CHAPTER 21
Interlaminar Epidural Steroid Injections: Cervical, Thoracic, Lumbar, and Caudal
INTRODUCTION
Epidural steroid injections have been used for the treatment of radicular pain and spinal pathology for many decades. The epidural space can be accessed posteriorly via the interlaminar space. Although using an AP lateral or contralateral oblique fluoroscopically guided approach can be more precise and can also help visualize the spread of the injectate under live fluoroscopic view, a “blind” injection performed by a skilled practitioner using a “loss of resistance” technique to identify passage into the epidural space via the ligamentum flavum has been utilized successfully for years. The relative simplicity of the blind technique and one’s ability to perform it without the use of costly equipment such as a fluoroscopy unit has provided a much-needed procedure to the masses especially in developing countries. The use of interlaminar approach to the epidural space for injection is one of the most frequently used procedures in the practice of interventional pain management.
INDICATIONS
• Unilateral or bilateral radiculopathy resulting from
![]() Acute intervertebral disc herniation causing compression or impingement of spinal nerve
Acute intervertebral disc herniation causing compression or impingement of spinal nerve
![]() Acutely herniated nucleus pulposus with compression or local proinflammatory mediator release and resultant nerve irritation
Acutely herniated nucleus pulposus with compression or local proinflammatory mediator release and resultant nerve irritation
![]() Spinal stenosis (acquired or congenital)
Spinal stenosis (acquired or congenital)
![]() Foraminal stenosis
Foraminal stenosis
![]() Lateral recess stenosis
Lateral recess stenosis
![]() Impingement from degenerative disc disease
Impingement from degenerative disc disease
![]() Compression by cysts on zygapophyseal (facet) joints
Compression by cysts on zygapophyseal (facet) joints
• Spondylolisthesis
• Spinal deformity (eg, scoliosis)
• Postlaminectomy syndrome
• Pain from vertebral compression fractures
• Pain from herpes zoster
RELEVANT ANATOMY
• Level of interlaminar injections are initially identified via palpation between spinous processes or via identification of the space between vertebrae on fluoroscopic imaging.
• From superficial to deep (dorsal), an epidural needle passes through the following structures for a midline approach: skin, subcutaneous tissues, supraspinous ligament, interspinous ligament, ligamentum flavum, and the epidural space. If the injection proceeds deeper, it comes in contact with the dura mater and the subarachnoid space.
• From superficial to deep (dorsal), an epidural needle passes through the following structures for a paramedian approach: skin, subcutaneous tissues, ligamentum flavum, and the epidural space.
• The epidural space is bounded by the ligamentum flavum and the lamina posteriorly, the posterior longitudinal ligament anteriorly, and the vertebral pedicles and neural foramina laterally.
• The epidural space contains fat, lymphatics, venous plexi, connective tissue, and the spinal nerve roots.
• The ligamentum flavum can be discontinuous in the cervical and high thoracic regions, making localization of the epidural space via loss of resistance technique potentially more challenging.
CONTRAINDICATIONS
• Absolute
![]() Local or systemic infection
Local or systemic infection
![]() Acute spinal cord compression (injection at that level)
Acute spinal cord compression (injection at that level)
![]() Untreated bleeding disorders that predispose to hemorrhage
Untreated bleeding disorders that predispose to hemorrhage
![]() Uncontrolled or untreated systemic disorders (cardiopulmonary, renal, endocrine) where steroid effects may cause acute or subacute decompensation of the patient’s medical condition
Uncontrolled or untreated systemic disorders (cardiopulmonary, renal, endocrine) where steroid effects may cause acute or subacute decompensation of the patient’s medical condition
![]() Hypersensitivity or allergy to medications used in epidural steroid injection
Hypersensitivity or allergy to medications used in epidural steroid injection
![]() Patient refusal
Patient refusal
• Relative
![]() Preprocedure evaluation in patients with immunosuppressive diseases should be undertaken to rule out the potential for latent infection.
Preprocedure evaluation in patients with immunosuppressive diseases should be undertaken to rule out the potential for latent infection.
![]() Considerations should be made to perform epidural injections without fluoroscopy in pregnant women to decrease the risk of radiation exposure to the fetus.
Considerations should be made to perform epidural injections without fluoroscopy in pregnant women to decrease the risk of radiation exposure to the fetus.
![]() Morbid obesity and inability to lie down (especially if there is respiratory distress).
Morbid obesity and inability to lie down (especially if there is respiratory distress).
![]() Concurrent use of anticoagulants or antiplatelet agents (other than aspirin or nonsteroidal anti-inflammatory medications). A careful risk assessment in patients requiring anticoagulation needs to be performed.
Concurrent use of anticoagulants or antiplatelet agents (other than aspirin or nonsteroidal anti-inflammatory medications). A careful risk assessment in patients requiring anticoagulation needs to be performed.
PREOPERATIVE PREPARATIONS
• Fully informed consent must be obtained prior to any intervention from the patient or legal representative.
• Preprocedure vital signs should be obtained and documented, including temperature, blood pressure, heart rate, and oxygen saturation.
• If a cervical epidural steroid injection will be performed, some practitioners may start an intravenous line. Occasionally, preprocedure IV access must be obtained prior to procedure for patients with a history of vasovagal syncope.
• Preprocedure pain level and character of pain (location, duration, intensity) should be elicited prior to procedure. If this is a repeat injection, subsequent pain relief or lack thereof should be assessed and documented.
• The classic interlaminar injection is done with the patient in the prone position at all levels.
• Some practitioners may perform cervical epidural steroid injections with fluoroscopy with the patient in a seated position with the head face down on the fluoroscopy table.
• Patient should be positioned appropriately on fluoroscopy table in order to maximize the spaces between the lamina. A pillow may be placed under the patient near the level of interest to accentuate kyphosis or reverse lordosis to maximize the width of the interlaminar space.
• Patient movement has been implicated in a significant number of cases of spinal cord injury related to epidural injections. Judicious selection of patients requiring sedation may decrease the risk of complications related to patient movement. (See Chapter 11.)
Equipment
1. Room
![]() Monitor for vital signs (minimum includes blood pressure, heart rate, oxygen saturation).
Monitor for vital signs (minimum includes blood pressure, heart rate, oxygen saturation).
![]() Fluoroscopy machine with fluoroscopy-compatible table (CT-guidance and ultrasound guidance are also utilized but fluoroscopy is much more common).
Fluoroscopy machine with fluoroscopy-compatible table (CT-guidance and ultrasound guidance are also utilized but fluoroscopy is much more common).
![]() Lead apron (for coverage of thorax and thyroid). Use of radiation attenuating gloves and lead-lined eye protection is highly recommended.
Lead apron (for coverage of thorax and thyroid). Use of radiation attenuating gloves and lead-lined eye protection is highly recommended.
![]() Pillows to improve positioning for procedure and patient comfort.
Pillows to improve positioning for procedure and patient comfort.
![]() Oxygen supply (wall or tank) and suction mounted and ready to use.
Oxygen supply (wall or tank) and suction mounted and ready to use.
![]() Immediate availability of resuscitation equipment, including Ambu bag and/or advanced airway devices. Devices and medications for advanced cardiac life support should be available or be ready to be activated quickly.
Immediate availability of resuscitation equipment, including Ambu bag and/or advanced airway devices. Devices and medications for advanced cardiac life support should be available or be ready to be activated quickly.
2. Procedure
![]() Epidural kits containing
Epidural kits containing
![]() Syringes for local anesthetic infiltration, preparation of epidural injection, needles for drawing up medication and skin/tissue infiltration.
Syringes for local anesthetic infiltration, preparation of epidural injection, needles for drawing up medication and skin/tissue infiltration.
![]() Syringe for loss of resistance.
Syringe for loss of resistance.
![]() Skin preparation solutions to sterilize the skin for the procedure.
Skin preparation solutions to sterilize the skin for the procedure.
![]() Tuohy needle for epidural injection (gauges are practice specific but generally range from 18-gauge to 20-gauge needles).
Tuohy needle for epidural injection (gauges are practice specific but generally range from 18-gauge to 20-gauge needles).
![]() Labels for syringes (The Joint Commission [JCAHO] standard).
Labels for syringes (The Joint Commission [JCAHO] standard).
![]() The addition of tubing to connect the epidural tubing to the syringe containing contrast can be used to distance the provider from fluoroscopy radiation during continuous injection of contrast and also avoid needle movement.
The addition of tubing to connect the epidural tubing to the syringe containing contrast can be used to distance the provider from fluoroscopy radiation during continuous injection of contrast and also avoid needle movement.
![]() Sterile drape
Sterile drape
![]() Gauze
Gauze
![]() Sharps recovery/protective device
Sharps recovery/protective device
3. Medications
![]() Corticosteroids (particulate or nonparticulate determined by provider)
Corticosteroids (particulate or nonparticulate determined by provider)
![]() Radiopaque water-soluble contrast
Radiopaque water-soluble contrast
![]() Sterile saline
Sterile saline
![]() Local anesthetic for epidural injection (often bupivacaine, ropivacaine, or lidocaine); lidocaine for skin puncture analgesia
Local anesthetic for epidural injection (often bupivacaine, ropivacaine, or lidocaine); lidocaine for skin puncture analgesia
Techniques
1. Lumbar interlaminar epidural steroid injection
![]() Identify the appropriate interlaminar space with fluoroscopy using a radio-opaque device to mark the space (metal marker, Kelly clamp).
Identify the appropriate interlaminar space with fluoroscopy using a radio-opaque device to mark the space (metal marker, Kelly clamp).
![]() Prepare the skin using chlorhexidine and drape.
Prepare the skin using chlorhexidine and drape.
![]() Infiltrate the skin and subcutaneous tissues with 1% lidocaine using a 25- or 27-gauge infiltration needle. After initial infiltration, inject into the deeper ligamentous structures using a 22- or 25-gauge 1.5-in needle.
Infiltrate the skin and subcutaneous tissues with 1% lidocaine using a 25- or 27-gauge infiltration needle. After initial infiltration, inject into the deeper ligamentous structures using a 22- or 25-gauge 1.5-in needle.
![]() With the fluoroscope in the AP position, a Tuohy or Weiss needle is placed in the midline or paramedian approach with the tip of the needle toward the midline of the fluoroscopic image between the spinous processes of interest for bilateral radicular symptoms or to the ipsilateral side (of the patient’s pain), just lateral to the spinous process.
With the fluoroscope in the AP position, a Tuohy or Weiss needle is placed in the midline or paramedian approach with the tip of the needle toward the midline of the fluoroscopic image between the spinous processes of interest for bilateral radicular symptoms or to the ipsilateral side (of the patient’s pain), just lateral to the spinous process.
![]() The needle is advanced until a subjective feeling of “engagement” of the ligament has been felt.
The needle is advanced until a subjective feeling of “engagement” of the ligament has been felt.
![]() The fluoroscope is rotated to the lateral position and depth is confirmed. Prior to entry into the epidural space, the stylet is removed and a loss-of-resistance syringe is attached filled with 1 mL or more of saline with an air bubble. Rapid, shallow ballottement of the syringe continues as the needle is advanced into the epidural space until there is loss of resistance and injection of saline through the epidural needle with minimal syringe pressure.
The fluoroscope is rotated to the lateral position and depth is confirmed. Prior to entry into the epidural space, the stylet is removed and a loss-of-resistance syringe is attached filled with 1 mL or more of saline with an air bubble. Rapid, shallow ballottement of the syringe continues as the needle is advanced into the epidural space until there is loss of resistance and injection of saline through the epidural needle with minimal syringe pressure.
![]() Entry into the epidural space is confirmed by injecting 0.5 to 2 mL of nonionic contrast to verify the spread in the epidural space.
Entry into the epidural space is confirmed by injecting 0.5 to 2 mL of nonionic contrast to verify the spread in the epidural space.
![]() Unilateral or bilateral spread is confirmed with fluoroscopy image capture in the AP position, while the lateral view shows the spread of the contrast in the posterior or anterior epidural space.
Unilateral or bilateral spread is confirmed with fluoroscopy image capture in the AP position, while the lateral view shows the spread of the contrast in the posterior or anterior epidural space.
![]() Injection of steroid with or without local anesthetics and/or saline is performed.
Injection of steroid with or without local anesthetics and/or saline is performed.
![]() Replace the stylet and withdraw the epidural needle.
Replace the stylet and withdraw the epidural needle.
![]() Place gauze on needle entry site and apply pressure if there is bleeding. Place sterile dressing or bandage over entry site.
Place gauze on needle entry site and apply pressure if there is bleeding. Place sterile dressing or bandage over entry site.
![]() Patient should be sat upright. Standing should always be with assistance in case there is mild weakness after the injection or orthostatic hypotension (Figure 21-1).
Patient should be sat upright. Standing should always be with assistance in case there is mild weakness after the injection or orthostatic hypotension (Figure 21-1).
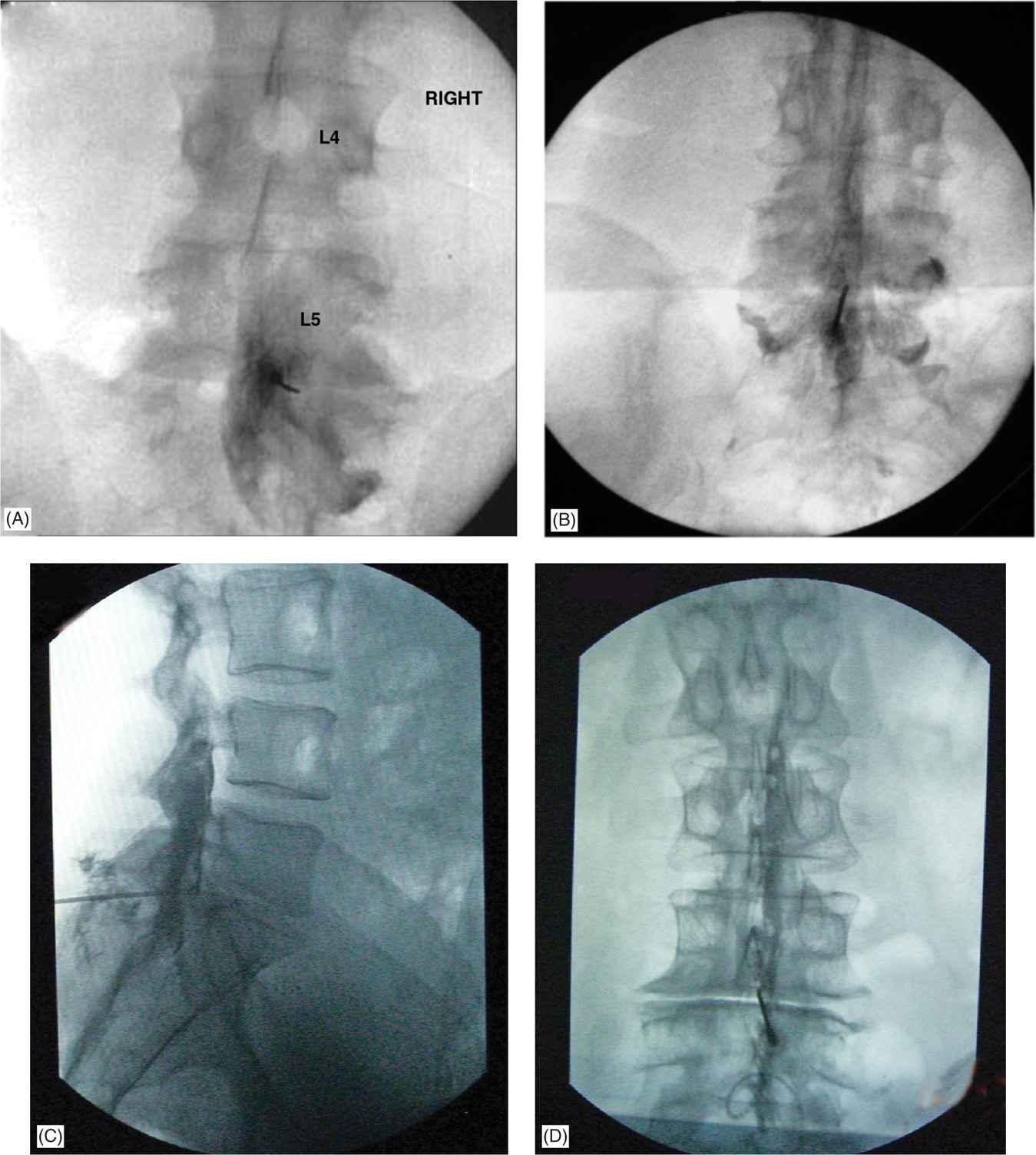
Figure 21-1. (A) Fluoroscopic images of a lumbar interlaminar injection in AP view. Note the unilateral spread of the contrast and the needle placement in the paramedian area. (B) Fluoroscopic image of a midline lumbar interlaminar injection in AP view. Note the bilateral spread of the contrast and the needle placement in the paramedian area. This is not the most common type of spread seen. (C) Fluoroscopic image of a lumbar interlaminar injection in lateral view. Note the posterior and lateral spread of the contrast. Absence of smooth contrast silhouette close to the posterior margin of the vertebral body suggests epidural placement. (D) Fluoroscopic image of a midline lumbar interlaminar injection in AP view. Note the presence of the bubbles (air used for the loss of resistance technique) in the cephalad area.
2. Cervical interlaminar epidural steroid injection
![]() The technique for cervical epidural steroid injections is very similar to lumbar epidural steroid injections with some distinct differences:
The technique for cervical epidural steroid injections is very similar to lumbar epidural steroid injections with some distinct differences:
![]() Positioning
Positioning
![]() A roll or pillows are placed under the chest so that there is mild flexion of the neck. A pillow or padded gauze can be placed on the forehead to prevent the patient’s face from being compressed by the table. The patient’s arms are placed at their sides.
A roll or pillows are placed under the chest so that there is mild flexion of the neck. A pillow or padded gauze can be placed on the forehead to prevent the patient’s face from being compressed by the table. The patient’s arms are placed at their sides.
![]() Positioning devices are available to allow for consistent positioning of the patient’s head with the arms flexed and placed above their head (“Superman” position).
Positioning devices are available to allow for consistent positioning of the patient’s head with the arms flexed and placed above their head (“Superman” position).
![]() Anatomy
Anatomy
![]() There is no interspinous ligament in the cervical space. Additionally, 50% of cryomicrotomal specimens show an absence of a midline ligamentum flavum (gaps) with absence of a posterior epidural space above C7-T1.
There is no interspinous ligament in the cervical space. Additionally, 50% of cryomicrotomal specimens show an absence of a midline ligamentum flavum (gaps) with absence of a posterior epidural space above C7-T1.
![]() Some practitioners may only perform cervical interlaminar epidurals at C7-T1 using either the volume of injectate- or catheter-directed delivery to deposit medications to the level of interest (Figure 21-2).
Some practitioners may only perform cervical interlaminar epidurals at C7-T1 using either the volume of injectate- or catheter-directed delivery to deposit medications to the level of interest (Figure 21-2).
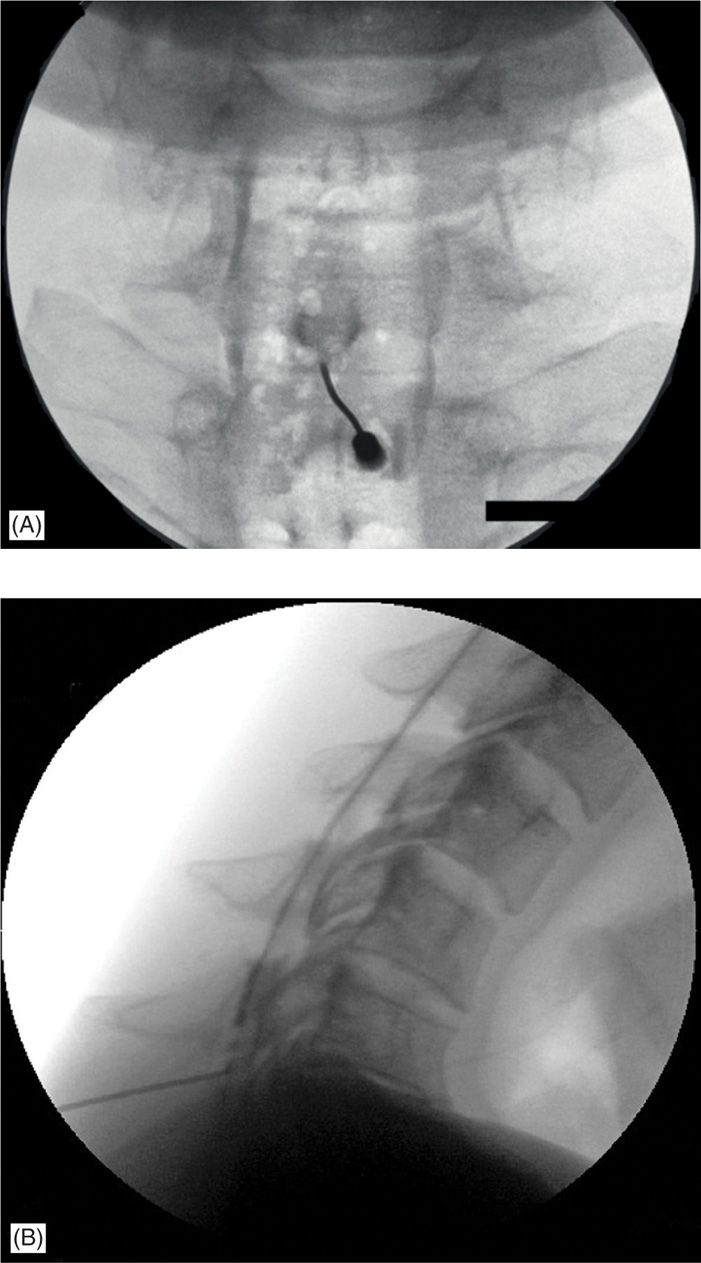
Figure 21-2. (A) Fluoroscopic image of a midline cervical interlaminar injection in AP view. Note the presence of the air bubbles form the use of loss of resistance technique. A more reliable technique is to use an air/fluid interface in the loss of resistance syringe as the fluid provides a noncompressible medium and in case of an inadvertent intrathecal penetration, prevents sudden headache due to air travelling to the intra-ventricular area in the brain. (B) Fluoroscopic image of a midline cervical interlaminar injection in lateral view. Note the spread of the contrast medium in the posterior epidural space. Although the spread is also in the lateral epidural space, the thinness of the contrast film viewed in a perpendicular plane makes it nearly invisible on a lateral view.
3. Thoracic interlaminar epidural steroid injection
![]() Positioning
Positioning
![]() Pillows may be placed under the patient while in the prone position to accentuate the thoracic kyphosis. Arms may need to be placed either at the patient’s side (for upper thoracic injections) or above the patient’s head (for lower thoracic injections).
Pillows may be placed under the patient while in the prone position to accentuate the thoracic kyphosis. Arms may need to be placed either at the patient’s side (for upper thoracic injections) or above the patient’s head (for lower thoracic injections).
![]() Anatomic abnormalities may preclude a midline approach. A paramedian approach may be necessary to access the thoracic epidural space (Figure 21-3).
Anatomic abnormalities may preclude a midline approach. A paramedian approach may be necessary to access the thoracic epidural space (Figure 21-3).
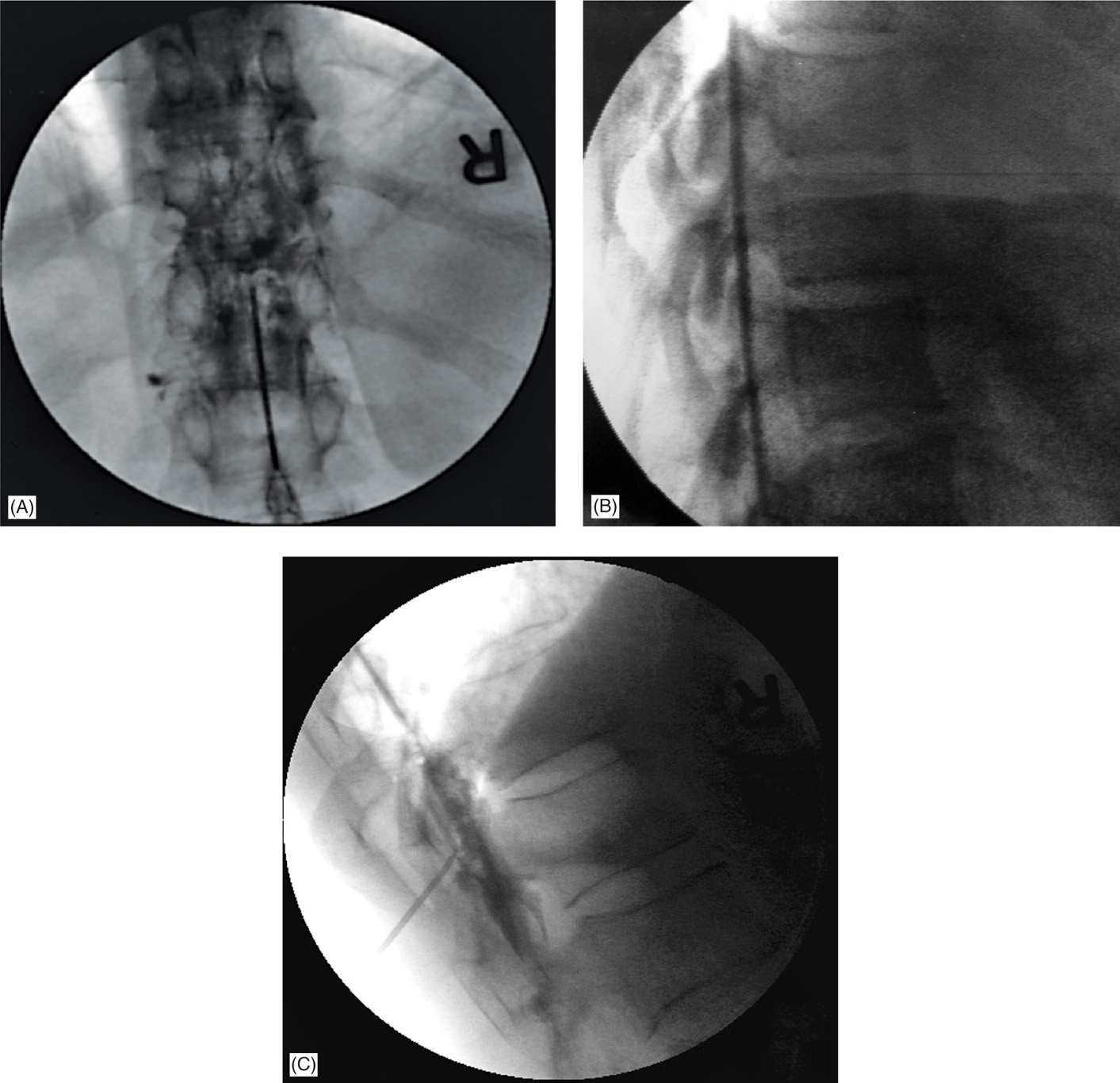
Figure 21-3. (A) Fluoroscopic image of a midline thoracic interlaminar injection in AP view. At higher thoracic levels, a posterior midline approach is very difficult and a paramedian approach is preferred. (B) Fluoroscopic image of a midline thoracic interlaminar injection in lateral view. Just as in the cervical area, thoracic epidurals in a lateral view are seen to be mainly in the posterior epidural space as the lateral spread is too thin to be visualized in lateral view. An AP view would clearly demonstrate spread in the lateral epidural space (see Figure 21-3A). A greater amount of contrast may show lateral spread as in Figure 21-3C. (C) Fluoroscopic image of a midline thoracic interlaminar injection in lateral view with contrast spreading in the lateral epidural space as well.
4. Caudal epidural steroid injection
![]() Caudal epidural steroid injections are most commonly performed in patients with previous laminectomies or with abnormal anatomy in the lumbar space.
Caudal epidural steroid injections are most commonly performed in patients with previous laminectomies or with abnormal anatomy in the lumbar space.
![]() Positioning
Positioning
![]() A roll or a pillow may be placed under the patients pelvis in the prone position. Tape may need to be applied to the patient’s buttocks to laterally retract the tissue to access the sacral midline.
A roll or a pillow may be placed under the patients pelvis in the prone position. Tape may need to be applied to the patient’s buttocks to laterally retract the tissue to access the sacral midline.
![]() Preparation
Preparation
![]() Given the location of the injection, the potential injection site and the surrounding area must be meticulously disinfected.
Given the location of the injection, the potential injection site and the surrounding area must be meticulously disinfected.
![]() Technique
Technique
![]() The sacral cornua are identified by palpation and skin site analgesia is administered using 1% lidocaine.
The sacral cornua are identified by palpation and skin site analgesia is administered using 1% lidocaine.
![]() The fluoroscopy machine is placed in the lateral position and the sacral hiatus is imaged and marked with a radio-opaque marker.
The fluoroscopy machine is placed in the lateral position and the sacral hiatus is imaged and marked with a radio-opaque marker.
![]() If using a Tuohy needle, the needle should be bent with a convex bend to facilitate placement of the needle within the caudal epidural space. Alternatively, a 22-gauge Quincke spinal needle with a convex bend may also be used.
If using a Tuohy needle, the needle should be bent with a convex bend to facilitate placement of the needle within the caudal epidural space. Alternatively, a 22-gauge Quincke spinal needle with a convex bend may also be used.
![]() Passage of the needle though the sacrococcygeal ligament may be felt (“pop”) and the need is advanced at a less acute angle.
Passage of the needle though the sacrococcygeal ligament may be felt (“pop”) and the need is advanced at a less acute angle.
![]() Confirmation of position is performed with nonionic contrast injection.
Confirmation of position is performed with nonionic contrast injection.
![]() Larger volumes of injectate may be required (about 20 mL of steroid, ±local anesthetic, and sterile saline) to fill the caudal epidural space and to achieve cephalad spread of injectate to the desired lumbar levels (Figure 21-4).
Larger volumes of injectate may be required (about 20 mL of steroid, ±local anesthetic, and sterile saline) to fill the caudal epidural space and to achieve cephalad spread of injectate to the desired lumbar levels (Figure 21-4).
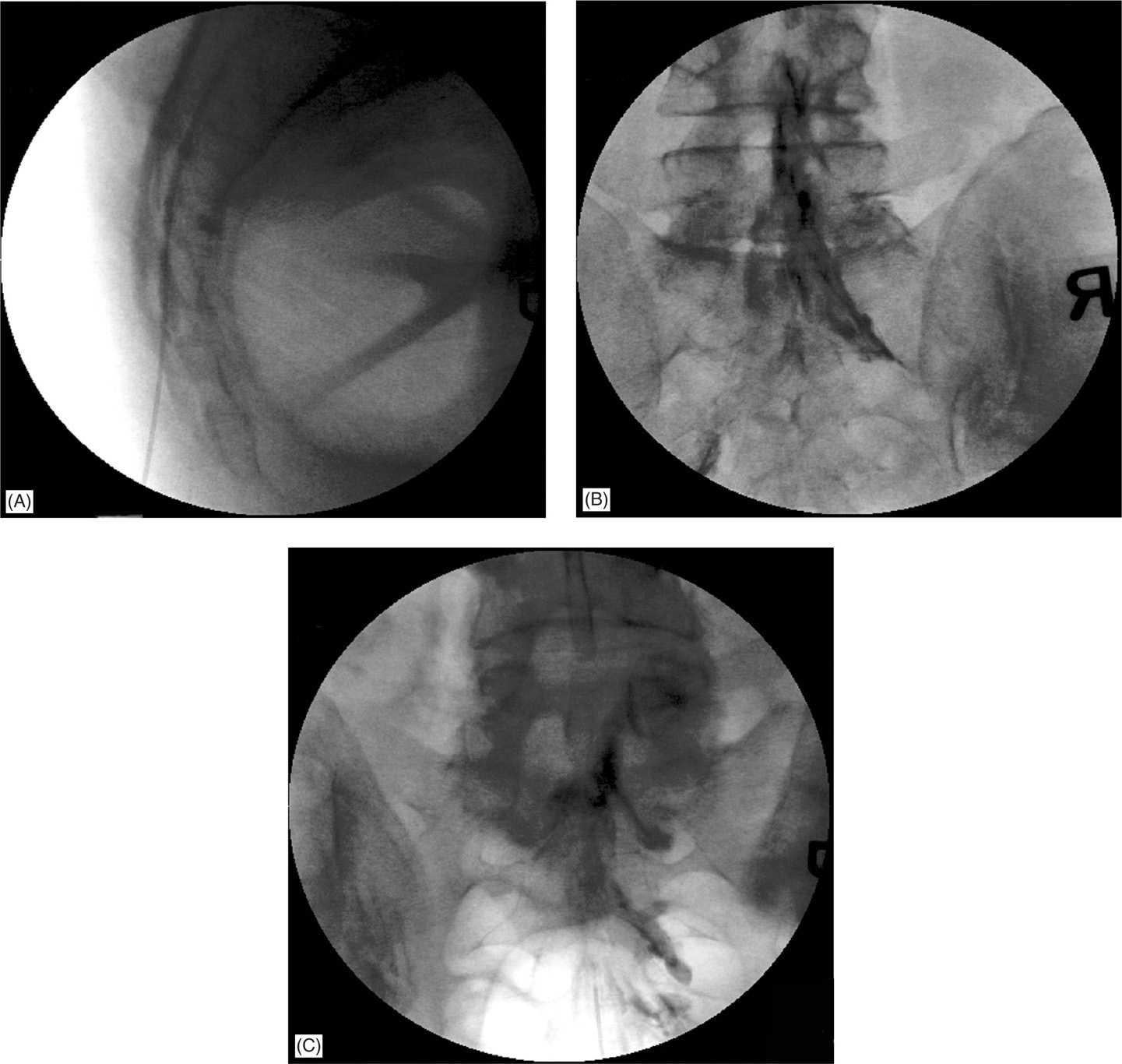
Figure 21-4. (A) Caudal epidural injection: lateral view with the needle through the sacral hiatus. Note the position of the needle in the anterior epidural space. This can be achieved selectively by placing the needle slightly more vertically. (B) Caudal epidural injection: AP view. The epidural needle tip is not visible. (C) Caudal epidural injection: AP view. The needle tip is at approximately S3 level. In most cases of spinal stenosis, significant amount of contrast can be seen escaping through the sacral foramina anteriorly following the path of least resistance. Unilateral spread is not uncommon.
POSTPROCEDURE INSTRUCTIONS
• Patient should have vital signs checked immediately after the procedure.
• Patients should be able to stand without difficulty and without significant deviation from their preprocedure neurologic status.
• If intravenous sedation was administered, the patient should be transferred to a postanesthesia care unit (or equivalent) for observation until the patient is considered recovered from sedation.
• Patient should not engage in any strenuous activities for the rest of the day but can resume normal activities the next day.
COMPLICATIONS AND PITFALLS
• Complications related to drug effects
![]() Corticosteroids. Major effects include flushing, hyperglycemia, hypothalamic-pituitary-adrenal axis suppression, fluid retention, changes in vascular tone usually resulting in hypertension. Corticosteroids used acutely and chronically affect all organ systems, and a full account of organ-specific effects is beyond the scope of this text.
Corticosteroids. Major effects include flushing, hyperglycemia, hypothalamic-pituitary-adrenal axis suppression, fluid retention, changes in vascular tone usually resulting in hypertension. Corticosteroids used acutely and chronically affect all organ systems, and a full account of organ-specific effects is beyond the scope of this text.
![]() Contrast dye-allergic reaction, flushing.
Contrast dye-allergic reaction, flushing.
![]() Local anesthetic-related weakness, numbness, etc.
Local anesthetic-related weakness, numbness, etc.
• Complications related to procedure
![]() Presyncope or syncope
Presyncope or syncope
![]() Nausea and vomiting
Nausea and vomiting
![]() Dizziness
Dizziness
![]() Back pain
Back pain
![]() Feeling of “pressure” or fullness at the level of the injection
Feeling of “pressure” or fullness at the level of the injection
![]() Infection (abscess, meningitis, arachnoiditis)
Infection (abscess, meningitis, arachnoiditis)
![]() Spinal cord injury
Spinal cord injury
![]() Spinal cord infarction
Spinal cord infarction
![]() Numbness/weakness
Numbness/weakness
![]() Paralysis
Paralysis
![]() Inadvertent subarachnoid/subdural injection
Inadvertent subarachnoid/subdural injection
![]() Postdural puncture headache
Postdural puncture headache
![]() Bleeding/bruising at skin site
Bleeding/bruising at skin site
![]() Epidural hematoma
Epidural hematoma
![]() Muscle soreness from needle placement (more common with larger-gauge needles)
Muscle soreness from needle placement (more common with larger-gauge needles)
![]() Air embolism (if using loss of resistance to air)
Air embolism (if using loss of resistance to air)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






