Key Clinical Questions
How are catheter-related infections diagnosed?
What are the potential complications of catheter-related infection?
What is the appropriate management of catheter-related infection?
When is it appropriate to attempt salvage of an infected intravascular catheter?
How can catheter-related infection be prevented?
Epidemiology
Indwelling vascular catheters are the most common cause of nosocomial bloodstream infections. They are particularly common among critically ill patients, hemodialysis-dependent patients, and persons receiving chemotherapy or total parenteral nutrition. In the United States, approximately 80,000 central venous catheter (CVC)-related bloodstream infections occur each year in intensive care units (ICUs). These infections prolong hospitalization by 7.5 to 22 days, cost in excess of $20,000 per episode, and have an attributable mortality of 11.5% to 35%.
Staphylococci, including Staphylococcus epidermidis and Staphylococcus aureus, cause more than two-thirds to 90% of all catheter-related bloodstream infections (CRBSIs). Other infecting organisms include enteric gram-negative rods, Pseudomonas aeruginosa, and Candida species. Less common pathogens include Serratia marcescens, Enterobacter species, Burkholderia cepacia complex, and Citrobacter freundii.
Pathophysiology
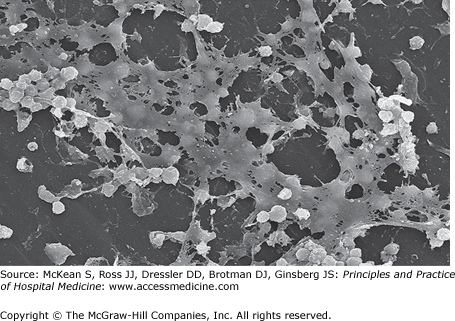
Infections of vascular catheters arise from bacterial biofilm, comprised of bacteria embedded within an extracellular polysaccharide matrix on the catheter surface (Figure 196-1). Bacterial biofilm may develop as early as 24 hours after catheter placement. As shown by electron microscopy, biofilm forms on the external surface of short-term catheters that have been in place for < 10 days, and may be found on the luminal surface of long-term catheters that have been in place for ≥ 10 days.
The first step in biofilm formation is the binding of free-floating, or planktonic, organisms to the catheter surface by cell wall–associated adhesins. This is facilitated by the formation of a film of host fibrin and fibronectin on the catheter surface. Other factors favoring attachment include hydrophobic and electrostatic forces, cell surface structures such as pili or fimbriae, platelet binding, and shear stress from the fluid environment. Attached organisms multiply to form microcolonies and secrete an extracellular polysaccharide matrix that forms the architectural structure of the biofilm. Bacteria embedded in biofilm typically have a lower metabolic rate, making them less susceptible to the effects of antibiotics; the minimal inhibitory concentrations of microorganisms in biofilm can be up to 1000-fold higher than for planktonic organisms. Additionally, antibiotics have difficulty penetrating biofilm. This explains why biofilm-based infections are difficult to eradicate without removal of the infected device.
Catheter infection may arise by several routes. The external catheter may become colonized by skin flora during insertion, or subsequent migration of skin organisms along the catheter surface. Luminal colonization occurs when microorganisms are introduced through the hub of the catheter. The risk of luminal infection increases with more frequent manipulation of the hub. Hematogenous seeding of the catheter may occur during bloodstream infection from another source. Uncommonly, contamination of intravenously administered fluids or drugs can cause CRBSI, sometimes leading to outbreaks. Table 196-1 lists factors associated with development of CRBSIs.
|
How Is Catheter-Related Infection Diagnosed?
The clinician must accurately make a diagnosis of catheter-related infection to appropriately treat the patient and reduce the rate of unnecessary procedures. The most common presenting manifestation of catheter-related infection is fever. Erythema and purulence at the catheter site are only present in a minority of patients. Sicker patients may have hypotension and tachycardia. Leukocytosis is usually present. Diagnosis can be established by various methods for culturing the removed catheter or blood cultures with an in situ catheter.
Diagnostic techniques that do not require catheter removal are not widely used. Quantitative blood cultures allow a comparison of the number of microorganisms in blood collected simultaneously via the lumen of the catheter and from a peripheral vein. A central-to-peripheral blood culture colony count ratio of 5 to 10:1 is indicative of CRBSI. Although this technique is useful in predicting CRBSIs, it is not routinely performed in most hospitals. A single bacterial count of > 100 colony-forming units (CFU)/mL in the catheter blood specimen is also suggestive of CRBSI, in the presence of a positive peripheral blood culture.
Differential time to positivity (DTP) compares the time it takes for a blood culture to become positive when drawn from the catheter versus peripheral blood. The underlying assumption is that blood drawn via the lumen of an infected catheter will have higher number of bacterial colonies than that obtained from a peripheral blood draw, and thus will become positive earlier. When catheter cultures become positive ≥ 2 hours earlier than peripheral blood, DTP is quite sensitive for the diagnosis of CRBSI. The specificity of DTP is dramatically reduced in patients receiving antibiotics at the time cultures were drawn. Most hospitals have automated blood culture machines, making information on time to positivity readily available in the microbiology laboratory.
Endoluminal brushing of the catheter while still in place and subsequent culture is very sensitive for the diagnosis of catheter-related infection in patients with peripheral bacteremia. However, adverse events such as cardiac arrhythmias, embolization, and subsequent bacteremia have been reported.
The most commonly employed method in clinical microbiology laboratories is semiquantitative culture of the catheter tip, the so-called roll-plate method. This technique consists of rolling the distal 4 cm of the catheter tip on an agar plate for culture. A yield of ≥ 15 CFU of bacteria distinguishes catheter colonization from infection. A major limitation is that only microorganisms from the external surface of the catheter are cultured, potentially underdiagnosing catheters with primarily intraluminal infection. Rapid diagnosis of CRBSI may also be achieved by direct microscopic examination of the catheter tip stained with Gram stain or acridine orange.
A more sensitive technique involves sonication of the catheter tip to dislodge biofilm-embedded organisms, with culture of the resultant sonicate. This technique is much more sensitive than the roll-plate method, with a cutoff limit for infection of ≥ 102 to 103 CFU/catheter segment. This culturing technique retrieves organisms from both the external and internal surfaces of the catheter. A technique for the rapid diagnosis of CRBSI is direct microscopic examination of the catheter tip stained with Gram stain or acridine orange. Table 196-2 shows the relative sensitivity and specificity of the methods outlined above.
| Accuracy | ||||
|---|---|---|---|---|
| Diagnostic Criteria | Sensitivity | Specificity | Disadvantages | |
| Techniques without CVC removal | ||||
| Simultaneous quantitative blood cultures | Quantitative blood culture drawn through CVC yields CFU count five-fold higher or more than CFU count from simultaneously drawn blood from peripheral vein | 93% | 97–100% | Labour intensive, costly |
| Differential time to positivity | Blood culture drawn from CVC becomes positive ≥ 2 h before simultaneously drawn blood culture from peripheral vein | 89–90% | 72–87% | Hard to interpret when patient is taking antibiotics through the CVC |
| CVC-drawn quantitative blood culture | Quantitative blood culture from CVC is ≥ 100 CFU/mL | 81–86% | 85–96% | Cannot differentiate between CRBSI and high-grade bacteraemia |
| Acridine orange leucocyte cytospin | Presence of any bacteria | 87% (96% if followed by Gram stain) | 94% (92% if followed by Gram stain) | Not widely tested or used |
| Endoluminal brush | Quantitative culture with > 100 CFU/mL | 95% | 84% | May induce bacteraemia, arrhythmia, embolisation |
| Techniques requiring CVC removal | ||||
| Semiquantitative CVC tip culture, roll plate | ≥ 15 CFU/mL from CVC tip | 45–84% | 85% | Unable to culture organisms embedded intraluminally |
| Quantitative CVC culture: centrifugation, vortexing, sonication | ≥ 103 CFU from CVC tip | 82–83% | 89–97% | The cut-off point of ≥ 103 CFU vs ≥ 102 CFU is not well defined |
| Microscopy of stained CVC: Gram stain and acridine orange staining | Direct visualisation of the microorganisms | 84–100% | 97–100% | Labour intensive, impractical |
What Are Potential Complications of Catheter-Related Infection?
Complicated bacteremia should be suspected in patients with persistent bacteremia or fever. Potential complications of CRBSIs include infective endocarditis, septic thrombophlebitis, osteomyelitis, septic arthritis, meningitis, epidural abscess, metastatic abscess, catheter or venous thrombosis, prosthesis infection, various embolic phenomenon, and septic shock.
S aureus bacteremia is associated with an especially high risk of complications, ranging from 25% to 43%. In one study, the strongest predictor of complicated bacteremia was a positive follow-up blood culture result at 48 to 96 hours. A scoring system based on the presence or absence of four risk factors (community acquisition, skin examination findings suggesting acute systemic infection, persistent fever at 72 hours, and positive follow-up blood culture results at 48–96 hours) accurately identified complicated S aureus bacteremia.
Another study evaluated all cases of CVC-related S aureus bacteremia in order to determine host and pathogen factors that were associated with hematogenous complications. On multivariable analysis, symptom duration, hemodialysis dependence, presence of a long-term intravascular catheter or a noncatheter device, and infection with methicillin-resistant S aureus (MRSA) were significantly associated with complications. Thus, at least in patients with S aureus CRBSI, the above mentioned factors should prompt providers to remove the infected catheter.
Vascular catheter infections can be associated with thrombosis and septic thrombophlebitis. This may be manifested by evidence of peripheral emboli distal to the site of catheter insertion, or swelling in an extremity. In one study, thrombosis was a common complication of CVC-associated S aureus bacteremia (71%), with poor sensitivity of physical examination findings.
Many cases of infective endocarditis are not suspected clinically and therefore are not detected. Studies using transesophageal echocardiogram (TEE) to identify endocarditis in patients with S aureus bacteremia have shown high rates of valvular vegetations (25–32%). TEE is more sensitive than transthoracic echocardiogram, and is most sensitive when performed five to seven days after the onset of bacteremia. Clinically, endocarditis is seen in 17% to 20% of cases of S aureus bacteremia. In general, patients with S aureus bacteremia have a high 90-day mortality rate of 25% to 30%.
TEE should be considered in patients with CRBSI who have any of the following: a prosthetic heart valve, pacemaker, or implantable defibrillator; persistent bacteremia or fungemia, or fever more than three days after initiation of appropriate antibiotic therapy and catheter removal, as well as any case of S aureus
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree