Hasson 12 mm trocar (1)
5 mm blunt trocar (3)
11 mm blunt trocar (1)
10 mm – 30° scope
Atraumatic laparoscopic graspers
Laparoscopic needle holder
Babcock clamp
L-shaped hook cautery with suction-irrigation capacity
Laparoscopic scissors
Vessel sealing system
Liver retractor
Fast clamp or laparoscopic BookWalter retractor
Penrose drain
0 and 2-0 SurgiDac sutures
56 French esophageal bougie
Laparoscopic clip applier
Technical Steps for Laparoscopic Antireflux Procedure
Placement of Trocars
Five trocars are used for the operation. The initial trocar is placed about 15 cm below the xiphoid process about 1–2 cm to the left of the midline; this port is used for insertion of the scope. The method for first trocar insertion maybe the Hasson technique, direct trocar insertion with or without pneumoperitoneum and will vary depending on patient’s specific characteristics and surgeon’s preference. The second port (5 mm) is placed at the same level as the Hasson between the left midclavicular and the left anterior axillary line; this is the assistant’s port utilized for retraction via Babcock or Penrose drain. The third port (5 mm) is placed at the same level as the previous two ports but in the right midclavicular line or the sub-xiphoid location. It is used for insertion of the diamond liver retractor, the purpose of which is to lift the lateral segment of the left lobe of the liver and expose the esophagogastric junction. The last two trocars (5 mm on the right of the patients and 11 mm on the left) are placed as high as possible under the costal margin and about 5–6 cm to the right and the left of the midline; these ports are used by the operating surgeon for insertion of graspers, energy devices, and for suturing.
Essential Technical Elements of LARS
There are five key technical steps of LARS:
1.
Complete crural dissection with identification and preservation of both anterior and posterior vagus nerve and reduction/excision of hiatal hernia sac if present,
2.
Circumferential dissection of the esophagus and posterior mediastinum to obtain adequate abdominal esophageal length (3 cm),
3.
Crural closure,
4.
Mobilization of gastric fundus with division of short gastric vessels, and
5.
Fundoplication
The last two steps have been source of long debate in the surgical community and while some authors, based on data from RCTs [14], may recommend against routine division of the short gastric vessels, all agree that a form of fundoplication – partial or complete – is a mandatory final step for a successful antireflux procedure.
Dissection of the Esophageal Hiatus and Esophageal Mobilization
The procedure begins with division of the gastrohepatic ligament above the caudate lobe of the liver, where this ligament usually is very thin, and continues toward the diaphragm until the right crus is identified (Fig. 12.1). In 15 % of patients an accessory or replaced left hepatic artery, branching off the left gastric artery, may run in the gastrohepatic ligament altogether with the always present hepatic branch of the vagus nerve. This should be preserved, but if exposure is compromised and the vessel has a small size (indicative that it may be an accessory not a replaced left hepatic artery) it can generally be divided without consequence. The peritoneum and the phrenoesophageal membrane above the esophagus are divided (Fig. 12.2) and the anterior vagus nerve is identified (Fig. 12.3). The Phrenoesophageal fad pad maybe excised and left crus of the diaphragm is exposed (Fig. 12.4).
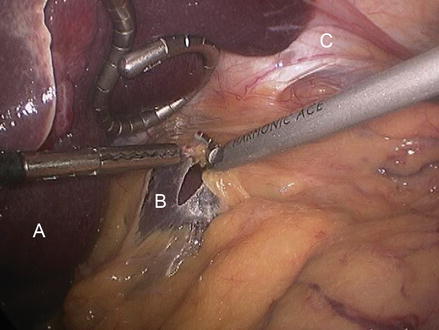
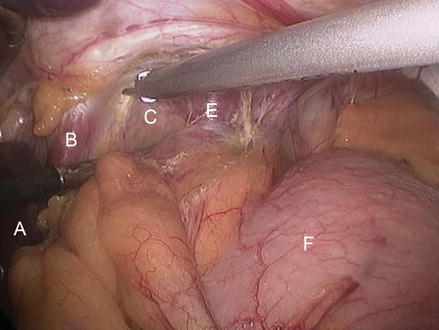
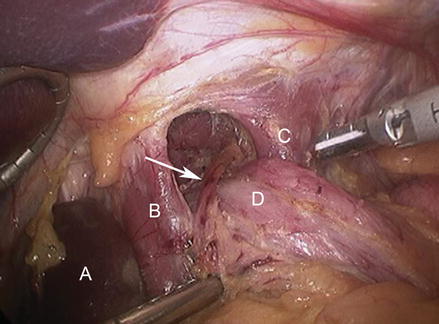
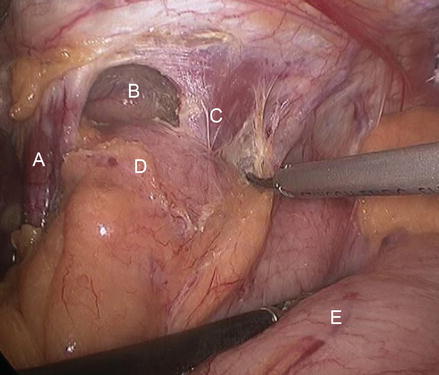
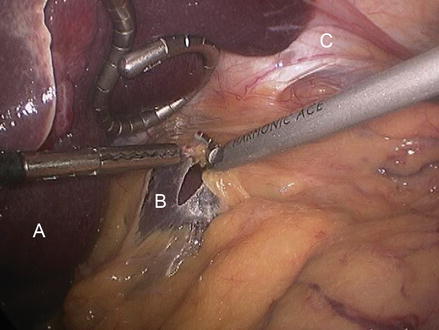
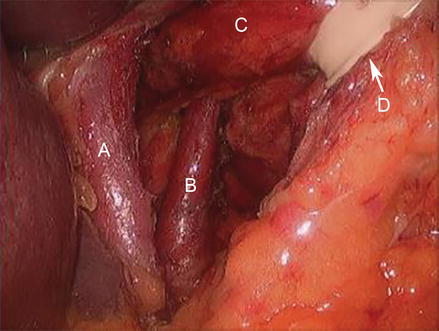
Figure 12.1
Division of the gastrohepatic ligament (A left lobe of the liver, B gastrohepatic ligament, C diaphragm)
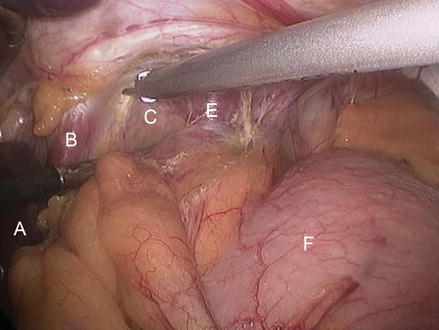
Figure 12.2
Opening of the phrenoesophageal membrane and initial dissection into the posterior mediastinum (A caudate lobe of the liver, B right crus, C. areolar tissue of posterior mediastinum, D divided phrenoesophageal ligament and fat pad E left crus, F gastric fundus)
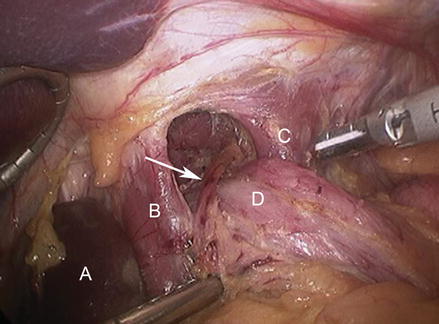
Figure 12.3
The anterior vagus nerve (Arrow) is identified (A caudate lobe of liver, B right crus, C left crus, D esophagus)
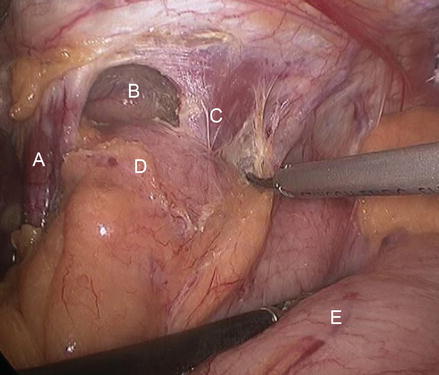
Figure 12.4
Exposure of the left crus and dissection of the angle of his (A. right crus, B posterior mediastinum, C left crus, D gastroesophageal junction (excised phrenoesophageal fat pad), E stomach)
The right crus is then separated from the right side of the esophagus by sharp and blunt dissection (Fig. 12.5), and the posterior vagus nerve is identified. The right crus is dissected inferiorly toward the junction with the left crus (Fig. 12.6). Care should be taken to leave the peritoneal lining on the right crus in preparation for crural closure.
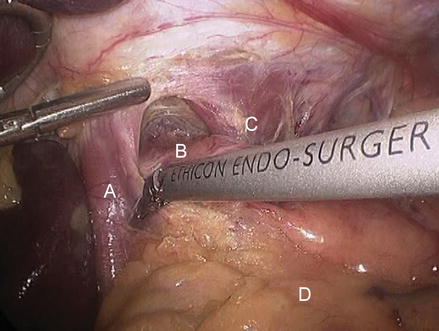
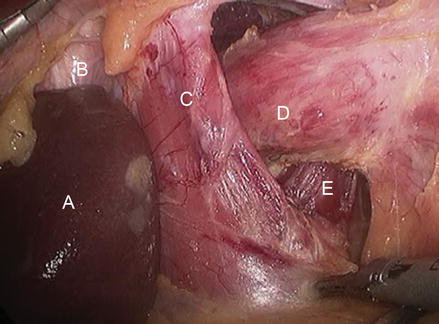
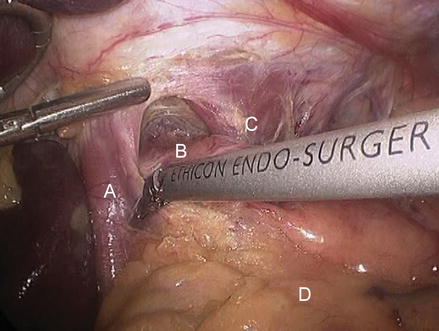
Figure 12.5
Dividing the peritoneum in between the right crus and esophagus (A right crus, B esophagus, C left crus, D stomach)
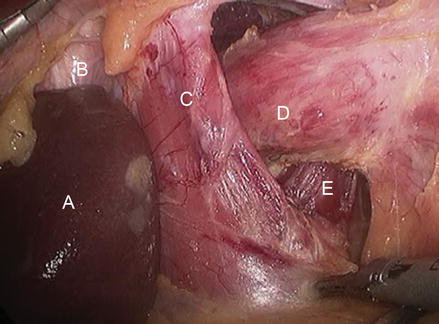
Figure 12.6
Dissecting the right crus inferiorly towards the junction with the left crus (A caudate lobe of liver, B inferior vena cava, C right crus, D esophagus, E left crus)
It is at the beginning of the dissection that care must be taken to identify and excise any potentially present hiatal hernia sac. If present, the sac needs to be reduced in the abdominal cavity and excised in its entirety.
The dissection is continued cranially into the posterior mediastinum to ensure proper mobilization of the distal esophagus which will then translate into adequate abdominal esophageal length.
Tips and Tricks
To avoid the risk of injuring the inferior vena cava or the left gastric artery at the beginning of the dissection, some surgeons use a different method—the so-called left crus approach. In this approach, the operation begins with identification of the left crus of the diaphragm and division of the peritoneum and the phrenoesophageal membrane overlying it. The next step is division of the short gastric vessels, starting midway along the greater curvature of the stomach and continuing upward to join the area of the previous dissection. When the fundus has been thoroughly mobilized, the peritoneum is divided from the left to the right crus, and the right crus is dissected downward to expose the junction of the right and left crura. With this technique, the vena cava is never at risk. In addition, the branches of the anterior vagus nerve and the left gastric artery are less exposed to danger. This technique can be very useful, particularly for management of very large paraesophageal hernias and for re-operative antireflux operations.
Mobilization of Greater Curvature with Division of Short Gastric Vessels
If routine Mobilization of Greater curvature with Division of SGV is contemplated, then at this point the vessel sealer of choice is utilized for this part of the procedure. Dissection begins at the level of the superior portion of the gastric body (Fig. 12.7) and continues upward until the most proximal short gastric vessel is divided (Figs. 12.8 and 12.9). Importantly, all the attachments of the posterior aspect of the gastric fundus to the left crura and the pancreas should also be divided (Fig. 12.10).
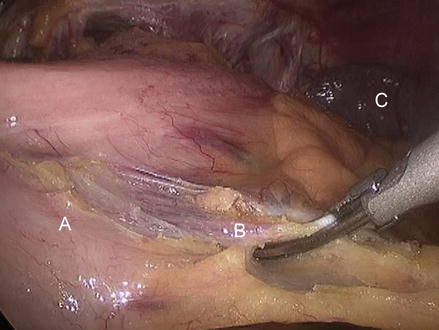
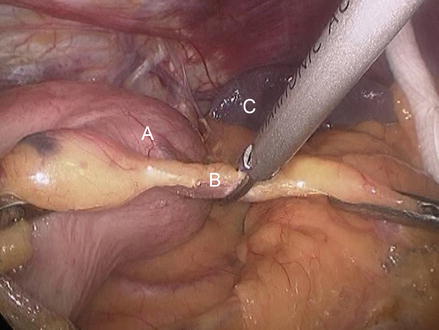
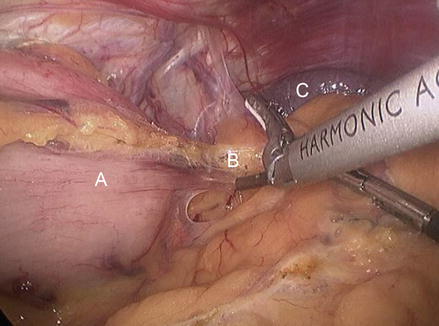
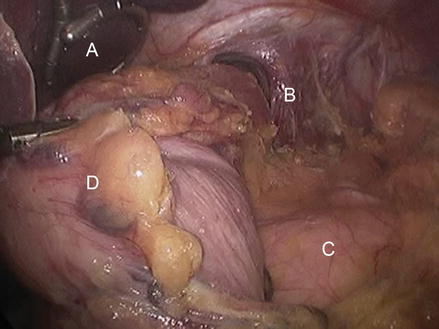
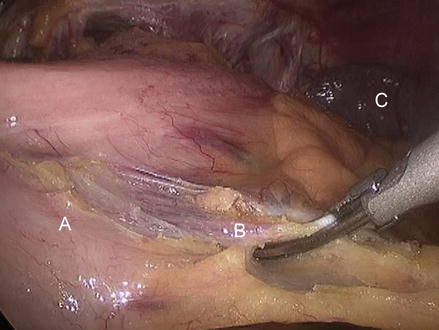
Figure 12.7
Mobilization of greater curvature with division of SGV (A greater curvature of the stomach, B SGV, C spleen)
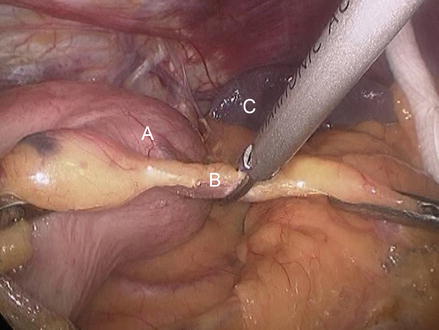
Figure 12.8
Mobilization of greater curvature with division of SGV (A greater curvature of the stomach, B SGV, C spleen)
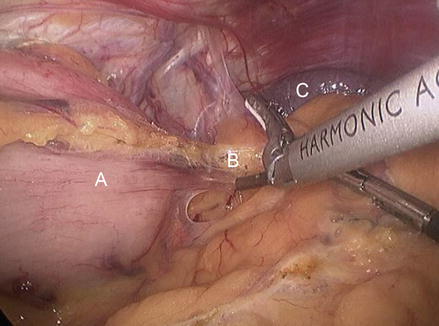
Figure 12.9
Mobilization of greater curvature with division of SGV (A greater curvature of the stomach, B SGV, C spleen)
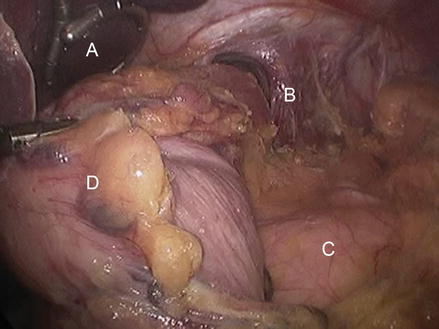
Figure 12.10
Final aspect of complete mobilization of greater curvature with division of SGV (A liver, B left crus, C pancreas, D greater curvature of the stomach)
Care must be taken to avoid bleeding, either from the short gastric vessels or from the spleen, and damage to the gastric wall. Placement of endoscopic clips in the more proximal short gastric vessels before dividing it may be used to prevent bleeding.
Creation of a Large Retroesophageal Window
The esophagus is retracted upward with a Babcock clamp applied at the level of the esophagogastric junction. By blunt and sharp dissection, a window is created under the esophagus between the gastric fundus, the esophagus, and the left pillar of the crus. The window is enlarged and a Penrose drain is passed around the esophagus. This drain is then used for traction instead of the Babcock clamp to reduce the risk of damage to the gastric wall (Fig. 12.11).