Figure 24.1
A window is made behind the IMA and IMV to isolate these structures prior to transection. The hypogastric nerves are identified and swept posteriorly to avoid injury
A total mesorectal excision is then performed by retracting the distal sigmoid colon and rectum anteriorly and finding the avascular plane behind the mesorectum (Fig. 24.2). The peritoneum is first scored on either side of the rectum down to its anterior reflection which is also incised. Then electrocautery is used to dissect the areolar tissues posteriorly and laterally down to the level of the pelvic floor, keeping the mesorectal envelope intact (Fig. 24.3). Care should be taken to avoid the hypogastric nerves which course along the pelvic sidewalls bilaterally. Injury to these nerves can result in sexual and urinary dysfunction. Anteriorly, the dissection follows closely along the rectum and care is taken to avoid injury to the seminal vesicles and prostate gland in the male and the posterior vaginal wall in the female (Fig. 24.4). Preservation of the fascia propria which envelops the rectum is a key maneuver that has been shown to reduce local tumor recurrence [3, 4]. The dissection continues distally until the levator muscles have been identified circumferentially at the pelvic floor, and the mesorectum has ended.
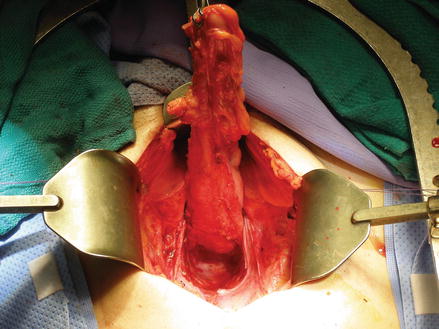
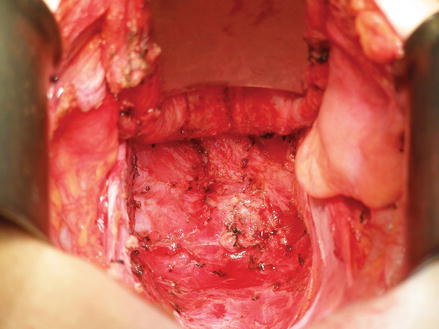

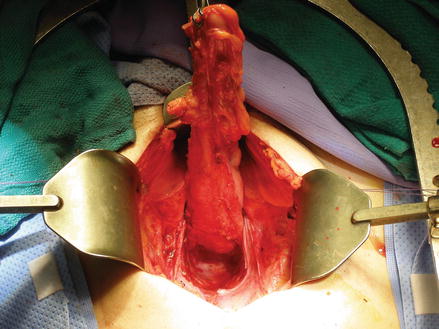
Figure 24.2
The divided colon is retracted anteriorly to visualize the posterior, avascular, retro-rectal dissection plane
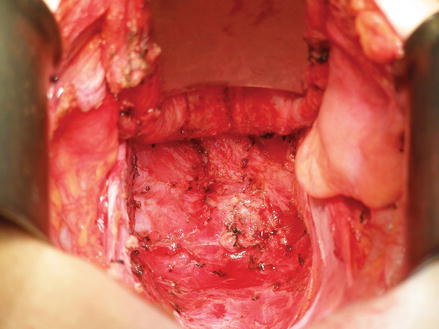
Figure 24.3
The total mesorectal excision is performed by dissecting in the avascular plane posterior to the mesorectum and anterior to the sacrum. The dissection continues down to the levator muscles bilaterally. Identification and preservation of the hypogastric nerves is maintained throughout the dissection

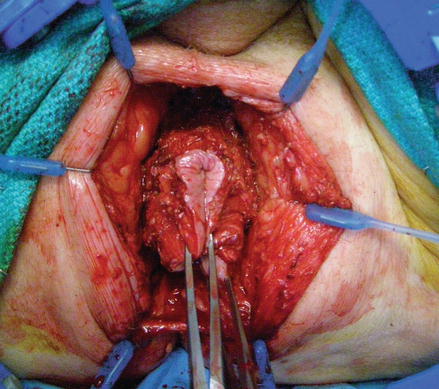
Figure 24.4
In females, the dissection continues between the anterior rectum and posterior vaginal wall, leaving the anterior mesorectum intact. In males, care should be taken to avoid injuring the prostatic urethra
For upper third rectal tumors, a general margin of approximately 5 cm is suggested. In these cases the mesorectum may be divided perpendicular to the rectum. For middle or lower third rectal tumors, a complete mesorectal excision is necessary and a distal margin of 2 cm is customary, although a smaller margin may be acceptable in certain patient populations where preservation of the sphincter complex is possible, especially after neo-adjuvant treatment [15]. The rectum is divided distal to the tumor with an appropriate margin with a thoracoabdominal (TA) linear stapler and a scalpel (Fig. 24.5). A digital rectal exam should be performed after the TA has been positioned to confirm appropriate location prior to completion of the resection. The specimen should be opened on the back table and subsequently sent to pathology to confirm negative margins. An anvil is then secured within the lumen of the proximal colon using a purse-string suture. Care should also be taken to exclude epiploica, colonic fat, or diverticula from the surface of the anvil as these can compromise the integrity of the staple line. The end-to-end circular stapler is then inserted transanally and gently maneuvered into place so that the spike is deployed in the center of the distal staple line (Fig. 24.6). The anvil is secured to the circular stapler spike and the stapler is then closed and fired. The alignment of the descending colon should be confirmed to be in a straight line with no tension and all small bowel loops cleared from the surgical area prior to completing to anastomosis. The stapler is then slowly removed until the luminal anvil has traversed the new anastomosis. The anastomotic rings are inspected on the back table to ensure a full circumferential anastomosis and sent to pathology for evaluation. A leak test is typically performed.
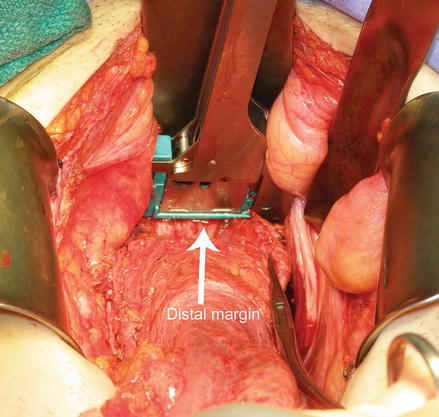
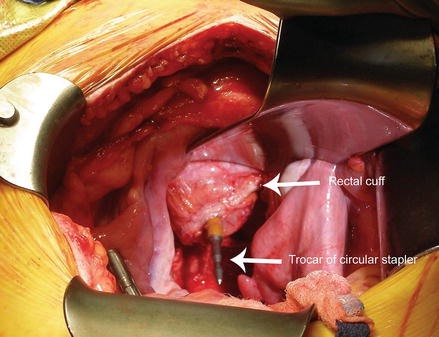
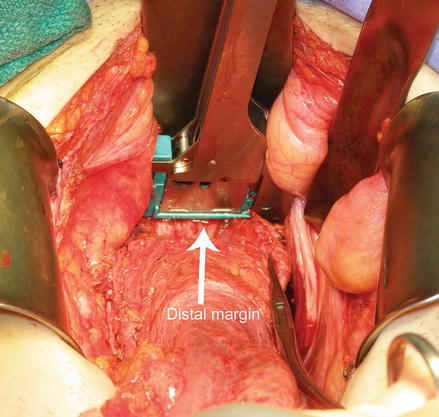
Figure 24.5
When performing an LAR, at the completion of the mesorectal mobilization, the rectum is transected at least 1 cm beyond the level of the tumor utilizing a transverse, non-cutting stapler
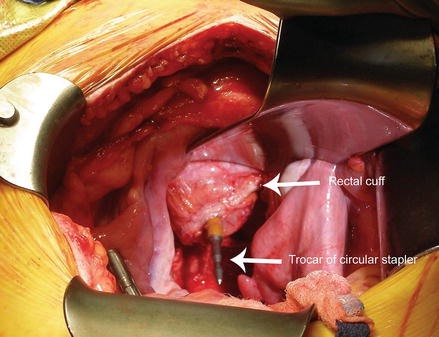
Figure 24.6
An assistant then inserts the circular stapler through the anus and into the rectal pouch. The spike is advanced until it is visualized penetrating the center of the rectal cuff staple line. It is then fully deployed prior to attaching the anvil component and completing the anastomosis
Alternatively, for extremely low-lying rectal tumors, a colo-anal anastomosis can be performed with a colonic J-pouch in either a hand-sewn or stapled fashion. Colonic J-pouches may confer some advantages, such as reduced fecal incontinence, reduce frequency of bowel movements and urgency [16]. The J-pouch is configured by folding the distal colon back upon itself approximately 5–6 cm (Fig. 24.7). A colotomy is made at the base of the fold with cautery. A linear GIA stapler is then inserted through the colotomy with each arm passing into a separate lumen and fired, creating a common pouch. An anvil is then placed through this colotomy and a secured in place. The anastomosis is completed as previously described. A hand-sewn colo-anal anastomosis is typically performed when the rectum must be sharply divided without closure, rather than using a stapler, in order to obtain a distal margin. A retractor is placed at the anal opening to view the dental line and the proximal resection margin. The segment of proximal colon is then brought down into the surgical field and full-thickness interrupted absorbable sutures are used to circumferentially sew the colon to the anal canal.
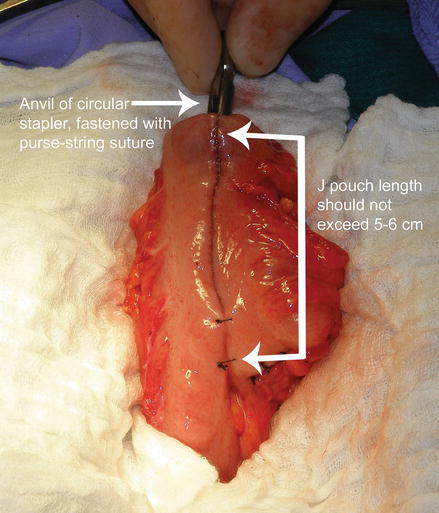
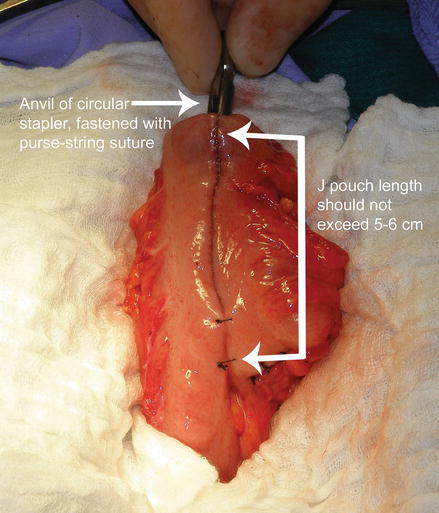
Figure 24.7
A colonic J-pouch is illustrated. The colon is folded over on itself and a side-to-side J-pouch is constructed with a linear cutting stapler. The J-pouch length should not exceed 5–6 cm in order to optimize post-operative function. The anvil of the circular stapler is placed at the apex and secured with a purse-string suture
In most LAR cases, especially post-chemoradiation therapy, a diverting loop ileostomy (see Stoma section) is performed to reduce the morbidity associated with anastomotic leak.
Abdominoperineal Resection
APR is indicated for low-lying rectal cancers which are close to or involve the anal sphincter complex, in patients who require a rectal resection and have fecal incontinence at baseline, or those with severe peri-anal inflammatory bowel disease in whom a distal anastomosis is not advised. The procedure involves the en bloc removal of the rectum, mesorectum, and anus.
The abdominal portion of the APR is identical to the LAR. After complete mobilization of the rectum and mesorectum, the perineal dissection begins. The patient’s legs can be adjusted as needed to a high lithotomy position to expose the perineum. The anus is then exposed with a self-retaining retractor. An elliptical incision is made sharply around the anus and includes the entire anal sphincter complex (Fig. 24.8). Dissection continues posteriorly until the coccyx is encountered. The anococcygeal ligament is divided and blunt dissection is used to enter the presacral space just anterior to the coccyx that had been previously dissected transabdominally (Fig. 24.9). A finger can then be placed deep to the levator muscles laterally on either side to act as a guide for division bilaterally with cautery. Dissection then continues to the anterior aspect of the anal canal and distal rectum. This portion of the dissection can be quite challenging in males as the membranous portion of the prostatic urethra is just anterior to this plane and can be easily damaged. In females, retraction of the vagina can facilitate separation of the anterior rectum and posterior vaginal wall. Eversion of the specimen through the perineal opening can also assist in completing the anterior dissection plane (Fig. 24.10). Once the specimen has been completely dissected circumferentially, it is removed from the perineal opening and sent to pathology for permanent section (Fig. 24.11). The perineal incision in then closed in multiple layers in an anterior-posterior fashion using absorbable suture. We typically close the skin with nylon suture (Fig. 24.12). After the perineum has been closed, attention is then turned to the creation of an end colostomy, which is described in the Stoma section. Much of the abdominal and perineal portions of the APR procedure can be done simultaneously by two operating surgeons.