Frontal view of knee.
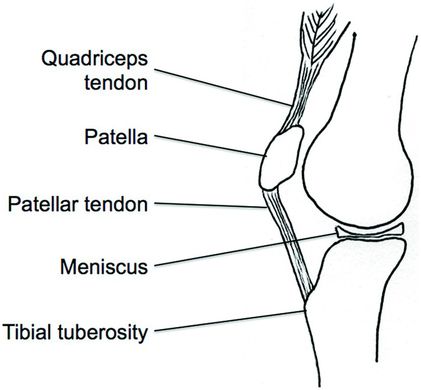
Lateral view of knee.
Focused History and Physical Exam
A focused history in the ED should include:
Injury/trauma: mechanism, pain location, time course, weight-bearing status, presence of mechanical symptoms (locking/catching), instability or giving way, swelling or ecchymosis, paresthesias or weakness.
Prior treatment: medications, physical therapy/rehab ilitation, RICE (rest, ice, compression, elevation).
Prior history: prior injury, surgery, medical history, work history, sports history, family history.
A focused physical exam in the ED should include:
Inspection: gait, alignment, skin, muscular symmetry, soft tissue swelling, effusion, ecchymosis.
Palpation: assess for point tenderness, effusion and increased skin warmth.
Make sure to palpate the medial and lateral femoral condyles and tibial plateaus, quadriceps and inferior patellar tendons, tibial tuberosity, patella, medial and lateral collateral ligaments, and medial and lateral joint lines.
Palpation of joint lines is best performed with the knee in slight flexion.
An effusion may be detected with ballottement or by sweeping the joint space.
Ballottement is performed by applying downward pressure on the patella towards the foot with one hand and then applying pressure on the superior pole of the patella with the other hand.
The test is positive if there is a sensation of bogginess felt while applying pressure on the patella.
Sweeping the joint space is performed by sweeping either the medial or lateral joint space and looking for a fluid wave, or bulge, on the other side.
Range of motion: active and passive range of motion, evaluation for crepitus, patellar tracking
Normal flexion: 130–150°
Normal extension: 0–10°
Special testing: bony, muscular, ligament, meniscus
ACL
Lachman test (most sensitive) (Figure 6.3)
May be difficult to perform in the acute setting, and is operator dependent.
Patient supine, knee flexed 20–30°, stabilize distal femur with one hand, apply anterior force to proximal tibia with other hand.
The test is positive if there is subluxation of tibia anteriorly with no firm endpoint.
Pivot shift test (highest positive predictive value, but only in a patient without guarding)
Patient supine, knee fully extended, internally rotate foot and tibia, apply mild valgus stress while flexing knee.
The test is positive if the tibia subluxates anteriorly at around 30° of knee flexion.
Anterior drawer test (Figure 6.4)
Patient supine, knee flexed to 90°, stabilize foot in neutral position on the table, apply anterior force to the proximal tibia with thumbs placed along the joint line on either side of the patellar tendon.
The test is positive if there is subluxation of tibia anteriorly.
PCL
Posterior drawer test (Figure 6.4)
Patient supine, knee flexed to 90°, foot stabilized on the table, thumbs placed along the joint line on either side of the patellar tendon, posterior force applied to the proximal tibia.
The test is positive if there is posterior subluxation of the tibia.
Posterior sag test
Patient supine, knees and hips flexed to 90°
The test is positive if there is a sagging or translation of tibia posteriorly.
Dial test
Assesses for both injury to the posterolateral corner structure (PLC) and PCL.
Patient supine, foot/tibia over side of table, femur stabilized on table, passive rotation of the tibia laterally at both 30 and 90°, compare to opposite side.
Look for asymmetry compared to uninjured leg at both 30 and 90°:
MCL
Valgus stress test (Figure 6.5):
Apply valgus pressure to knee while stabilizing the ankle
Test with knee in 0 and 30° flexion and compare to opposite side, knee in 30° of flexion isolates superficial MCL.
Test is positive if there is pain and/or opening of the medial joint space.
LCL
Varus stress test (Figure 6.6)
Apply varus pressure to knee while stabilizing the ankle.
Test with knee in 0 and 30° flexion, and compare to opposite side, knee in 30° of flexion isolates LCL.
Test is positive if there is pain and/or opening of the lateral joint space.
PLCS
Dial test: see in the earlier section under PCL injury
Menisci
McMurray test (Figures 6.7 and 6.8)
Patient supine, one hand holding patient’s heel, other hand on the patient’s joint line, maximally flex knee, apply external tibial rotation (medial meniscus) or internal tibial rotation (lateral meniscus), and bring knee into full extension while maintaining rotation.
The test is positive if there is a painful pop/click over the appropriate joint line.
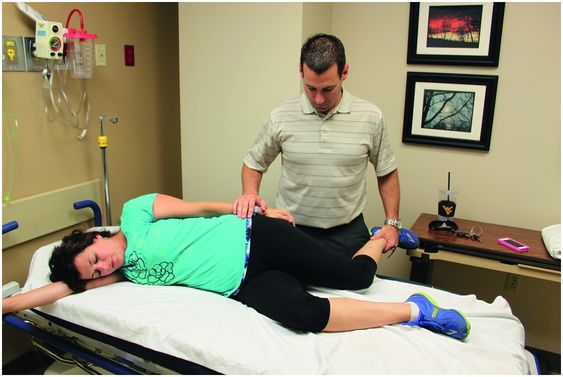
Apley compression test
Patient prone, knee flexed to 90°, apply downward axial load to tibia with internal (lateral meniscus) or external (medial meniscus) rotation.
The test is positive if there is a painful pop/click over the affected joint line.
Patellofemoral pain syndrome
Grind test
Retropatellar pain with compression of the articular patellofemoral surfaces during quadriceps contraction.
Retropatellar pain with half or full-squat
ITB friction syndrome
Ober’s test (Figure 6.9)
This test is used to evaluate for ITB tightness.
Patient lying on side with symptomatic side up, knee resting on the exam table is flexed 45°, pelvis is at 90° to exam table and stabilized with examiner’s hand, other arm supports the affected knee and then brings hip from flexion/abduction into extension/adduction, allow hip to passively adduct.
The test is positive if the leg does not adduct past parallel.
Noble compression test
Hip and knee passively flexed to 90°, apply pressure with thumb over ITB proximal to lateral femoral condyle, patient actively extends hip and knee
The test is positive if there is pain over distal ITB (just proximal to lateral femoral condyle) at 30° of extension.
Extensor mechanism (Figure 6.10)
Used to evaluate the integrity of the entire extensor mechanism of the knee including quadriceps, quadriceps tendon, and patellar tendon.
While keeping the leg extended at knee, the patient attempts to actively raise their straight leg off the exam table.
Inability to actively raise a straightened leg off the exam table is an indication that there has been a disruption of the extensor mechanism.
Patellar apprehension test (Figure 6.11)
Used to assess for instability of patella after a patellar dislocation.
While the patient is supine, the examiner places lateral pressure on the patella while flexing the knee; test is positive if the patient contracts quadriceps, resists further attempts at manipulation of the knee, and has the same sensation of patellar instability as at the initial dislocation.
Neurovascular exam: sensation, strength, reflexes (patellar, Achilles), pulses (popliteal, dorsalis pedis, posterior tibialis), and capillary refill
Nerve distribution:
Common peroneal nerve
Motor innervation for ankle dorsiflexion and great toe extension, sensation to web space between first and second toes and lateral leg
Saphenous nerve
Sensation to anteromedial aspect of the leg and foot
Tibial nerve
Sensation to posterolateral leg, lateral foot, sole of foot, and motor innervation to posterior compartment of the leg including plantarflexion, toe flexion, and weak inversion
Skin exam
Check for color, warmth, erythema, or ecchymosis

Lachman test.

Correct positioning of hands to perform anterior and posterior drawer tests.

Valgus stress test.

Varus stress test.

McMurray test for medial meniscus.

McMurray test for lateral meniscus.
Ober’s test.

Test for integrity of extensor mechanism.

Patellar apprehension test.
Differential Diagnosis – Emergent and Common Diagnoses
Patellar Fracture
General Description
Patella is the largest sesamoid bone.
Patella increases leverage and efficiency of the quadriceps muscle.
Typically triangular, apex pointing distally
Rectus femoris and vastus muscles insert on proximal pole.
Patellar ligament attaches to distal pole of patella, inserts on tibial tuberosity.
Quadriceps tendon passes over patella, joins patellar ligament distally.
Fracture classified by fracture pattern or location.
Location: lower, middle, or upper pole
Pattern: transverse, stellate or comminuted, vertical, and osteochondral
May be displaced or nondisplaced.
Normal variants that may be mistaken for a fracture
Bipartite patella
Persistence of an accessory ossification center that fails to fuse in childhood
May involve inferior, lateral, or superolateral (most common) margin
Usually asymptomatic and able to differentiate from patellar fracture by history and physical exam
This is best seen on AP view
Has well-defined zone of separation
View of opposite knee usually confirms this diagnosis, as bipartite patella may be bilateral
Fabella
Small sesamoid bone in the tendons posterior to knee joint
Best seen on lateral view
| Emergent Diagnoses | Common Diagnoses |
|---|---|
| Patellar fracture | ACL injury |
| Patellar dislocation | MCL injury |
| Extensor mechanism disruption | Meniscus injury |
| Proximal tibiofibular joint dislocation | Patellar tendinopathy |
| Total knee dislocation | Patellofemoral pain syndrome |
| Tibial plateau fracture | Popliteal cyst |
| Pre-patellar septic bursitis | Osteoarthritis |
| Septic arthritis | |
| Pediatric physis injury |
Mechanism
May be caused by direct or indirect forces
Direct forces include fall onto anterior knee or striking knee on dashboard.
Typical fracture pattern is stellate and nondisplaced
Indirect forces include forceful quadriceps muscle contraction usually in an attempt to prevent a fall.
This force may exceed the intrinsic strength of the patella leading to fracture.
With repeated quadriceps contraction there is tearing of the medial and lateral retinacula resulting in displacement.
Typical fracture pattern is transverse and displaced.
Presentation
Pain and swelling over anterior knee after injury
Inability to fully extend the knee
Physical Exam
Tenderness and soft tissue swelling over patella
Effusion likely
Displaced fracture may have palpable defect or separation if swelling not excessive
Evaluate for disruption of the extensor mechanism (Figure 6.10)
Essential Diagnostics
Obtain an x-ray of the knee including AP, lateral, oblique, and sunrise views
Lateral view is most useful in delineating fracture lines and determining displacement, especially for transverse fractures
Separation of more than 3 mm between fragments or articular step-off more than 2 mm constitutes a displaced fracture
Marginal vertical fractures best seen on sunrise views
ED Treatment
Ice, compression, elevation to decrease swelling
Nondisplaced fractures with intact extensor mechanism may be placed in a knee immobilizer in full extension and allowed to weight bear as tolerated.
Orthopedic surgery consult indicated for displaced, open, or severely comminuted fractures, or any patella fracture with a disrupted extensor mechanism.
Disposition
Nondisplaced patellar fractures with extensor mechanism intact may be discharged.
Patient should be instructed to follow-up with sports medicine or orthopedic surgery within five to seven days.
Return to work
May return as tolerated based upon requirements.
Sedentary jobs: may return after a few days of rest, ice, compression, elevation, though consider waiting until after first follow-up appointment (five to seven days).
Jobs requiring knee flexion: even climbing stairs, should not return until cast or brace is discontinued and range of motion has progressed to allow for ability to perform these activities with reasonable comfort, which is typically six to eight weeks.
Return to sport
May begin activities requiring little knee flexion soon after immobilization.
Begin straight leg raises, and ankle range of motion while in immobilizer.
No clearance for return until fracture has healed, typically six to eight weeks, with no pain and normal strength and range of motion.
Displaced, severely comminuted, or open patellar fractures should be admitted for surgical repair by orthopedic surgery.
Complications
Infection
Loss of reduction or failure of internal fixation
Avascular necrosis
Delayed union, nonunion, malunion
Chondromalacia
Osteoarthritis
Stiffness and weakness
Extensor mechanism disruption
Pediatric Considerations
Patella ossifies in early childhood, first visible on radiographs between ages 3 and 6.
Up to six ossification centers, correlate with clinical exam for tenderness and obtain comparison view of normal knee.
Unlike adults, knee effusions are rarely due to ligamentous injury.
Patellar dislocation or fracture is much more likely.
MRI or arthroscopy may be required for adequate evaluation because fracture may primarily involve cartilage.
