CHAPTER 57
Intercostal Nerve Block
INTRODUCTION
The intercostal nerve block was first described in 1907 by Heinrich Braun1 to treat acute and chronic pain of the posterior and anterior portions of the superficial thorax and upper abdomen. The intercostal nerves are mixed nerves of with motor and sensory components. Elaborate on the function of the ICN.
INDICATIONS
Intercostal blocks are useful in relieving post-traumatic and postoperative pain, and more recently, chronic nonmalignant and from malignancies processes involving the thoracic wall (Table 57-1).2–4 Blockade of the intercostal nerve may ameliorate painful nerve impulses associated with chronic neuropathic pain. Local anesthetic blocks can also be used to diagnose pain problems when both thoracic and visceral sources are suspected. Similar techniques can be used to perform neurolysis (cryoablation, radiofrequency ablation, or chemical neurolysis).
TABLE 57-1. Indications for Intercostal Nerve Blocks3,5,6
CONTRAINDICATIONS
While there are few absolute contraindications to an intercostal nerve block, extra caution must be taken in patients to whom a pneumothorax may be detrimental. These patients may include:
• Respiratory decompensated patients
• Patients with a single lung on the side of the planned procedure
• Patients on positive pressure ventilations
• Postsurgical patients
General relative contraindications include blood dyscrasias, local or uncontrolled systemic infection, or unknown anatomical changes (eg, unknown rib resection).
Advantages
As with other regional techniques, intercostal nerve blocks are associated with:
• Decreased need for parenteral or oral opioids.3,5
• In thoracic surgery, the use of intercostal nerve blocks allows for improved respiratory function in FEV1 and Peak expiratory flow rate.5,7
• Decreasing oral or parental opioids may reduce the incidence of nausea, vomiting, urinary retention, itching, and hypotension.
Complications
While complication rates vary, performing the block with imaging may reduce some of the associated risks described below (Table 57-2).
TABLE 57-2. Complications Associated with Intercostal Nerve Blocks3
ANATOMY
The intercostal nerve travels along the intercostal groove of each corresponding rib. Each intercostal nerve, bilaterally from T1-T12, emerges from the intervertebral foramen of the respective vertebra. From the foramen, each thoracic nerve root divides into four branches:
• The white and gray rami communicate (traveling anteriorly to join the sympathetic ganglion).
• The posterior dorsal ramus.
• The ventral ramus (which becomes the intercostal nerve).5,8
The Ventral Ramus
• The ventral ramus joins with the corresponding thoracic artery and vein, forming the neurovascular bundle, which carries both sensory and motor fibers (Figure 57-1).
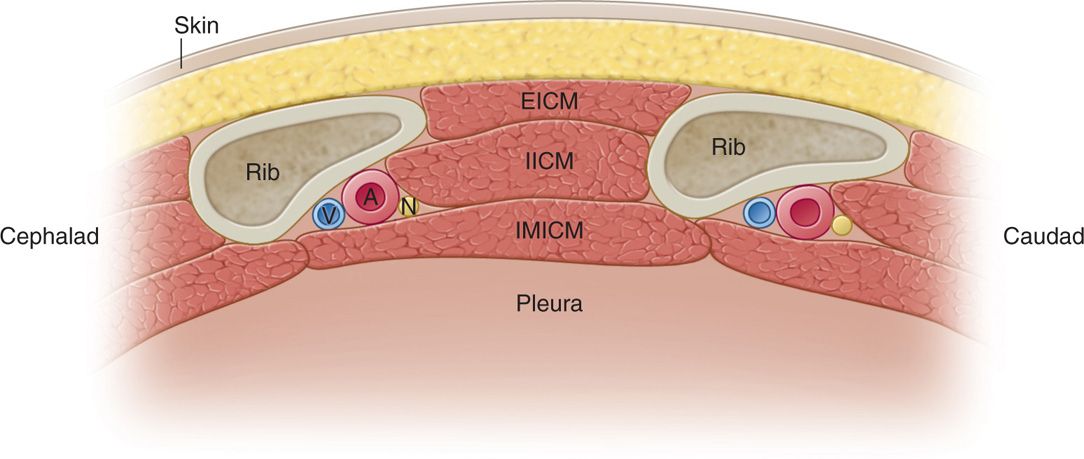
Figure 57-1. Cross-sectional view of the intercostal space from a cephalocaudal transection. This cross section is a common view obtained with ultrasound-guided procedures involving the intercostal nerve. EICM, external intercostal muscle; IICM, internal intercostal muscle; IM ICM, innermost intercostal muscle; V-A-N = intercostal vein, artery, and nerve, respectively. (Adapted from Cousins & Bridenbaugh, 1998.)
• Within this bundle, the vein is positioned superior to the artery and nerve, with the intercostal nerve sitting most inferiorly (V-A-N configuration).
• About 3 cm away from the intervertebral foramen, the neurovascular bundle first transects the internal intercostal membrane, where it then runs parallel with the rib traveling in the intercostal groove, located on the internal surface of inferior border of the rib.
• At this point, the intercostal nerve is situated between the innermost intercostal muscle and the internal intercostal muscle.
The first major branch of the intercostal nerve is the lateral cutaneous branch, occurring at midaxillary line (Figure 57-2). The remaining intercostal nerve continues to travel anteriorly and terminates into the anterior branch at the sternum. Along the course of the nerve, smaller branches may separate from the intercostal nerve (ie, anterior and posterior cutaneous branches). The intercostal muscles and parietal pleura are innervated by small branches of the intercostal nerves of T1-T6.
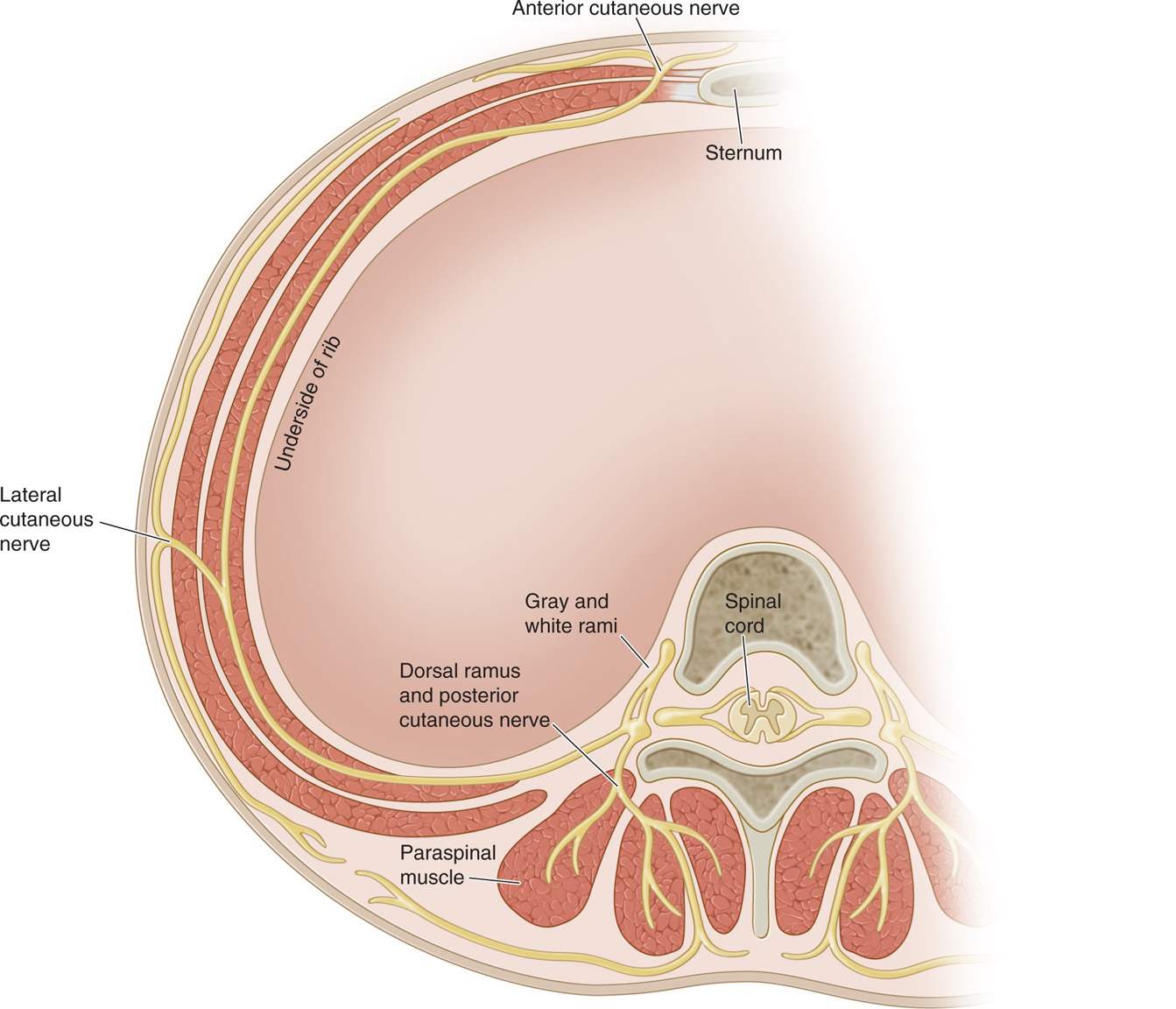
Figure 57-2. Cross section of vertebral body. Path and branches of the intercostal nerve are marked. The thoracic nerve root leaves the vertebral body and lies inferior to the corresponding rib. (Adapted from Cousins & Bridenbaugh, 1998.)
The T12 intercostal nerve:
• The T12 intercostal nerve does not run as closely to the intercostal groove of its accompanying rib as the other intercostal nerves do, making it a more difficult nerve to identify and anesthetize.5
• A substantial part of the T12 ventral rami ultimately joins the ventral ramus of L1, forming the iliohypogastric, ilioinguinal, and genitofemoral nerves.
• The remaining portion transects the transverse abdominis muscle and lies between that and internal oblique muscle.8
Lateral cutaneous branches:
• The lateral branches of the intercostal nerve pierce the internal and external intercostal muscles, dividing into anterior and posterior branches that innervate muscles and skin of the lateral aspects of the chest.
• The lateral anterior divisions of T7-T11 supply the skin extending to the lateral edges of the rectus abdominis muscle. The lateral posterior division supplies the skin overlying the latissimus dorsi muscle.8
Anterior cutaneous branches:
• The anterior cutaneous branches of T2-T6 travel through the external intercostal and pectoralis major muscles, entering into the superficial fascia at the lateral border of the sternum.
• These nerves supply the midline portion of the anterior thoracic wall.
• The anterior branches of T7-T12 supply the motor nerves to the rectus abdominis muscle as well as sensory fibers to the skin of the anterior abdominal wall.
• Some branches continue to travel anteriorly to innervate the parietal peritoneum and the cutaneous area of the abdominal midline.5,8
PREOPERATIVE CONSIDERATIONS
As with any regional anesthetic technique, proper preparation is essential for a safely performed procedure. A patient’s airway, respiratory, and cardiac status and examination should be performed. Resuscitation equipment should be nearby, and if sedation and analgesia are used, supplemental oxygenation may be necessary. Postprocedure evaluations should include signs of pneumothorax, local anesthetic toxicity, and intrathecal injection. Vital sign monitoring, including heart rate, rhythm, and oxygen saturation, should be performed.
Technique
Perform a cardiac and respiratory assessment to determine the patient can tolerate the blockade of one or more intercostal nerves. Obtain baseline vital signs and consider monitors to be placed on the patient. Supplemental oxygenation should be available. Resuscitation cart should be accessible. Larger needle gauges (smaller diameter) could reduce the risk of puncturing the pleura. Usually, 2 to 3 mL of solution is sufficient to successfully block the intercostal nerve. Commonly injected local anesthetic solutions include lidocaine (1%-2%), ropivicaine (0.2%-0.5%), or bupivicaine (0.25%-0.5%).
Anatomical Landmark Technique
The patient can be in the prone, sitting, or lateral decubitus position. The angle of the rib (where the rib begins its bend in front of the tubercle), which is usually about 6 to 8 cm from the paraspinal muscles for lower ribs and 4 to 7 cm for upper ribs, is located by palpation. Blocks medial to the rib angle may pose more risks, as the nerves lie deep to the posterior intercostal membrane with very little tissue between it and the parietal pleura.
CLINICAL PEARLS
• At the angle of the rib, the risk of a dural injection is unlikely. The rib is relatively superficial and the subcostal groove is at the widest, minimizing the risk of a pneumothorax, hopefully.
