Figure 20.1
Patient positioning during a laparoscopic splenectomy. The patient is placed on the operating room table in the right “lazy” decubitus position using a bean bag with the right arm abducted and the left arm adducted anterior and superior. This positioning allows gravity to assist in the dissection of the splenic attachments and it leaves the abdomen readily accessible if a quick conversion to a laparotomy is required
General endotracheal anesthesia is required. Deep vein thrombosis prophylaxis is administered (typically 40 mg enoxaparin subcutaneously) and sequential compression devices are applied prior to induction. A Foley catheter is placed to monitor fluid status in select patients. An orogastric tube is placed to decompress the stomach and minimize the likelihood of gastric injury; this is particularly important because we access the abdomen using a Veress technique in the left upper quadrant. Patients also receive preoperative antibiotic prophylaxis.
Description of Procedure
Abdominal Access
Entry into the abdomen is performed using a Veress needle in the left upper quadrant (Fig. 20.2). We prefer a Veress approach due to the relatively high frequency of obesity in our patient population. Intra-abdominal positioning of the needle is confirmed by aspiration and a negative saline drop test. Pneumoperitoneum is then established by insufflating the abdomen to a pressure of 15 mmHg with carbon dioxide. A 5 mm port is placed into the abdomen either through the Veress incision or via an adjacent incision in the left upper quadrant.
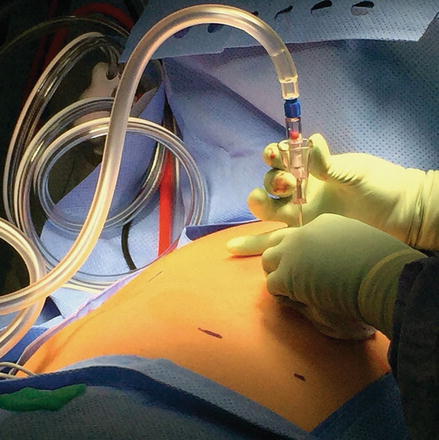
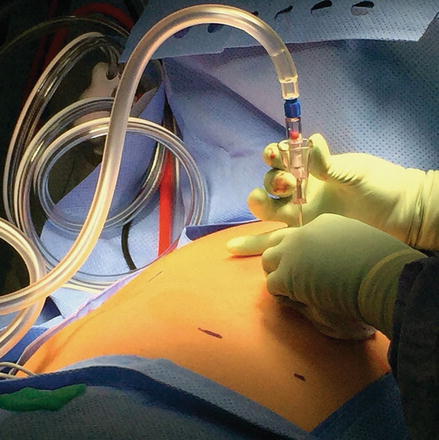
Figure 20.2
Entry into the abdomen with Veress needle technique. A Veress needle is placed 3 cm below the left subcostal border in the midclavicular line. Intra-abdominal positioning of the needle is confirmed by aspiration and a negative saline drop test
Alternatively, using the Hasson technique, a 1 cm upper midline vertical incision is made approximately 15 cm inferior to the xiphoid process. The fascia is elevated and incised, and entry into the intra-abdominal cavity is confirmed by direct visualization. Two figure-of-eight absorbable sutures are placed in the fascia and the Hasson cannula is inserted under direct visualization.
Either a 5 mm or 10 mm, 30° laparoscope is then inserted through the first trocar and the intra-abdominal cavity is inspected for any injury or pathology. Additional ports are inserted at the supra-umbilical position, right upper midline, left mid-abdomen at the anterior axillary line, and left lower mid-abdomen at the mid-clavicular line. The left lower mid-abdominal port at the mid-clavicular line is typically a 12 mm port, which allows passage of an endo-GIA stapler. To avoid direct trocar injuries to the spleen, these trocar positions may vary if a patient has splenomegaly (Fig. 20.3).


Figure 20.3
Trocar placement for laparoscopic splenectomy. Ports are inserted at the supra-umbilical position, right upper midline, left mid-abdomen at the anterior axillary line, and left lower mid-abdomen at the mid-clavicular line. After inspection of the abdomen, the left lower mid-abdominal 5 mm trocar (shown) was upsized to a 12 mm port to accommodate passage of the endo-GIA stapler. These trocar positions may vary if a patient has splenomegaly or other anatomical limitation
Division of the Short Gastrics
The greater curve of the stomach at the level of the inferior margin of the spleen is grasped and retracted anteriorly and to the patient’s right. The adjacent omentum is retracted in the opposite direction. The short gastric vessels are then divided with the bipolar coagulating device and the lesser sac is entered (Fig. 20.4). There are typically two layers of attachments that need to be transected and often a posterior layer of short gastrics. Division is complete once the left crus of the diaphragm is visualized.
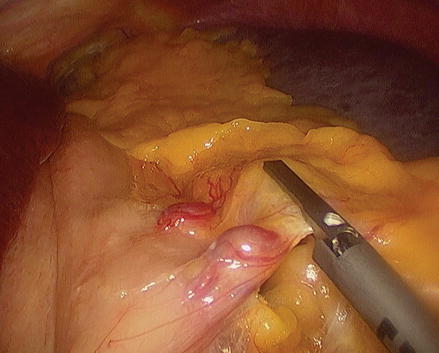
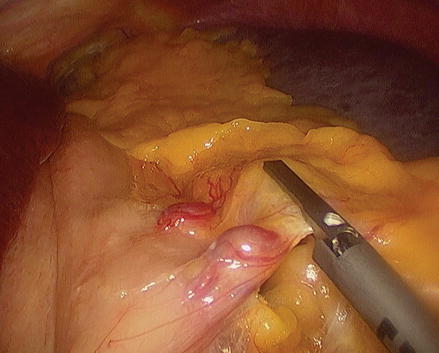
Figure 20.4
Mobilization of the stomach. The short gastric vessels are divided with the bipolar coagulating device, mobilizing the stomach from the spleen
Division of the Splenic Artery
Division of the short gastrics allows entry into the lesser sac and visualization of the anterior surface of the pancreas. The splenic artery can usually be identified inferior and anterior to the splenic vein. After circumferential exposure, the splenic artery is transected with an endoscopic vascular linear stapler (Fig. 20.5). The pancreas is inspected to ensure that no injury occurred. If there is concern about possible pancreatic injury, a 15 Fr Blake drain is placed in the splenic bed to both identify and manage a possible pancreatic fistula. If it is not possible to isolate the splenic artery at this location, the arterial and venous splenic branches will be transected at the hilum.
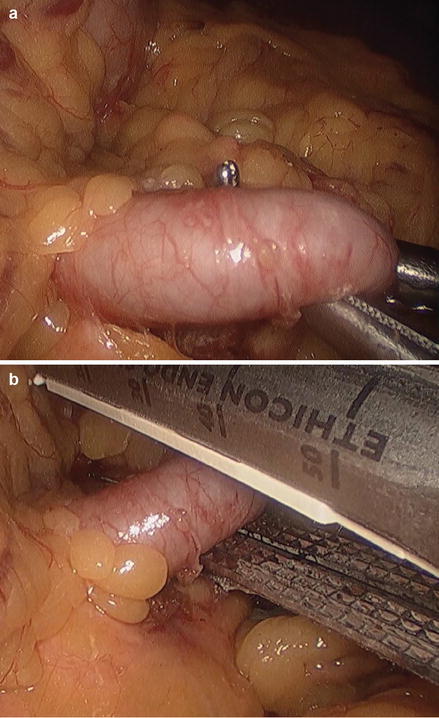
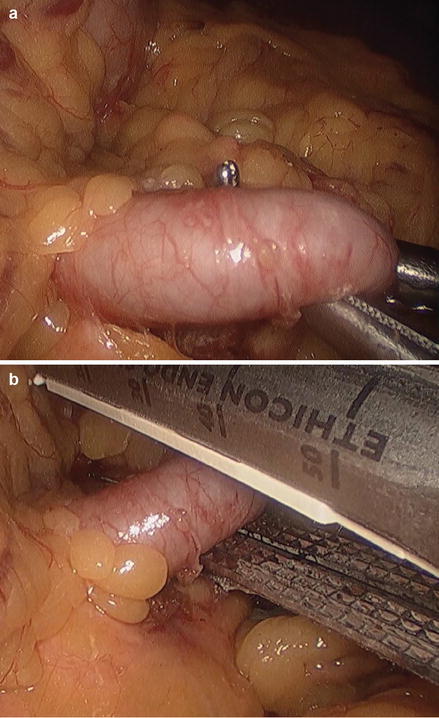
Figure 20.5
Division of the splenic artery. At the hilum, the splenic artery is exposed circumferentially (panel a) and then transected with an endoscopic vascular linear stapler (panel b)
Division of the Splenic Vein Branches
The splenic flexure of the colon is mobilized inferiorly. The splenocolic ligament is then exposed and divided using a bipolar coagulating device. Once the splenic flexure is mobilized away from the spleen, dissection continues starting at the inferior pole of the spleen and proceeds toward the upper pole of the spleen. A grasper should easily pass posterior to the branches of the splenic vein along the medial margin of the spleen (Fig. 20.6). Multiple firings of the endo-GIA vascular load 60 mm stapler are performed. The stapler should slide smoothly with each passage (Fig. 20.7). This completes division of the blood supply to the spleen.










