Any wound deeper than a superficial abrasion should be considered for closure to improve the cosmetic result, preserve viable tissue, and restore tensile strength. This can be accomplished with sutures, tissue adhesive, or staples. Tissue adhesive may be indicated for hemostatic wounds in low tension areas that are at low risk for infection. Staples are appropriate for relatively linear lacerations located on the extremities, trunk, or scalp.
The decision about whether and when to repair a laceration is based on many factors, which can be divided broadly into host and wound factors. Host factors include age (elderly patients have 3–4 times higher rate of infection and slower wound healing), malnutrition, and immunocompromise (eg, diabetes mellitus). Wound factors include timing, location, mechanism, and contamination. Bacterial counts begin to increase 3–6 hours post-injury, and every attempt is made to achieve primary wound closure as expeditiously as possible. However, there is no evidenced-based definitive time by which wounds must be closed. Wounds of the face and scalp rarely become infected (1–2%) because the face and scalp have an excellent blood supply; such wounds may be closed safely 24 hours or more after injury. Infection rates of upper (4%) and lower (7%) extremity wounds are higher, and many practitioners use 6–12 hours as a guideline for closing these wounds. Lacerations sustained by a blunt, crushing force produce more local tissue damage and therefore have a higher rate of infection than lacerations caused by a sharp instrument (ie, knife). A puncture wound also has a high rate of infection because bacteria are driven into the tissue and are difficult to remove. Visible contamination within a wound doubles the likelihood of infection. Bite wounds (eg, dog, cat, human) have a very high rate of infection owing to bacterial colonization within the mouth. Generally, bite wounds are not closed primarily unless the wound is gaping or in a cosmetically sensitive area (eg, face).
Staples and tissue adhesive should not be used on deep wounds that would require multiple layered closure. Tissue adhesives should not be used near mucosal surfaces, within the scalp, or over joints (without immobilization), and care must be taken when used near the eyes.
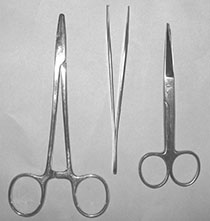
When preparing the wound for closure, the following are needed: povidone-iodine solution, local anesthetic (1% lidocaine with or without 1:100,000 epinephrine), 25- or 27-gauge needle, and a syringe. Irrigation is typically performed with normal saline or sterile water, a 60-mL syringe, and an irrigation shield or 18-gauge angiocatheter; however, some authors have argued that tap water is sufficient for uncomplicated wounds. Similarly, sterile gloves are typically used, although one study did not show a decreased infection rate when sterile gloves were used compared with clean gloves in the repair of clean wounds less than 6 hours old. Instruments needed include a needle driver, tissue forceps (pick-ups), and scissors (Figure 6-1). Use the smallest monofilament suture available that will adequately appose the ends of the laceration, because thinner suture causes less scarring. Usually 4-0 (largest, for torso and extremities) to 6-0 (smallest, for face) will suffice. Antibacterial ointment, gauze, and tape are needed for aftercare.