Figure 6.1
This figure illustrates the proper decubitus positioning for a laparoscopic transabdominal adrenalectomy. It is very important to ensure that the inferior costal margin is positioned at the “break” in the bed. Used with permission of COACHsurgery.com
Patient positioning is often the hardest and most time consuming part of the operation. Constant communication with the anesthesiologists and staff is critical to prevent mishaps. It is important to place the urinary catheter and to gather all the necessary positioning equipment prior to moving the patient. The patient is placed on a beanbag in the lateral decubitus position with the side of the adrenal tumor up. It is important to place the patient’s costal margin 2–3 cm superior to the point where the bed flexes. Positioning here places the junction of the superior pole of the kidney and the adrenal gland at the break, allowing gravity to auto-retract the kidney inferiorly. The bed should be flexed maximally to increase the space between the costal margin and the hip to create more working space. In addition, a kidney rest should be elevated to further accentuate this space. The beanbag is inflated taking care not to push it into the abdomen, as this will decrease the intra-abdominal working space. Rather the beanbag should be conformed to the patient’s hip and chest to insure secure positioning. The arms are placed in an ergonomically correct position without tension on the shoulder joints, most often separated by pillows rather than with an arm board. All pressure points are adequately padded and an axillary roll is placed. Pillows are placed between the legs in the usual decubitus positioning.
Port Placement (Fig. 6.2a, b)
Figure 6.2
(a) Illustrates the placement of the ports for a laparoscopic transabdominal left adrenalectomy. Often, only 3 ports are used in a left adrenalectomy. Used with permission of COACHsurgery.com. (b) Illustrates the placement of the ports for a laparoscopic transabdominal right adrenalectomy. In this case, the fourth port is used to place a liver retractor. Used with permission of COACHsurgery.com
We typically enter the abdomen via a Veress needle technique at Palmer’s point 2–3 cm inferior to the costal margin at the midclavicular line. On the left side, we place three ports subcostally about 5–10 cm apart, with the lateral-most port in the midaxillary line. On the right side, we typically place four ports in total with the additional port for a liver retractor. When inserting the ports, it is important to enter obliquely svhat the trochars are pointed toward the adrenal gland, otherwise you will have to work against the abdominal wall the entire case. The camera is placed in the middle port and the surgeon works with a two-handed technique.
Procedure
Although some authors advocate identifying and ligating the adrenal vein first, we do not adopt this strategy for the following reasons: (1) identifying the vein can sometimes be difficult early on, especially in obese patients; (2) after ligating the vein in cases of pheochromocytoma, the friable parasitic blood vessels characteristic of that disease dilate and lead to increased bleeding. The key to performing this operation successfully is respecting and exploiting the clear planes between structures – the hook cautery as a very precise means of following these planes. A vessel-sealing device is utilized to coagulate and ligate vessels. The operation is divided into a series of steps popularized by Quan-Yang Duh at UCSF:
1.
Opening the book – Incising the peritoneum and Gerota’s fascia to separate the adrenal gland and peri-adrenal fat from surrounding structures medially
2.
Reading from the top down – Opening the plane between the adrenal gland and peri-adrenal fat and the medial structures starting from the peri-adrenal fat tail superiorly and moving to the adrenal vein or renal hilum
3.
Identifying and ligating the adrenal vein
4.
Separating the adrenal gland from the superior pole of the kidney
5.
Freeing the rest of the peri-adrenal attachments
Left Adrenalectomy
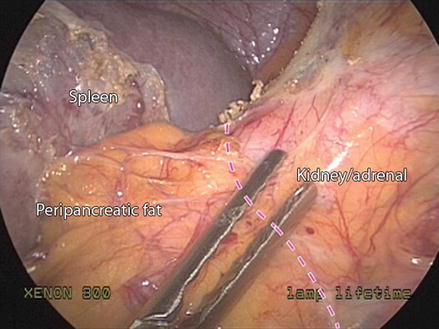
First mobilize the splenic flexure by incising the lienorenal and lienophrenic ligaments to allow the spleen to fall medially with gravity. The dissection continues by using the hook cautery – stay one centimeter off the splenic capsule to prevent tearing the capsule. Incise the ligament at the superior pole of the spleen, at this point it is important to identify and avoid the stomach, which lies just posteriorly. Once the spleen is dissected and reflected medially, the plane between Gerota’s fascia and the pancreas becomes readily identified. Retracting the spleen medially accentuates this plane. In obese patients, a fourth port for lateral retraction of the kidney and adrenal is sometimes helpful. The plane between Gerota’s fascia and the pancreas is carried inferiorly (Fig. 6.3). The splenic flexure often needs to be mobilized as you come to the superior pole of the kidney. Once the plane between spleen and Gerota’s fascia is developed, open Gerota’s fascia superiorly and dissect through the peri-adrenal fat to identify the psoas muscle. Carry this dissection laterally 4–5 cm to allow for lateral and inferior retraction of the adrenal gland as necessary. Then divide the peri-adrenal fat along the medial edge of the adrenal gland and carry this dissection toward the renal hilum. Multiple adrenal arteries will be identified and may be ligated with the electrocautery or vessel-sealing device as suitable. During this dissection the phrenic vein is often encountered and will lead to the adrenal vein (Fig. 6.4). Another rule of thumb is that the splenic vessels “point” to the location of the adrenal vein. The adrenal and phrenic veins are dissected with careful blunt dissection and ligated either with clips or the vessel-sealing device. Once the vessels are divided, identify the plane between the superior pole of the kidney and adrenal gland. When carrying out this dissection, it is important to watch out for a superior pole renal artery and avoid injuring it. The adrenal gland is then separated from the kidney. Then using a combination of blunt and sharp dissection, the adrenal gland is liberated from the psoas muscle and lateral abdominal wall. Hemostasis is obtained with irrigation, aspiration and electrocautery. The specimen is then removed in an impermeable specimen bag through the most anterior trocar. Enlarging the incision may occur for larger specimens. Fascial and skin incisions are closed.