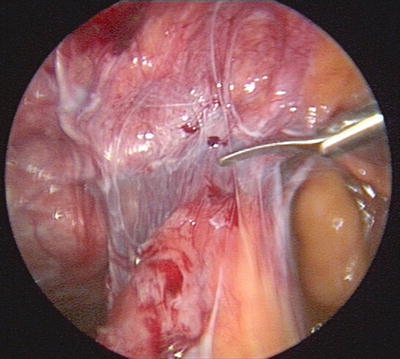
Fig. 7.1
Wound over hernia defect
The ability to repair multiple defects with a single prosthetic through small laparoscopy incisions.
Cosmetic advantage of laparoscopic surgery.
Less pain and faster recovery: many studies have documented the decreased need for pain medication in the postoperative period and earlier return to normal activities with LVHR compared to OVHR.
Disadvantages of LVHR include:
Increased cost of operative supplies.
Need for general anesthesia in all cases.
Typically, increased time of operation, especially early in the surgeon’s experience.
Need for specialized coated mesh: intraperitoneal placement of mesh means that it is likely to come in contact with the bowel.
Higher risk for missed intestinal injury, with possibility of fistula, sepsis, and death.
Indications
Nearly all ventral hernias can be approached laparoscopically. As the complexity of the hernia increases and/or the number of patient comorbidities increase, the skill level required to repair the hernia will also increase. Thus the true indication for a laparoscopic ventral hernia repair is dependent on the comfort level of the surgeon. Primary ventral hernias (umbilical or epigastric) and first time incisional hernias are the most straightforward, and the vast majority of these are candidates for laparoscopic repair. Multiply recurrent hernias, incarcerated hernias, and parastomal hernias are more complicated but still may be approached with LVHR. Often these patients see the most benefit from LVHR, compared to OVHR. Complex abdominal wall reconstruction for hernia with loss of domain remains an open procedure.
Preoperative Preparation
Patient preparation is identical to that for OVHR. Patients with comorbid conditions need these optimized prior to elective repair. Smoking cessation, weight loss, and control of diabetes and metabolic deficits have the same advantages in decreased complications and increased chance for successful repair in LVHR as in OVHR. Consider a CT scan to image the hernia anatomy, but it is not absolutely necessary. Consider a bowel prep only if the patient has large intestine in the hernia. All patients should receive a dose of prophylactic preoperative antibiotics and DVT prophylaxis.
Most importantly, ensure that you have the proper supplies for your operation. In addition to an angled 5 mm laparoscope and standard laparoscopy supplies, you will need a mechanical fixation device, a suture passing device, and an assortment of sizes of specialty mesh that include an adhesion barrier bonded to one side. Mesh is either polypropylene or polyester, and there are several proprietary adhesion barrier systems that are applied to one side of the mesh. It is also helpful to have access to energy sources that will help with the dissection of the hernia, such as bipolar cautery shears or ultrasonic dissection.
Operative Strategy
The hernia is approached from within the peritoneum, reduced, and repaired with an intraperitoneal onlay of permanent mesh. This mesh is then secured to the abdominal wall with transfascial fixation sutures placed through the entire abdominal wall. The mesh overlaps the healthy fascia by at least 5 cm in every direction.
Proper initial placement of the trocars is essential to facilitate completion of the procedure. Trocars should be placed away from the defect, far enough to allow the surgeon to work at a reasonable angle to fix the defect, but close enough to allow the instruments to reach the furthest part of the mesh. Surgeon and assistant typically work from one side of the defect, but must be able to alter their positions and placement of the scope and instruments through their ports to work around all sides of the hernia. Primary and slave video monitors are needed if the surgeon will be working from more than one angle, which is often the case (Fig. 7.2).
Fig. 7.2
Illustration of typical patient setup
Operative Technique
The patient is placed under general anesthesia with complete muscle relaxation. The arm on the side where the surgeon plans to work should be tucked to allow the surgeon and assistant to operate without restriction. Foley catheter placement may be necessary for lower abdominal hernias and cases that are expected to take a long time. The abdomen should be prepped and draped as widely as possible. Initial planning for trocar placement is critical.
If the hernia is in the midline, the first choice for Veress needle placement is at the costal margin in the left upper quadrant. The abdominal wall is fixed at this point, the liver is not near the entry point, and most patients have not had surgery in this region. The right upper quadrant would be an alternative if prior left upper quadrant surgery has been performed. A laparoscopic port can then be placed at any desired location. If a Hasson approach is going to be utilized, then placement can be in either the right or left abdomen, depending on lowest expected adhesions. The angled 5 mm laparoscope is then inserted, and the additional 2 or 3 ports can be placed under direct vision. A 4-port technique is useful to allow the surgeon to operate with both hands, the assistant to hold the scope and provide additional retraction with a grasper. The ports are best arrayed in a semicircle around about half the circumference of the hernia. When placing the ports, consider that mesh will overlap normal fascia 5 cm away from the hernia defect; ports placed too close to the defect will not be of use to secure the mesh. One port must be at least 10 mm to accommodate introduction of the mesh (Fig. 7.3).
Fig. 7.3
Port placement for periumbilical midline hernia
Once all ports are placed, the first step is reduction of the hernia and lysis of adhesions to the anterior abdominal wall. The surgeon should identify any bowel adherent or incarcerated and take special care to use only atraumatic graspers there. Omentum can be grasped with traumatic instruments. Scissor dissection, monopolar cautery, bipolar cautery, and ultrasonic dissection are all appropriate options, but care must be taken when using cautery around the bowel. Clearing away all adhesions widely around the hernia defect is important to allow placement of the mesh (Fig. 7.4).