• The intercostal nerve is oriented inferiorly to the intercostal artery, and surrounded by adipose tissue, coursing between the internal intercostal and innermost intercostal muscles.
• Once the location is decided, apply a disinfectant preparation (consider chlorohexidine or betadine), draping and sterile precautions.
• While retracting the skin over the rib superiorly, infiltrate the skin with local anesthetic (usually a 30-gauge needle and 1 mL of local anesthetic is sufficient) at the puncture site. The rib palpated should correspond to the intercostal nerve to be blocked.
• The preferred target is the inferior border of the rib.
• Introduce the needle (usually a 22- or 25-gauge 1-in spinal needle) and contact the rib. While maintaining control of the needle, slowly walk the needle caudally with the injecting hand.
• When bony contact has ceased, slowly advance (usually about 2-3 mm) until a subtle “pop” through the fascia of the internal intercostal muscles is felt. Use of a blunt needle can facilitate the tactile “pop.”
• The average distance between the posterior aspects of the rib to pleura may be as little as few millimeters.9
• After negative aspiration, 2 to 5 mL of local anesthetic can be injected.
Fluoroscopy-Guided Technique
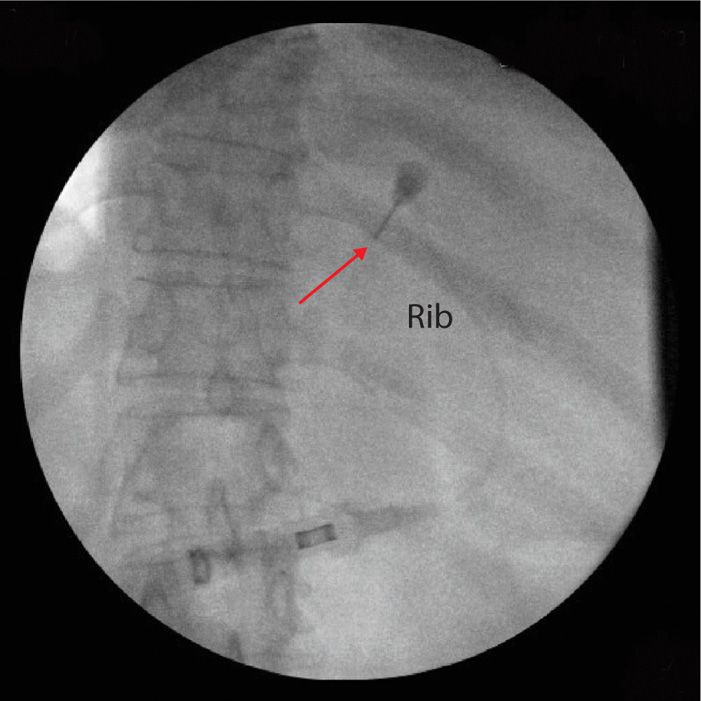
The anatomical technique can be modified such that the rib is visualized under fluoroscopy. This may be especially beneficial when the rib cannot be reliably palpated. Again, the needle is directed to contact the inferior border of the corresponding rib and directed caudally such that the needle is both inferior to the rib and at the anterior border of the rib in lateral and AP view (Figures 57-3 and 57-4, respectively).
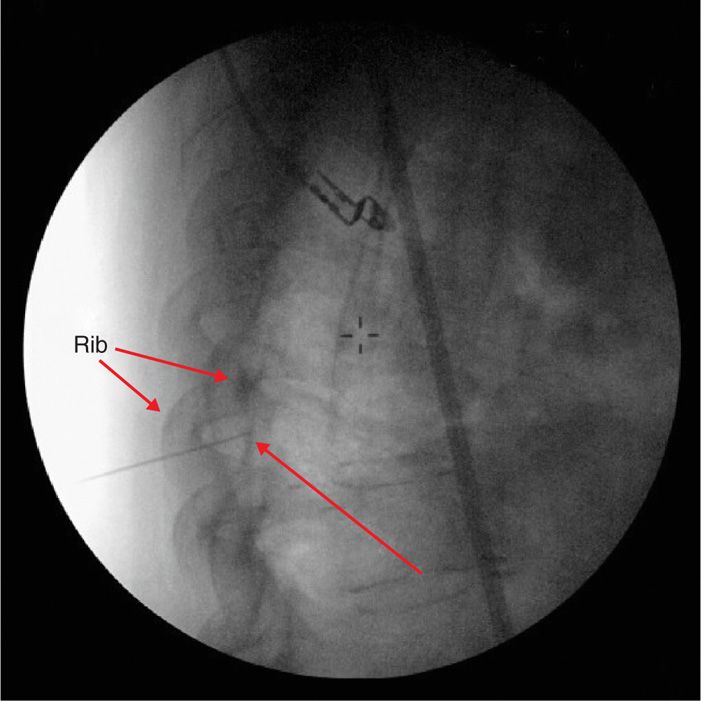
Figure 57-3. Lateral view of the intercostal nerve block under fluoroscopic guidance. The white arrow shows the needle at the anterior border of the rib. This image can be used in conjunction with the AP view to accurately guide the needle.
