, negative heel
 Priessnitz compress
Priessnitz compress
 Medical exercise therapy
Medical exercise therapy
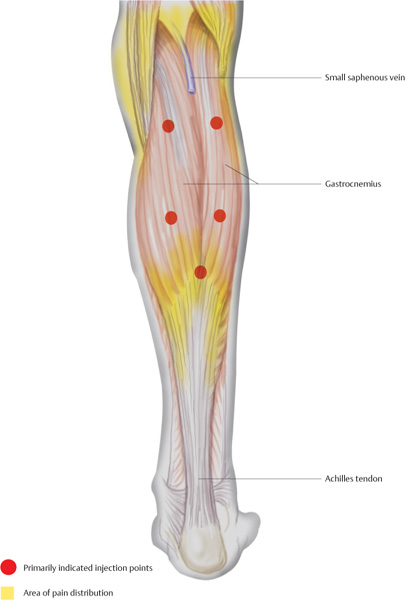
Triceps Surae
Indications
 Calf pain, radiating into the Achilles tendon
Calf pain, radiating into the Achilles tendon
 Adjuvant treatment in:
Adjuvant treatment in:
Differential Diagnoses
 Venous insufficiency
Venous insufficiency
 Deep vein thrombosis
Deep vein thrombosis
 Compartment syndrome
Compartment syndrome
 Peripheral arterial occlusion
Peripheral arterial occlusion
Material
 Local anesthetic: 5 mL
Local anesthetic: 5 mL
 Needle: 0.5 × 50 mm
Needle: 0.5 × 50 mm
Technique
 The patient is in the pronated position and attempts plantar flexion of the foot against resistance. This requires tensing the gastrocnemius and the soleus. The superior border of the two gastrocnemius heads is located. The needle is inserted 2 cm and 0.5 mL of a local anesthetic is injected on each side.
The patient is in the pronated position and attempts plantar flexion of the foot against resistance. This requires tensing the gastrocnemius and the soleus. The superior border of the two gastrocnemius heads is located. The needle is inserted 2 cm and 0.5 mL of a local anesthetic is injected on each side.
 Five centimeters distally, on top of the muscle bellies, the needle is inserted 2 cm and 0.5 mL of a local anesthetic is injected bilaterally. The needle is then advanced another 2 cm and the injectable is administered again.
Five centimeters distally, on top of the muscle bellies, the needle is inserted 2 cm and 0.5 mL of a local anesthetic is injected bilaterally. The needle is then advanced another 2 cm and the injectable is administered again.
 The distal conjunction of the gastrocnemius heads is located. A notch on the median line indicates the precise injection site. The needle is inserted vertically 2 cm and 0.5 mL of a local anesthetic is injected.
The distal conjunction of the gastrocnemius heads is located. A notch on the median line indicates the precise injection site. The needle is inserted vertically 2 cm and 0.5 mL of a local anesthetic is injected.
Risks
 Injection into the small saphenous vein
Injection into the small saphenous vein
 If the needle is advanced excessively, the tibial nerve may be anesthetized.
If the needle is advanced excessively, the tibial nerve may be anesthetized.
Concomitant Therapies
 Muscular relaxation using physical therapy
Muscular relaxation using physical therapy
 Connective-tissue massage
Connective-tissue massage
 Traction mobilization of the knee joint and the ankle joint
Traction mobilization of the knee joint and the ankle joint
 Supportive heel lift, if applicable
Supportive heel lift, if applicable
 Calf affusion according to Kneipp
Calf affusion according to Kneipp
 Priessnitz compress, cupping therapy
Priessnitz compress, cupping therapy
Peronei
Indications
 Pain in the area of the lateral lower leg
Pain in the area of the lateral lower leg
 Pain along the course of the tendon at the lateral malleolus
Pain along the course of the tendon at the lateral malleolus
 Adjuvant treatment in:
Adjuvant treatment in:
Differential Diagnoses
 Compartment syndrome
Compartment syndrome
 Peripheral arterial occlusion
Peripheral arterial occlusion
Material
 Local anesthetic: 3 mL
Local anesthetic: 3 mL
 Needle: 0.4 × 40 mm
Needle: 0.4 × 40 mm
Technique
 The patient is in the lateral position. The prominent fibular head is palpated. The first injection is performed directly inferior to the fibular head, at the transition onto the muscle attachment. The needle is inserted vertically until bone contact is made. The needle is then retracted 1 mm and 0.5 mL of a local anesthetic is injected.
The patient is in the lateral position. The prominent fibular head is palpated. The first injection is performed directly inferior to the fibular head, at the transition onto the muscle attachment. The needle is inserted vertically until bone contact is made. The needle is then retracted 1 mm and 0.5 mL of a local anesthetic is injected.
 On a straight line down to the lateral malleolus, two additional injections are performed 4 cm apart. The needle is inserted vertically 1 cm and 0.5 mL of a local anesthetic is administered.
On a straight line down to the lateral malleolus, two additional injections are performed 4 cm apart. The needle is inserted vertically 1 cm and 0.5 mL of a local anesthetic is administered.
 The final injection is performed posterior to the lateral malleolus. Nearly parallel to the peroneal tendon, the needle is inserted caudally at a shallow angle into the tendon sheath. Then, 0.5 mL of a local anesthetic is injected.
The final injection is performed posterior to the lateral malleolus. Nearly parallel to the peroneal tendon, the needle is inserted caudally at a shallow angle into the tendon sheath. Then, 0.5 mL of a local anesthetic is injected.
Risks
 If the injectable is administered posterior to the fibular head, the peroneal nerve may be anesthetized and temporary weakness in dorsal flexion of the foot may result.
If the injectable is administered posterior to the fibular head, the peroneal nerve may be anesthetized and temporary weakness in dorsal flexion of the foot may result.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree