CHAPTER 9 Lower limb blocks
Femoral nerve block (3-in-1 block)
Landmark technique
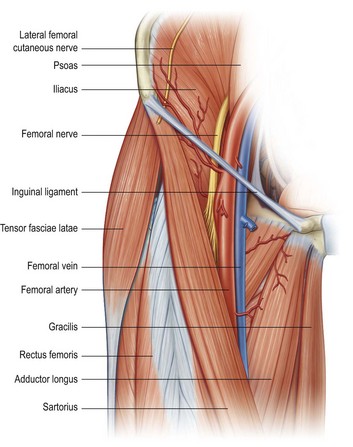
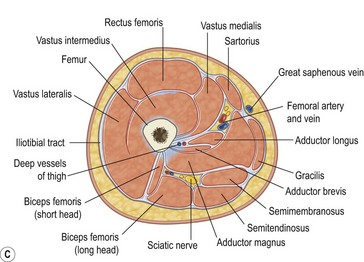
The femoral nerve arises from the L2, L3 and L4 nerve roots. The nerve descends between the psoas and the iliacus muscles and passes deep to the inguinal ligament into the thigh (Fig. 9.1). At this point the femoral nerve is positioned immediately lateral to and slightly deeper than the femoral artery. The acronym NAVY is a useful reminder of the arrangement of structures from lateral to medial: Nerve, Artery, and Vein, with Y representing the midline.
Preparation
Technique
Ultrasound technique
Preparation
Technique
In-plane approach
Out-of-plane approach
The injection process
Lateral femoral cutaneous nerve block
Preparation
Technique
Sciatic nerve block
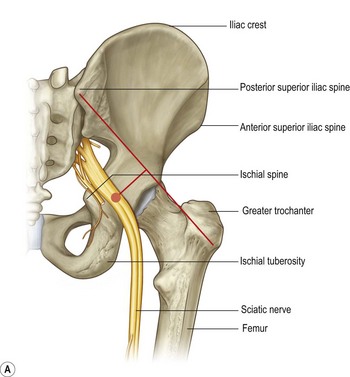
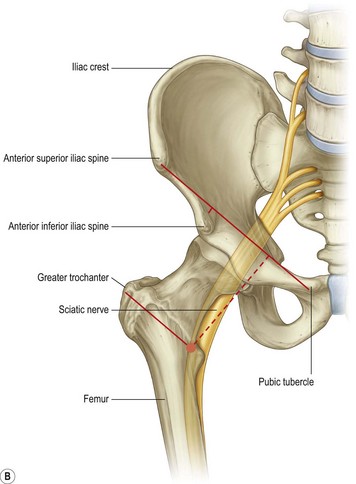
Sciatic blockade (via the posterior, anterior or popliteal approach) has the potential to be one of the most commonly used regional anaesthetic techniques in the ED and can be invaluable for pain management following trauma to the lower limb (Fig. 9.10). This block is relatively easy and is associated with a high success rate when properly performed. It is particularly well suited for injuries to the leg, ankle, and foot. It provides complete anaesthesia of the leg below the knee with the exception of a medial strip of skin which is innervated by the saphenous nerve. When combined with a femoral nerve block or 3-in-1 block, anaesthesia of almost the entire lower limb distal to the mid-thigh is achieved. If spinal immobilisation procedures are required, rather use the anterior or the popliteal approach, which require less movement of the patient and the injured limb.
Posterior approach landmark technique
Preparation
Technique
Posterior approach ultrasound technique
Preparation
Technique
In-plane approach
Out-of-plane approach
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree