Introduction
Chronic non-cancer pain is a common clinical condition afflicting many people, with a significant proportion of them experiencing some form of functional disability (Chapter 1). When pharmacological therapy or conventional surgery fails to control pain adequately or when patients have intolerable side effects to drug treatment, the role of invasive interventional procedures may remain an option for the treatment of chronic pain.
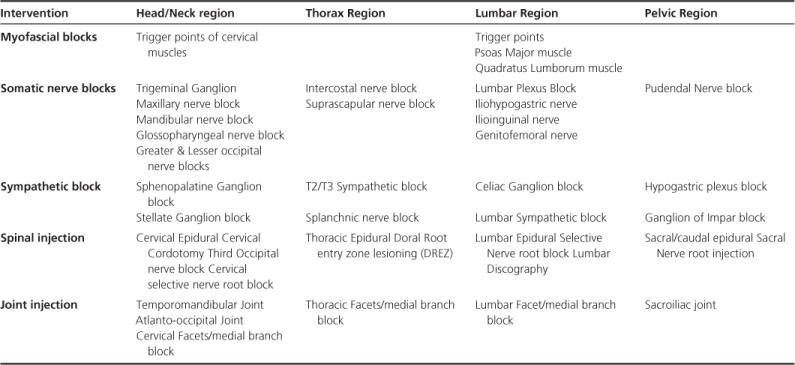
The commonest procedures performed in each anatomical area are listed in Table 16.1. Only some of these procedures are examined in detail and the reader is advised to refer to the ‘Further reading’ list for more information. While many readers may not be actually performing these interventions, it is important to have an understanding of what is involved if referring patients for assessment and consideration of an intervention.
Table 16.1 Common interventional procedures used in each region of the body
Patient assessment and selection
Irrespective of what intervention is chosen, proper patient evaluation and selection, taking into consideration the patient’s unique presentation of symptoms and overall health status, is very important. Malignancy, infection and fractures are some of the ‘red flags’ that must be ruled out prior to the formulation and recommendation of treatment management (Chapter 5). By combining the patients’ pain history, clinical examination and appropriate radiological and biochemical investigations, it is possible to choose a suitable intervention for each patient.
General complications
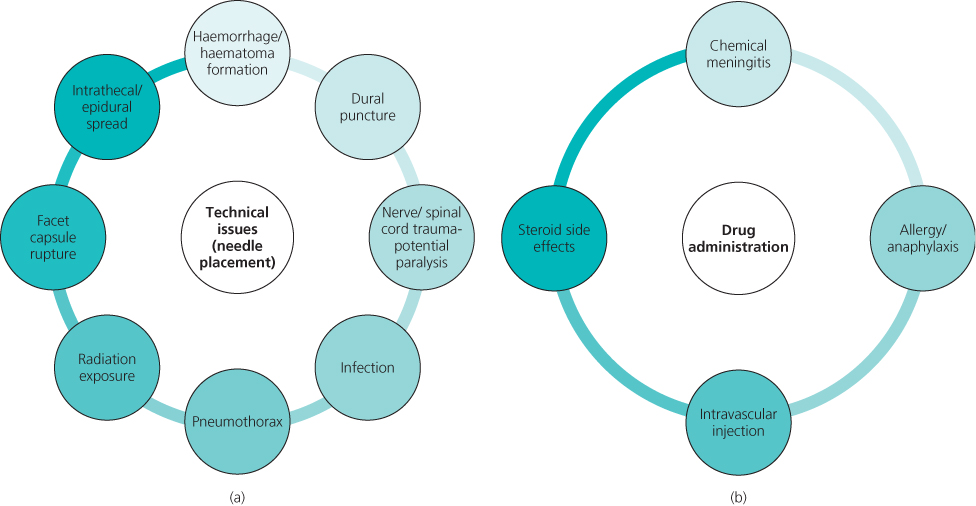
While the benefits of interventional pain strategies are attractive for any symptomatic patient, there are potential risks and complications that should be considered when planning patient management (Figure 16.1). For example, anticoagulation may increase the risks of bleeding, and this should be considered against the potential benefits.
Figure 16.1 Potential complications arising as a result of interventions related to (a) needle placement and (b) drug administration. All these adverse effects, however, are rare and often minor.
Pharmacological intervention
The most commonly drugs used for interventional procedures include corticosteroids and local anaesthetics (lignocaine and bupivacaine). Steroids relieve pain by reducing inflammation, blocking transmission of nociceptive C-fibre input and inhibiting the action of phospholipase A2, both responsible for cell membrane injury and oedema. Due to the risk of complications associated with prolonged use, corticosteroids for interventional procedures are administered not more than three to four times a year. Local anaesthetics are used to confirm appropriate medication delivery and to provide temporary relief until the corticosteroids reach their therapeutic levels.
Non-pharmacological intervention
Radio frequency or pulsed radio frequency lesioning of nerves or ganglion is a neurodestructive technique that uses continuous heat or radio waves to produce controlled tissue destruction (thermocoagulation). These interventions modulate pain transmission without causing clinical signs of nerve damage. Although pain relief is also temporary because of axon regeneration, multiple controlled trials have shown strong evidence in providing lasting relief for some pain syndromes such as facet joint pain.
Myofascial trigger point injections
Indications
There is no agreement on the definition or valid diagnostic criteria of trigger points in chronic pain. Typically, patients complain of muscle pain and examination often identities a point (a trigger point) that is painful on compression and may produce referred pain, motor dysfunction, and/or autonomic phenomena. Many studies have investigated the efficacy of treating trigger point pain using steroids, dry-needling, Botox and antidepressants with varying results.
Technique
Under sterile conditions the tender point is injected with a combination of either steroid and local anaesthetic, or botulinum toxin. Ultrasound visualisation has been used to help guide the deposition of the agents in the correct muscle layer.
Specific complications
These are relatively straightforward to carry out, but accurate localisation and injection of deep muscle may be problematic and the blind nature of needle advancement increases the risks.
Facet joint injection
Indications
Facet joints have been implicated in 15–45% of patients with back pain and 54–60% of patients with neck pain (but see Chapter 5). Described as dull, stiff or achy pain it is exacerbated by movements that compress the joints (extension, rotation). While pain in the lumbar facet joints radiates typically to the buttocks and upper posterior thigh, and cervical facet joint pain presents with headache, shoulder or mid-back pain, the location of referred pain cannot be used reliably to infer the exact spinal level where the pathology is situated. Unfortunately, facet joint pain cannot be diagnosed consistently by clinical examination or by imaging studies.
Technique
With the patient prone and under fluoroscopic guidance, local anaesthetic (bupivacaine) and corticosteroid are injected around the facet joint (Figures 16.2 and 16.3). A 50% reduction in pain after injection is considered a true positive. A single intra-articular injection results in short-term relief (fewer than six weeks) in 46–75% of patients while long-term relief (six weeks or longer) is seen in 20–36% of the patients. Thus, this intervention is both practical and cost efficient as it is diagnostic as well as therapeutic.
Figure 16.2 Lumbar spine radiograph with labelled landmarks. The figure shows the posterior-anterior radiograph of the lumbar spine with the key landmarks labelled. 1 = spinous process, 2 = transverse process, 3 = pedicle and area of the medial branch, 4 = superior articular process, 5 = inferior articular process of the lumbar vertebrae.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