Most patellar fractures in children are osteochondral or avulsion injuries.
Osteochondral fractures usually result from patellar dislocations, occurring in about 10 percent of dislocations.
Patellar sleeve fractures
Usually results from high-impact jumping activity.
Type of osteochondral avulsion fracture of the patella.
Patellar avulsion fracture, which includes a large amount of articular cartilage and retinaculum.
Will often see a high-riding patella on lateral knee x-ray.
Orthopedic consult is indicated for children with patella sleeve fractures, displaced avulsion fractures, or avulsion fractures complicated by inability to fully extend the knee.
Obtain MRI in a child if there is concern for disruption of the extensor mechanism.
Pearls and Pitfalls
Always make sure to check integrity of the extensor mechanism.
Beware of what appear to be small patella avulsion fractures in pediatric patients because they often represent a much larger injury.
Patellar Dislocation
General Description
Typically underlying patellofemoral malalignment.
Factors that increase risk of subluxation or dislocation include shallow femoral groove, hypoplasia of lateral femoral condyle, small or high-riding patella, genu valgum, external tibial torsion, atrophy of vastus medialis muscle.
Nearly all occur laterally
Mechanism
Several mechanisms may result in patellar dislocation:
External pivotal motion on partially flexed knee followed by a forceful contraction of the quadriceps that pulls the patella laterally.
Sudden cutting motion or sudden contraction of quadriceps during deceleration.
Direct blow to medial patella forcing it laterally.
Spontaneous reduction, knee went out of place and slipped back after extension of the knee.
Presentation
Acute knee pain and swelling after injury.
Patient will often report that they felt or heard “a pop.”
Patient may not present with an obvious deformity if the patella has spontaneously reduced prior to ED presentation.
Physical Exam
If there is an obvious deformity, the patella is typically laterally displaced.
Patient will often have an effusion.
Tenderness over medial retinaculum and lateral femoral condyle.
Positive apprehension test (Figure 6.11).
Assess integrity of extensor mechanism (Figure 6.10).
Essential Diagnostics
Knee x-rays should include AP, lateral, oblique, and sunrise views.
Pre- and post-reduction x-rays to rule out accompanying fracture, even if spontaneous reduction.
Pay particular attention to the medial edge of the patella to evaluate for osteochondral fracture.
ED Treatment
Any patient with a laterally displaced patella will need reduction.
Patient should be placed in either a supine or seated position.
Hip is flexed to decrease tension on the quadriceps.
Gradually extend the knee while gently pushing patella medially.
The same technique is used for a medially displaced patella, except apply an anterolateral force to the patella.
Ice, compression, elevation to decrease swelling.
Place patient in a knee immobilizer to limit knee flexion.
May weight bear as tolerated.
Crutches as needed for ambulation.
Disposition
Most patellar dislocations may be discharged as long as they are successfully reduced and there is no associated fracture.
Follow-up may be with either sports medicine or orthopedic surgery within seven days.
Initial patella dislocations are usually managed conservatively with bracing and functional strengthening and conditioning.
Recurrent dislocations may need operative stabilization of patella.
Return to work or school based on job requirements, as the patient is able.
Rehabilitation
Early isometric quadriceps exercises to maintain strength.
Early range of motion exercises when pain and swelling decreased (usually seven to ten days).
Resistance exercises of quadriceps once full range of motion is achieved.
Return to sport after full, pain-free range of motion, full strength, and sport-specific agility progression program.
Complications
Recurrent dislocation
Degenerative arthritis
Osteochondral fracture
Osteoarthritis
Pediatric Considerations
Unlike adults, knee effusions are rarely due to ligamentous injury.
Patellar dislocation or fracture is much more likely.
Recommend orthopedic surgery consultation if there is an associated osteochondral fracture.
Obtain MRI if x-rays are normal but child is unable to perform a straight leg raise.
Pearls and Pitfalls
Lateral patella dislocation is most common.
Consider this diagnosis in any patient with suggestive history even if the patella is not displaced on exam as the patella may have spontaneously reduced prior to presentation.
Reduction is generally safe and simple.
Obtain x-rays to look for osteochondral fractures.
Check integrity of extensor mechanism
Disruption of the Extensor Mechanism
General Description
Disruption of the extensor mechanism of the knee includes quadriceps tendon rupture, patellar tendon rupture, tibial tubercle avulsion fracture.
Quadriceps tendon rupture typically occurs in patients greater than 40 years old at bone-tendon junction, and is more common than patellar tendon rupture.
Patellar tendon rupture typically occurs in patients less than 40 years old, and is most common at inferior pole of patella.
Tibial tubercle avulsion fractures occur most commonly in pediatric patients.
Tendon rupture may be partial or complete.
Risk factors include: systemic inflammatory disease, chronic renal disease, diabetes, tendinopathy, corticosteroid injection, anabolic steroids, chronic degeneration, history of prior ACL repair using patellar tendon autograft.
Mechanism
Several mechanisms may lead to disruption of the extensor mechanism:
Sudden, forceful contraction of quadriceps during vertical or horizontal deceleration, that is, jumping sports.
Direct trauma to anterior knee, especially in younger patients.
Patellar tendon rupture usually occurs due to a tensile overload of the extensor mechanism.
Most occur with knee in flexed position, greater than 60°.
Increased risk if history of patellar tendon allograft for repair of prior ACL injury.
Quadriceps tendon rupture usually occurs due to an eccentric contraction of the quadriceps muscle.
Most often occurs with the foot planted and the knee slightly bent.
Presentation
A “pop” may have been heard during injury.
Difficulty weight-bearing
Patellar tendon rupture: infrapatellar pain
Quadriceps tendon rupture: suprapatellar pain
Physical Exam
Effusion
Tenderness over injured tendon
May be able to palpate defect.
A gap may be present below inferior pole of patella in patellar tendon disruption.
A gap may be present superior to patella in quadriceps tendon rupture.
Loss of extension
A partial tendon injury does not extend into retinaculum, and patient may be able to extend against gravity.
May, however, still have an extensor lag.
A full-thickness tendon injury will result in the patient being unable to perform an active straight leg raise or maintain a passively extended knee (Figure 6.10).
Essential Diagnostics
X-ray views should include AP, lateral, oblique, and sunrise views.
The AP and lateral views are the best views to assess patella height and position, as well as possible associated fracture pattern.
The Insall–Salvati ratio may be used to assess patellar height.
This is the ratio of length of patella to length of patellar tendon.
Measured on lateral x-ray with knee flexed 30°.
Normal ratio is 1:1
Consider patella alta, which may be an indication of patellar tendon rupture, if ratio is less than 0.8.
Consider patella baja, which may be an indication of quadriceps tendon rupture, if ratio is greater than 1.2.
The sunrise view may be used to further delineate fracture displacement and osteochondral defects.
Ultrasound may be used to look for tendon continuity.
ED Treatment
Knee should be placed in a knee immobilizer in extension.
Consult orthopedic surgery for tibial tubercle avulsion fractures or complete tendon ruptures.
Complete tendon ruptures need urgent repair or reconstruction and are most successful if performed within fourteen days from initial injury.
Partial tendon ruptures with intact extensor mechanism may be placed in a knee immobilizer in full extension, allowed to weight bear as tolerated, and may begin early range of motion.
Disposition
Patients with complete tendon ruptures will likely require admission or urgent orthopedic surgery follow-up for surgical repair or reconstruction.
Patients with partial tendon ruptures may be discharged home.
Patients should follow-up with sports medicine or orthopedics within seven days for repeat evaluation.
Return to work or sports depends on degree of tear and operative management
Patients may return to sport after partial tears when they are pain free and have regained full range of motion and normal strength.
Patients with full tears who require operative treatment may generally return to sport in nine to twelve months after repair and completion of a rehabilitation program.
Complications
Re-rupture
Persistent quadriceps atrophy and weakness
Loss of motion/stiffness
Functional impairment
Pediatric Considerations
It is important to evaluate pediatric patients for tibial tubercle avulsion fracture if they present with a disruption in their extensor mechanism.
This is an avulsion fracture of tibial tuberosity, Salter–Harris type III of proximal tibial physis.
May present with either complete or partial disruption of the extensor mechanism.
Best seen on lateral view with patella alta depending on displacement of tuberosity.
Consider in adolescents.
Often occurs during jumping.
May be confused with Osgood–Schlatter disease, which has more insidious onset.
Compartment syndrome may be a complication.
Orthopedic surgery should be consulted in all cases as surgical repair may be required.
Pearls and Pitfalls
Always evaluate the integrity of the extensor mechanism after acute knee injuries.
When there is a deficit in the extensor mechanism, be sure to consider quadriceps tendon ruptures, especially in patients greater than 40 years old, patellar tendon ruptures in patients less than 40 years old, and tibial tubercle avulsion injury in adolescents.
ACL Injury
General Description
Origin at posteromedial aspect of intercondylar notch of lateral femoral condyle.
Insertion in front of intercondylar eminence of tibia and medial to anterior horn of lateral meniscus.
Functions as the primary restraint of anterior translation of tibia on femur.
Secondary restraint to internal rotation of the tibia when knee is in full extension.
Associated with meniscal injury, lateral meniscus tear more common with ACL injury.
The classic unhappy triad consists of ACL tear and medial meniscus and MCL injury.
Mechanism
Usually low-energy, noncontact injury that occurs with deceleration, hyperextension, or rotational force at the knee.
Presentation
Patient may have noticed a “pop.”
May have been unable to bear weight initially.
Swelling usually occurs within hours.
Often complain of a sensation of giving way or instability.
Physical Exam
Effusion usually present
Often presents with large effusion, but on occasion may have little to no effusion, especially in younger patients.
Guards or limits active extension of knee to avoid activation of the quadriceps muscle which may cause pain and/or symptoms of instability.
Lachman (Figure 6.3), anterior drawer (Figure 6.4), and pivot shift tests are often positive.
These tests may be falsely negative in patients with significant pain and guarding after acute injury.
Essential Diagnostics
Knee x-rays should include AP, oblique, and lateral views to exclude underlying bony injury.
Usually only show indirect evidence of ACL tear, but often normal.
Effusion may be visible.
May have bony avulsion of anterior tibial intercondylar eminence.
May have a Segond fracture, which is an avulsion fracture of lateral aspect of tibial condyle and pathognomonic for ACL injury.
MRI often used to confirm ACL injury, and look for associated injuries such as meniscal tear or osteochondral lesions.
This is not needed emergently in the ED and may be performed as an outpatient.
ED Treatment
Ice, compression, elevation to decrease swelling.
Activity modification, rest
Crutches if needed for ambulation, weight bear as tolerated.
Knee immobilizer only if instability symptoms for short period of time (i.e., seven to ten days).
Prolonged immobilization may complicate rehabilitation.
Disposition
Almost all ACL injuries may be discharged from the ED.
Emergent orthopedic consult is not indicated.
Patients may follow-up as an outpatient with orthopedic surgery or sports medicine.
Reconstruction is indicated for most, but usually delayed three to six weeks post injury.
Patients may return to work or school as tolerated based on job requirements.
Patients may return to play after reconstruction following normalization of range of motion and strength and progression of sport-specific activities without pain or instability, usually after six to nine months.
Complications
Chronic instability, especially if not surgically repaired
Multiligamentous injury
Meniscal injury
Loss of motion/muscle weakness
Osteoarthritis
Pediatric Considerations
Strongly consider surgery for ACL tear, as activity limitation not realistic in children.
Consider tibial spine fracture in late childhood to mid-adolescence.
Consider with mechanism that would cause ACL injury in adults.
Usually associated with bicycling after a foot gets caught in spokes of the wheel.
May also occur after hyperextension of knee during a fall.
Nondisplaced fracture in long-leg cast for five to six weeks, with knee in 5–10° of flexion.
Consult orthopedics if there is a displaced fracture.
Pearls and Pitfalls
Lachman, anterior drawer, and pivot shift tests are used to diagnose ACL tears, however may be falsely negative acutely and are operator dependent.
Knee immobilizers are only indicated for patients with symptoms of instability and should only be used for a short period of time (seven to ten days).
Often associated with other injuries, such as meniscal tears.
PCL Injury
General description
Origin at anterolateral aspect of medial femoral condyle.
Inserts on posterior tibia, below the articular surface.
It functions as the primary restraint of posterior translation of tibia and secondary restraint of external rotation of tibia.
May be associated with other injuries
Consider PLC when associated injuries occur, that is, common peroneal nerve or vascular injury.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