Figure 57-4. AP view of fluoroscope-guided intercostal nerve block. The needle placement is confirmed to be at the inferior border of the rib.
Ultrasound-Guided Technique
• The use of ultrasonography allows for real time visualization of needle placement and local anesthetic injection.
• This technique has the potential to reduce incorrect needle positions and pleural punctures when done appropriately.
• The ultrasound probe (usually high-frequency linear probes) is placed in the longitudinal axis, parallel to the posterior mid-clavicular or mid-axillary line (Figure 57-5).

Figure 57-5. Position of ultrasound probe, needle, machine, and rib markings to perform an intercostal nerve block.
• This allows for views of two ribs in cross-sectional view (Figure 57-6).
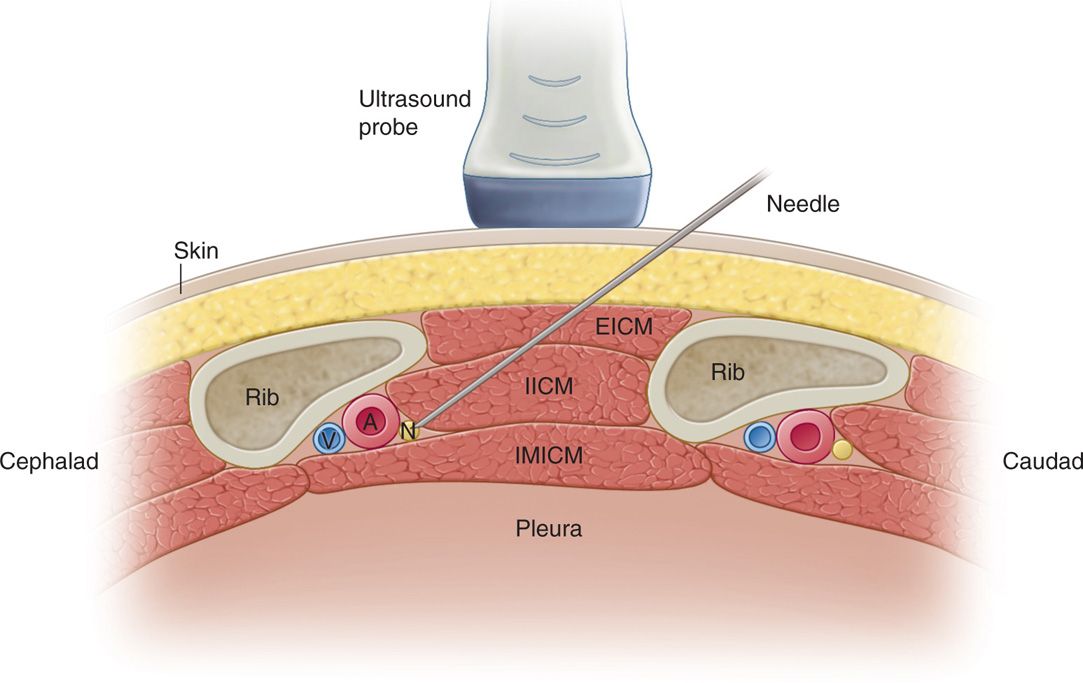
Figure 57-6. Anatomical representation of an intercostal nerve block. Needle entry point and target is shown. EICM, external intercostal muscle; IICM, internal intercostal muscle; IM ICM, innermost intercostal muscle; V-A-N, intercostal vein, artery, and nerve, respectively.
• An in-plane approach for needle placement is recommended.
• Puncture site is initiated from the superior border of the rib below the intercostal nerve of interest (ie, if T6 intercostal nerve is to be blocked, the superior border of T7 rib is the puncture site).
• After local anesthetic is given for skin anesthesia (as above), a 22- or 25-gauge needle is inserted roughly at a 30- to 45-degree angle (Figures 57-7 and 57-8).
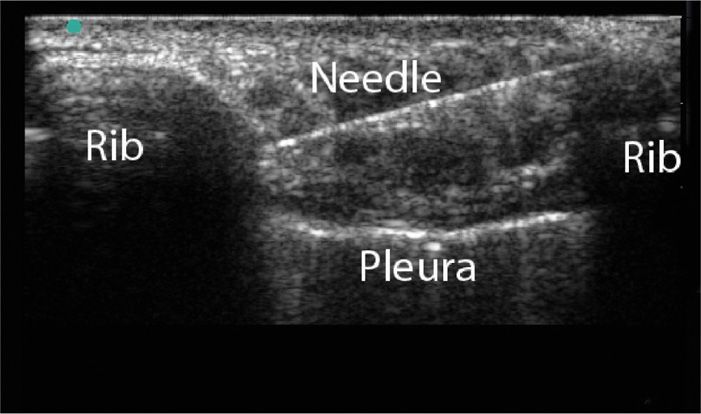
Figure 57-7. Intercostal nerve block under ultrasound guidance with a 22-gauge needle. Notice the needle is easier to visualize when compared to a 25-gauge needle.
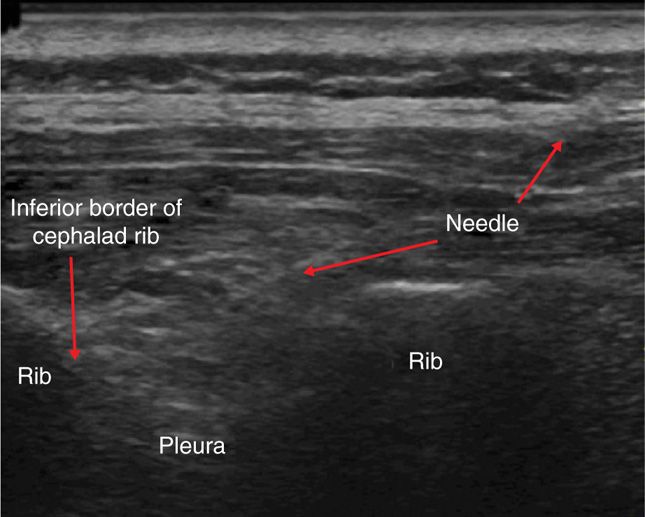
Figure 57-8. Intercostal nerve block under ultrasound guidance with a 25-gauge needle. A 25-gauge needle may be visualized subtly with tissue distraction under real-time view using ultrasonography.
• The needle can be directed to the inferior border of the corresponding rib.
• The needle can penetrate the internal intercostal muscle and can be visualized above the pleura and innermost intercostal muscle.
• Usually the intercostal nerve is not visualized, but the spread of solution beneath the fascia of the internal intercostal muscle signifies a successful blockade of the intercostal nerve.
POSTPROCEDURE FOLLOW-UP AND PITFALLS
After completion of the procedure, evaluation of the patient for side effects should be performed. Of primary concern is the presence of a pneumothorax, which can be detected with a postprocedure chest X-ray. A pulmonary examination may help detect a severe pneumothorax or a tension pneumothorax. Supplemental oxygen may be necessary for mild pneumothorax, while a chest tube may be necessary for symptomatic pneumothorax.
For lower thoracic intercostal nerve blocks, the peritoneum or retroperitoneum may be punctured. Hematoma may be considered if abdominal or back pain ensues over time. Finally, local anesthetic toxicity should be evaluated both for neurologic and cardiac complications, including seizure and arrhythmias.
CLINICAL PEARLS
• Intercostal nerve procedures are indicated for thoracic and abdominal pain and anesthesia.
• Intercostal nerve blocks are contraindicated for patients in which respiratory compromise would lead to severe patient decompensation.
• Utilization of imaging can be used to assist in the placement of the intercostal nerve block.
• Postprocedure evaluation for pneumothorax is warranted.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree